
Pediatrics(2)
.pdf•Onset is usually acute.
•Majority will give a history of a viral infec3on in the preceding 1-4 weeks
•Spectrum of bleeding severity ranges from cutaneous bleeding
-i.e. petechiae, to mucosal bleeds i.e. gum bleeds and epistaxis, to
life threatening bleeds i.e. intracranial haemorrhage.
Diagnosis and Investigations
•Diagnosis is based on history, physical examination, blood counts, and examination of the peripheral blood smear.
•Physical examination: absence of hepatosplenomegaly or lymphadenopathy.
•Blood counts: isolated thrombocytopenia, with normal haemoglobin and white cell count.
•Peripheral blood picture: normal apart from reduced, larger platelets, no abnormal cells.
•Threshold for performing a bone marrow aspiration is low and is indicated:
•Before starting steroid therapy (to avoid partially inducing an undiagnosed acute leukaemia).
•If there is failure to respond to Immunoglobulin therapy.
•When there is persistent thrombocytopenia > 6 months.
•Thrombocytopenia recurs after initial response to treatment.
-• Other tests that may be indicated when there is atypical
presentation are: Antinuclear factor and DNA antibodies.
•Coomb’s test.
•CMV serology for those less than a year old.
•Coagulation profile for those suspected non-accidental injury and inherited bleeding disorder.
•HIV testing for those at risk i.e. parents who are HIV positive or intravenous drug users.
-• Immunoglobulin levels for those with recurrent infections.
-
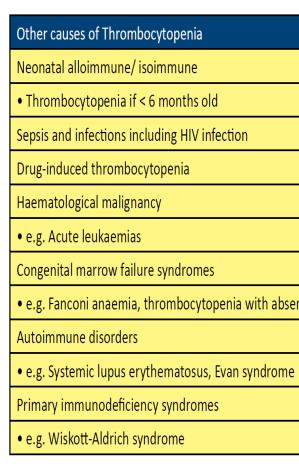
-Differential diagnosis: (ITP is a diagnosis of exclusion)
-- Systemic Lupus Erythematosus (SLE),
-- HIV infection
-- Wiskott-Aldrich Syndrome (WAS)) must be considered in young males found to have low platelet counts, particularly if there is a history of eczema and recurrent infection.
Management
•Not all children with diagnosis of acute ITP need hospitalization.
•Hospitalization is indicated if:
•There is severe life-threatening bleeding (e.g. ICH) regardless of platelet count.
•Platelet count < 10 x 109/L with evidence of bleeding.
•Platelet count < 10 x 109/L without bleeding but inaccessible to health care.
•Parents request due to lack of confidence in homecare.
•Most children remit spontaneously: 70% achieve a platelet count > 50 x 10^9/L by the end of the 3rd week. Treatment should be individualised.
•Precautions with physical activities, avoidance of contact sports and seeking immediate medical attention if bleeding occurs should be advised.
•Careful observation and monitoring of platelet count, without specific treatment, is appropriate for patients with:
•Platelet count > 10 x 109/L without bleeding.
•Platelet count > 30 x 109/L with only cutaneous purpura.
•A repeat blood count should be performed within the first 7-10 days to ensure that there is no evidence of serious evolving marrow condition.
•Treatment is indicated if there is:
•Life threatening bleeding episode ( e.g. ICH) regardless of platelet count.
•Platelet count < 10 x 109/L with mucosal bleeding.
-• Platelet count < 10 x 109/L with any bleeding.
•Choice of treatment includes:
•Oral Prednisolone 1 mg/kg/day for 14 days then taper off.
•Oral Prednisolone 4 mg/kg/day for 4 days.
•IV Immunoglobulin (IVIG) 0.8 g/kg/dose for a single dose.
Notes regarding treatment:
•All above are effective in raising platelet count much quicker compared to no treatment. However there is no evidence that these treatment
regimens reduce bleeding complications or mortality or influence progression to chronic ITP.
•Side effects of IVIG are common (15 - 75%): fever, flushing, headache, nausea, aseptic meningitis and transmission of Hepatitis C (older
preparations).
