
Essentials of Orthopedic Surgery, third edition / 12-The Knee
.pdf
12
The Knee
BRIAN G. EVANS
This chapter discusses the anatomy, biomechanics, and pathology of the knee. The function of the knee is provided primarily by the soft tissue. Therefore, injury to these soft tissue structures has significant impact upon the stability of the knee.
Anatomy
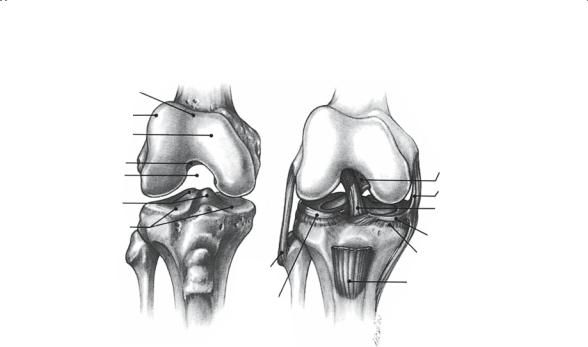
The osseous anatomy of the knee consists of the proximal tibia, distal femur, and the patella (Fig. 12-1). The distal femur consists of the medial and lateral condyles, the medial and lateral epicondyles, the femoral trochlear groove, and the intercondylar notch. The medial condyle is larger and extends slightly distal compared to the lateral condyle. Both condyles are covered with articular cartilage. The trochlear groove lies on the anterior aspect of the distal femur between the medial and lateral femoral condyles. This surface is also covered by articular cartilage and serves as the site of articulation of the patella. The lateral rim of the trochlear groove is frequently more prominent than the medial side to allow for proper patellar tracking along the femur.
The epicondyles serve as the site of insertion of several important structures. The deep and superficial medial collateral ligaments (MCL) attach to the medial epicondyle. The proximal margin of the medial epicondyle is enlarged and serves as the site of insertion of the adductor magnus (the adductor tubercle). The lateral or fibular collateral ligament (LCL) attaches to the lateral epicondyle. Inferior to the attachment of the LCL is the insertion of the popliteal muscle at the junction of the lateral condyle and epicondyle. The medial and lateral heads of the gastrocnemius muscle originate from the medial and lateral posterior femoral condyles. The intercondylar notch is the site of the femoral attachment of the cruciate ligaments. The anterior cruciate ligament (ACL) attaches in the posterolateral aspect of the notch, and the posterior cruciate ligament (PCL) attaches in the anteromedial aspect of the notch.
454
|
12. The Knee |
455 |
|
Femoral (trochlear) |
|
|
|
groove |
|
|
|
Lateral condyle |
|
|
|
Medial condyle |
|
|
|
Grant’s notch |
Posterior cruciate |
||
Intercondylar |
|||
ligament |
|
||
notch |
|
Deep medial |
Tibial spines |
|
collateral ligament |
|
Anterior cruciate |
|
|
|
|
Tibial plateaus |
|
ligament |
|
Medial meniscus |
|
|
|
|
|
|
Coronary ligament |
|
Lateral |
|
|
collateral |
Patellar tendon |
|
ligament |
|
|
|
|
|
Lateral |
|
|
meniscus |
|
FIGURE 12-1. Bony anatomy and major ligamentous structures of the flexed knee joint (anterior view).
The proximal tibial surface is composed of the medial and lateral plateaus and the intercondylar eminence. The medial plateau is larger and extends further posterior compared to the lateral plateau. The surface of the medial plateau is relatively flat. The lateral tibial plateau is, in fact, slightly convex. Both the tibial plateaus are covered with articular cartilage. The intercondylar eminence is the site of attachment menisci and the cruciate ligaments.
The patella is a sesamoid bone within the tendon of the quadriceps mechanism. There are two major facets on the patella, the medial and lateral facets. There is significant variability in the size and orientation of these facets. However, normally the lateral facet is broader and the medial facet is more acutely oriented to the femoral trochlea.