•Steroids should not be continued if there is no response or if there is a rapid relapse after withdrawal. The long-term side-effects in a growing
child outweigh the benefits of either frequent high-dose pulses or titration of platelet count against a regular lower steroid dose.
•Treatment should not be directed at increasing the platelet count above a preset level but rather on the clinical status of the patient (treat the child
and not the platelet count).
Intracranial Haemorrhage (ICH)
•The most feared complication of ITP.
•Incidence of ICH in a child with ITP is very low between 0.1 - 0.5%.
•The risk of ICH highest with platelet count < 10 x 109/L, history of head trauma, aspirin use and presence of cerebral arteriovenous malformation.
•50% of all ICH occurs aQer 1 month of presenta3on, 30% aQer 6 months.
•Early treatment with steroid or IVIG may not prevent late onset ICH.
Emergency treatment
Emergency treatment of ITP with severe bleeding i.e. severe epistaxis or GIT bleed causing drop in Hb or ICH (alone or in combination) includes:
•High dose IV Methylprednisolone 30 mg/kg/day for 3 days.
•IVIG 0.8g - 1g/kg as a single dose.
•Combination of IVIG and methylprednisolone in life threatening conditions.
•Platelet transfusion in life threatening haemorrhage: 8 - 11 units/m1 body surface area (1 to 3 folds larger than usual units) as the platelets will be
consumed by the haemorrhage to form blood clots and will reduce further circulating platelets.
• Consider emergency splenectomy if other modalities fail.
-• Neurosurgical intervention in ICH, if indicated and to perform with splenectomy if necessary.
-Note MANAGEMENT: (for newborns, see national neonatology protocols)
CHRONIC ITP
Definition
•Persistent thrombocytopenia aQer 6 months of onset (occurs in 10%)
•Wide spectrum of manifestations: mild asymptomatic low platelet counts to intermittent relapsing symptomatic thrombocytopenia to the rare
stubborn and persistent symptomatic and haemorrhagic disease.
Management
Counselling and education of patient and caretakers regarding natural history of disease and how to detect problems and possible complications early are important. Parents should be comfortable of taking
care of patients with persistent low platelet counts at home. At the same time they must be made aware of when and how to seek early medical attention when the need arises.
•Every opportunity should be given for disease to remit spontaneously as the majority will do so if given enough time.
•Revisit diagnosis to exclude other causes of thrombocytopenia (Immunodeficiency, lymphoproliferative, collagen disorders, HIV infection).
•Asymptomatic children can be left without therapy and kept under observation with continued precautions during physical activity.
•Symptomatic children may need short course of treatments as for acute ITP to tide them over the “relapse” period or during surgical procedures.

For those with Persistent bleeding, Second line therapies includes:
•Pulses of steroids: oral Dexamethasone 1 mg/kg given on 4 consecu3ve days every 4 weeks for 4 months.
•Intermittent anti-Rh(D) Immunoglobulin treatment for those who are Rhesus D posi3ve: 45 - 50 ug/kg. May cause drop in Hb levels.
•Second line therapy should only be started after discussion with a Paediatric haematologist.
Note:
•Care must be taken with any pulse steroid strategy to avoid treatmentrelated steroid side effects.
•Family and patient must be aware of immunosuppressive complications e.g. risk of severe varicella.
•There is no justification for long-term continuous steroids.
If first and second-line therapies fail, the patient should be managed by a paediatric haematologist.
Other useful agents are Rituximab and Cyclosporine.
Splenectomy
•Rarely indicated in children as spontaneous remissions continue to occur up to 15 years from diagnosis.
•The risk of dying from ITP is very low - 0.002% whilst the mortality associated with post-splenectomy sepsis is higher at 1.4 - 2.7 %.
•Justified when there is:
•Life-threatening bleeding event
•Severe life-style restriction with no or transient success with intermittent IVIG, pulsed steroids or anti-D immunoglobulin.
•Laparoscopic method preferred if expertise is available.
•Pre-splenectomy preparation of the child with immunization against pneumococcus, haemophilus and meningocccus must be done and postsplenectomy life-long penicillin prophylaxis must be ensured.
•Pneumococcal booster should be given every 5 years.
•7p to ;CO of pa3ents achieve complete remission post-splenectomy.