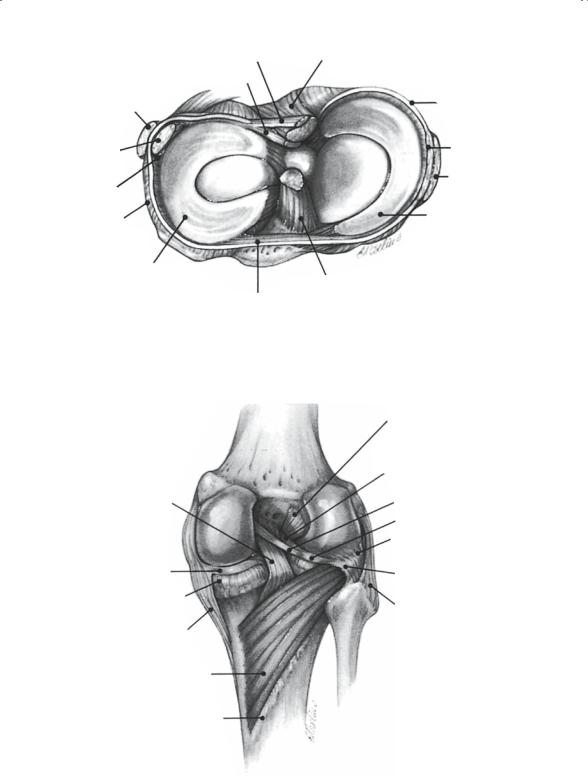
The osseous anatomy of the knee provides little to the stability of the knee. Stability and function are therefore provided by the complex soft tissue envelope around and in the knee (Figs. 12-2, 12-3). The soft tissue components of the knee can be divided into several components: static restraints (ligaments), dynamic restraints (muscles and tendons), and the menisci. The static restraints are represented by the medial collateral ligament (MCL), lateral collateral ligament (LCL), anterior cruciate ligament (ACL), and posterior cruciate ligament (PCL). These structures resist valgus and varus stress as well and anterior and posterior translation of the
Ligament of Wrisberg |
Posterior cruciate |
Ligament of Humphry |
ligament |
|
|
Lateral collateral |
Capsule |
ligament |
Deep medial |
|
|
Popliteal |
collateral |
ligament |
|
tendon |
Superficial |
|
|
Popliteal |
medial |
hiatus |
collateral |
(recess) |
ligament |
Coronary |
Medial meniscus |
ligament |
|
(meniscotibial) |
|
Lateral meniscus
Anterior cruciate
Transverse ligament ligament
FIGURE 12-2. Cross section of the knee demonstrating the menisci and associated ligaments.
|
Anterior cruciate |
|
ligament |
|
Anterior |
|
meniscofemoral ligament |
|
(ligament of Humphry) |
|
Posterior |
|
meniscofemoral ligament |
Posterior cruciate |
(ligament of Wrisberg) |
ligament |
Lateral meniscus |
|
|
|
Popliteus tendon |
|
(under arcuate ligament) |
Medial meniscus |
Arcuate ligament |
Coronary ligament |
|
(meniscotibial ligament) |
Lateral collateral |
|
|
|
ligament |
Superficial medial |
|
collateral ligament |
|
Popliteus muscle |
|
Soleal line |
|
FIGURE 12-3. Posterior aspect of the knee joint.

12. The Knee |
457 |
tibial relative to the femur. The MCL consists of two layers. The deep MCL spans from the medial epicondyle of the femur to the proximal tibial border just below the medial tibial plateau. The superficial MCL has the same femoral origin; however, the ligament has a broad tibial insertion extending 6 to 10 cm below the tibial plateau along the posteromedial border of the tibia. The LCL is a more-discrete band along the lateral aspect of the knee. It spans from the lateral epicondyle to the fibular head.
The anterior cruciate ligament resists the anterior translation of the tibia relative to the femur. The ligament runs from the anterior aspect of the tibial eminence to the posterolateral aspect of the femoral notch. The posterior cruciate ligament resists posterior translation of the tibia relative to the femur and resists hyperextension of the knee. The ligament extends from the posterior aspect of the intercondylar eminence and proximal tibia in the midline to the anteromedial aspect of the femoral intercondylar notch.
The dynamic restraints in the knee are the muscles and tendons that cross the knee joint. These muscles are broadly divided into those that act to extend the knee and those which act to flex the knee. The extensor muscles are the quadriceps femoris and the tensor fascia lata. The quadriceps is a group of four muscles, all inserting onto the patella and patellar tendon, which in turn inserts on the anterior tibial tubercle. The muscles that make up the quadriceps are the rectus femoris, vastus lateralis, vastus medialis, and vastus intermedius; these are all supplied by the femoral nerve. The tensor fascia lata originates on the pelvic brim and inserts at Gerdy’s tubercle on the proximal anterior lateral tibia. The tensor fascia lata is innervated by the superior gluteal nerve.
The primary flexors of the knee are the hamstring muscles—the semimembranosus, semitendinosus, and the biceps femoris—and the sartorius and gracilis. The hamstring muscles originate on the ischium and insert on the posteromedial and posterolateral proximal tibia. They receive their innervation from the sciatic nerve; all are innervated by the tibial division of the sciatic nerve, except the short head of the biceps, which is innervated by the peroneal division of the sciatic nerve. The sartorius originates from the anterosuperior iliac spine and the gracilis originates from the pubis. Both these muscles with the semitendinosus insert into the proximal medial tibia in the pes anserine (goose’s foot, relating to the appearance of the three tendons inserting together). The sartorius is innervated by the femoral nerve and the gracilis by the obturator nerve.
The other muscles that serve to flex the knee are the gastrocnemius and popliteus, which extend from the posterior aspect of the femoral condyles to the calcaneus and proximal tibia, respectively.
The menisci are two crescent-shaped cartilaginous structures attached to the proximal tibial surface. These structures serve two purposes in the knee. They increase the surface area for weight-bearing, therefore reducing the peak stress in the articular cartilage, and they also provide a small

458 B.G. Evans
degree of stability to the knee by changing the flat tibial articular surface to a cupped surface. The menisci are composed of dense organized cartilage tissue.
Biomechanics of the Knee
The mechanical axis of the lower extremity extends from the center of rotation of the hip to the center of the ankle joint. This axis normally crosses the knee joint in the lateral third of the medial tibial plateau. The normal anatomic alignment of the knee is in 7 degrees of valgus. When the knee is loaded, the medial compartment experiences 60% and the lateral compartment 40% of the weight-bearing stress. This difference in the applied load in the normal knee is the reason the medial tibial plateau and medial femoral condyle are larger than the lateral side. Patients with significant angular deformity in the knee have altered weight-bearing, which results in increased stress in the medial (with varus or bowlegged deformity) or lateral (with valgus or knock-knee deformity) compartment. The increased stress frequently results in early arthritis in the overused compartment of the knee.
The highest joint forces, however, are found in the patellofemoral articulation. Forces as high as fiveto eightfold body weight can be noted for activities such as stair climbing and jumping. The function of the patella has been controversial; however, most now recognize the role of the patella in providing a mechanical advantage to the quadriceps tendon. The patella moves the line of pull of the quadriceps further away from the center of rotation, therefore acting as a lever and reducing the force required to extend the knee. Patients who have had the patella removed because of arthritis or trauma are noted to have approximately 30% reduction in the force in the quadriceps compared to patients with a patella.
Evaluation of the Painful Knee
History
The history should begin with the chief complaint and how long the patient has noticed the problem. The specific location of pain, any radiation, the nature of the pain (ache, burning, stabbing, etc.), and any exacerbating or ameliorating factors are included. In particular, the relationship of the pain to activity and rest are important to note. Commonly, pain in the musculoskeletal system is relieved with rest. Severe pain that is present at rest suggests a septic process or neoplasm, which may be primary or metastatic.
Knee problems frequently begin with an injury. A detailed history describing the injury can be very helpful in determining the structures that are injured. The nature of any external force contacting the knee and the

12. The Knee |
459 |
position of the knee at the time of injury should be elicited. Did an audible or palpable pop occur at the time of the injury? Shifting or abnormal movement of the knee may also have been noted at the time of injury. The degree and nature of any swelling around the knee is important to record. In addition to a description of the injury, it is helpful to inquire about the patient’s ability to use the knee after the injury: Was the patient able to weight-bear? Was the onset of pain or swelling immediate or delayed? Could the patient flex or extend the knee after injury? These are important questions to ask the patient after a knee injury.
In addition to pain, patients with knee problems complain of mechanical problems in the knee. Patients may note an inability to fully bend or straighten the knee, which is referred to as locking of the knee. Locking can be a result of a loose body in the knee becoming lodged between the femoral condyle and tibial plateau, similar to a wedge “doorstop.” The patients who note intermittent locking of the knee are usually able to relieve the locked knee by gently moving the knee without weight-bearing. This maneuver allows the loose fragment to be released from between the femur and tibia, and motion will be restored. However, inability to fully flex and extend the knee can also be noted in patients with large effusions and in patients with ligament injuries.
Instability is another frequent complaint of patients with knee injuries. Patients observe that their knee shifts or buckles with particular activities. Instability can result from two general etiologies. The first are ligamentous injuries. As noted previously, the stability of the knee is a result of the ligaments that cross from the tibia to the femur. Disruption of the ligaments will result in alteration of knee function; the knee may shift or sublux with activity. The second common cause of a knee buckling or giving-way are problems in the patellofemoral joint. Instability of the patella in the trochlear groove will result in a giving-way sensation as the patella subluxes. Damage to the articular surfaces of the patella or the trochlear groove will result in pain as the patella tracks over the trochlea; this can occasionally lead to a sharp acute pain that leads to the quadriceps releasing its contraction while the patient is weight-bearing on the leg as a result of a primitive reflex arc. The patient notes a giving-way or buckling sensation in the knee, and a few patients may actually fall as a result.
The majority of knee complaints are aggravated by activities. The specific problems the patient has encountered are important to note. Patients commonly have difficulty ascending and descending stairs. Frequently, descending stairs will be the most symptomatic as this places high stress across the patellofemoral joint. Bicycling can also aggravate the patellofemoral joint. Activities that involve quadriceps contraction with the knee in flexion may result in subluxation in patients with patellar instability. Patients with meniscal tears have difficulty squatting and may notice snapping or pain when rising from a chair or ascending stairs. Activities that involve stopping and turning or cutting will result in the knee

460 B.G. Evans
shifting or giving-way if there is insufficiency in the collateral or cruciate ligaments.
Physical Examination
Physical examination of the patient with a knee complaint begins with inspection. Observation of the alignment of the lower extremity should demonstrate a normal 7 degree valgus (knock-knee) angle at the knee when a patient is standing. Deformity of the leg in varus or valgus beyond 7 degrees can be associated with either a ligamentous or osseous deficiency. Any swelling, bruising, or ecchymosis should be recorded.
Next, the evaluation should focus on the patient’s gait. Normal gait involves range of motion from 0 to 65 degrees of flexion. The gait should have a smooth cadence, with the length of each step being equal on the left and right sides. The knee should not demonstrate any sudden shift to either the lateral or medial side. If abnormal lateral motion is noted, this is recorded as a medial or lateral thrust.
The knee should then be examined with the patient sitting with the legs over the edge of the examining table. The position of the patella should be anterior and symmetrical. The patellar tracking can then be followed by asking the patient to flex and extend the knee with the examiner palpating the patella. There should be little lateral movement. Crepitus may also be noted as a grinding sensation between the patella and the femoral trochlear groove.
The knee should then be examined with the patient supine. For all aspects of the examination, the contralateral knee can be used as a normal control. Effusion or fluid within the knee can be assessed by placing both hands on the knee, with one below the patella and one above the patella. Any fluid in the knee can then be displaced and palpated proximally and distally. The knee can be palpated to determine the specific site of maximum tenderness. The range of motion of the knee is measured with the knee in straight extension as 0 degrees of flexion; normal full flexion is approximately 135 degrees.
The collateral ligaments are then assessed by stabilizing the thigh with one hand and placing a varus or valgus stress on the knee with the other hand. A normal knee has a small amount of medial and lateral laxity in the collateral ligaments. However, any laxity that is excessive, or causes pain to be elicited, should be noted. The cruciate ligaments can also be assessed. The anterior cruciate ligament is best assessed using the Lachman test. The examiner stands by the patient’s feet and stabilizes the femur with one hand holding the distal medial thigh. The tibia is held with a thumb at the lateral joint line. The examiner then attempts to displace the tibia forward in relation to the femur. Translation less than 5 mm should be noted, and the anterior cruciate ligament should be felt to “snap taut.” Injury to the posterior cruciate ligament can be demonstrated by noting
12. The Knee |
461 |
the degree of recurvatum (back-knee), which can be obtained passively compared to the contralateral knee. Also, with both knees flexed 60 to 90 degrees and the patient supine, the tibia on the deficient side will be noted to sag posteriorly compared to the uninjured leg when viewed from the side. Comparison to the contralateral knee is very important for examination of the collateral and cruciate ligaments.
The menisci are examined by palpation of their outer margin along the joint line at the proximal tibial articular surface. In addition, meniscal tears can be detected by the McMurray maneuver; this is done by flexing the knee internally and externally rotating the tibia and then extending the knee with a valgus force applied. If a reproducible snap is palpated or pain elicited at the joint line, this is suggestive of a tear. Patients with meniscal tears also report pain when asked to squat down with the knees flexed.
Imaging
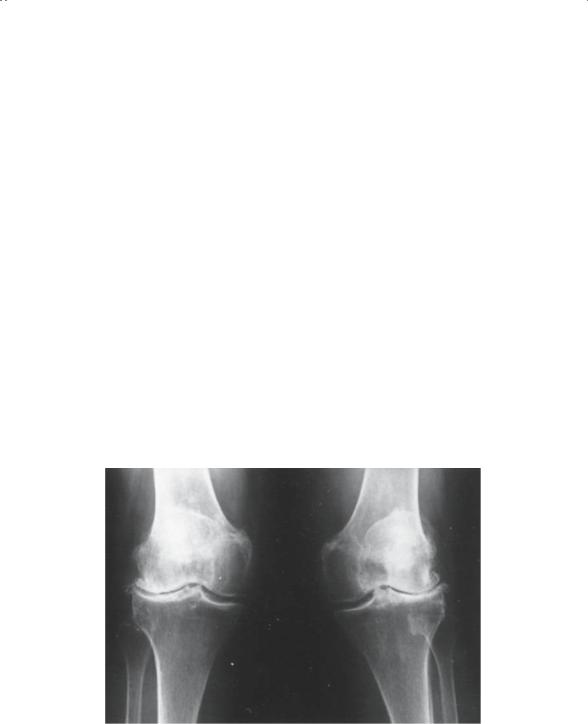
All the available imaging techniques have been utilized in the evaluation of patients with knee problems. Plain radiographs are the most commonly obtained studies (Fig. 12-4). Plain radiographs are helpful in the evaluation of fractures and subluxation of the joint; in addition, the condition of the articular surfaces can be investigated. The standard series of routine X-
FIGURE 12-4. Standing anteroposterior (AP) radiograph of both knees in a 70- year-old woman with osteoarthritis of both knees with a valgus (knock-knee deformity) of both knees. Note the asymmetrical space between the medial and lateral femoral condyles and the tibial surface.
462 B.G. Evans
rays of the knee should include a standing anteroposterior (AP) radiograph of both knees, a lateral view and a merchant or “sunrise view.” The sunrise view is a view taken with the knee in 45 degrees of flexion with the beam directed inferiorly and parallel to the patellar articular surface. There should be a space of 5 to 10 mm between the end of the femoral condyles and the tibial surface and beneath the patellar surface and the femoral trochlea. This “clear space” is in fact occupied by articular cartilage.
R19
A
B
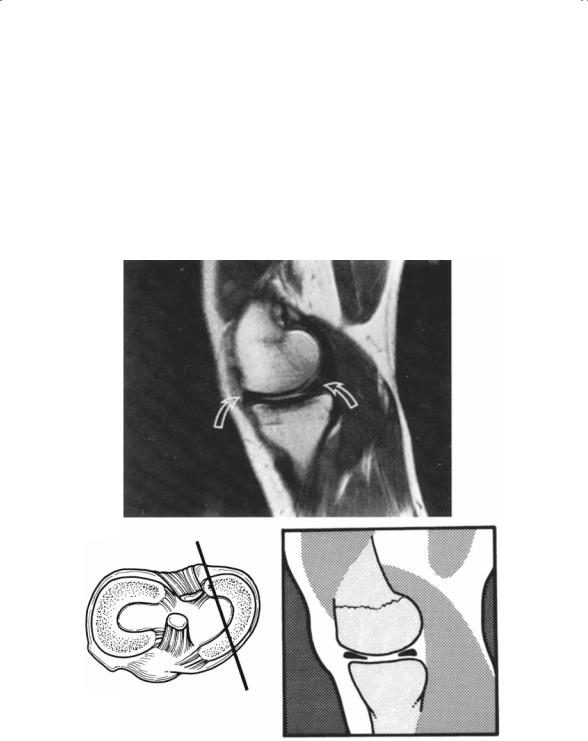
FIGURE 12-5. (A) Normal T1-weighted magnetic resonance imaging (MRI) sagittal image of the medial meniscus. (B) Schematic illustration showing the section cut of (A).

12. The Knee |
463 |
Routine radiography is an excellent tool for the evaluation of the knee for trauma, arthritis, and alignment. Plain radiographs, however, only demonstrate the osseous structures. As mentioned earlier, the soft tissues provide the stability and allow the knee to function. Arthrography has been used in the past to evaluate the knee for meniscal pathology. However, this technique is inaccurate and invasive. The development of arthroscopy is a technique that allows the direct visualization of the structures within the knee with a minor surgical procedure. However, this technique is also invasive, and although arthroscopy is accurate, the procedure is relatively expensive compared to an imaging modality alone. Nuclear medicine studies are of limited use in the knee. These studies are sensitive; however, the specificity of these studies is limited. Magnetic resonance imaging (MRI) has provided a dramatic step forward in our ability to diagnose soft tissue injury to the knee. MRI provides accurate and noninvasive evaluation of all the soft tissue structures within the knee (Fig. 12-5). MRI is currently the study of choice for the evaluation of intraarticular pathology within the knee.
Knee Pathology
Soft tissue injury is common in the knee. A knee with a bloody effusion after an injury has an incidence as high as 80% of significant soft tissue injury. The differential diagnosis of a posttraumatic bloody effusion in the absence of an intraarticular fracture are meniscal tear, ACL tear, or a patellar dislocation.
Meniscal Tears
Tears of the meniscus can occur in two settings. One is as the result of a specific injury, which usually involves a twisting injury with the knee in some flexion. Swelling and pain are noted immediately after the injury. There is increased pain with attempts at movement, and there is a limitation in the range of motion. Pain with squatting down or arising from a chair is commonly reported. The torn meniscus can block motion. Occasionally the knee can be gently manipulated to reduce the torn meniscal fragment, and motion will be restored. However, the fragment will frequently redisplace, and intermittent locking may occur. This form of a tear is usually in younger patients with stout meniscal tissue.
In older individuals, the meniscal tissues soften and the edge becomes frayed. As this occurs, the frayed edges can become entrapped between the edges of the bone, initiating a tear that can extend into the meniscal substance. This tear can occur with little or no trauma with minimal swelling and pain initially. The diagnosis is made by joint line pain, effusion, and rarely locking. Patients with locking frequently require arthroscopic
