
- •Global Impact
- •Epidemics and Pandemics
- •Current Situation
- •Individual Impact
- •The Virus
- •Requirements for Success
- •Virology
- •Natural Reservoir + Survival
- •Transmission
- •H5N1: Making Progress
- •Individual Management
- •Epidemic Prophylaxis
- •Exposure Prophylaxis
- •Vaccination
- •Antiviral Drugs
- •Epidemic Treatment
- •Pandemic Prophylaxis
- •Pandemic Treatment
- •Global Management
- •Epidemic Management
- •Pandemic Management
- •Containment
- •Drugs
- •Vaccines
- •Distribution
- •Conclusion
- •Golden Links
- •Interviews
- •References
- •Avian Influenza
- •The Viruses
- •Natural hosts
- •Clinical Presentation
- •Pathology
- •LPAI
- •HPAI
- •Differential Diagnosis
- •Laboratory Diagnosis
- •Collection of Specimens
- •Transport of Specimens
- •Diagnostic Cascades
- •Direct Detection of AIV Infections
- •Indirect Detection of AIV Infections
- •Transmission
- •Transmission between Birds
- •Poultry
- •Humans
- •Economic Consequences
- •Control Measures against HPAI
- •Vaccination
- •Pandemic Risk
- •Conclusion
- •References
- •Structure
- •Haemagglutinin
- •Neuraminidase
- •M2 protein
- •Possible function of NS1
- •Possible function of NS2
- •Replication cycle
- •Adsorption of the virus
- •Entry of the virus
- •Uncoating of the virus
- •Synthesis of viral RNA and viral proteins
- •Shedding of the virus and infectivity
- •References
- •Pathogenesis and Immunology
- •Introduction
- •Pathogenesis
- •Viral entry: How does the virion enter the host?
- •Binding to the host cells
- •Where does the primary replication occur?
- •How does the infection spread in the host?
- •What is the initial host response?
- •Cytokines and fever
- •Respiratory symptoms
- •Cytopathic effects
- •Symptoms of H5N1 infections
- •How is influenza transmitted to others?
- •Immunology
- •The humoral immune response
- •The cellular immune response
- •Conclusion
- •References
- •Pandemic Preparedness
- •Introduction
- •Previous Influenza Pandemics
- •H5N1 Pandemic Threat
- •Influenza Pandemic Preparedness
- •Pandemic Phases
- •Inter-Pandemic Period and Pandemic Alert Period
- •Surveillance
- •Implementation of Laboratory Diagnostic Services
- •Vaccines
- •Antiviral Drugs
- •Drug Stockpiling
- •General Measures
- •Seasonal Influenza Vaccination
- •Political Commitment
- •Legal and Ethical Issues
- •Funding
- •Global Strategy for the Progressive Control of Highly Pathogenic Avian Influenza
- •Pandemic Period
- •Surveillance
- •Treatment and Hospitalisation
- •Human Resources: Healthcare Personnel
- •Geographically Targeted Prophylaxis and Social Distancing Measures
- •Tracing of Symptomatic Cases
- •Border Control
- •Hygiene and Disinfection
- •Risk Communication
- •Conclusions
- •References
- •Introduction
- •Vaccine Development
- •History
- •Yearly Vaccine Production
- •Selection of the yearly vaccine strain
- •Processes involved in vaccine manufacture
- •Production capacity
- •Types of Influenza Vaccine
- •Killed vaccines
- •Live vaccines
- •Vaccines and technology in development
- •Efficacy and Effectiveness
- •Side Effects
- •Recommendation for Use
- •Indications
- •Groups to target
- •Guidelines
- •Contraindications
- •Dosage / use
- •Inactivated vaccine
- •Live attenuated vaccine
- •Companies and Products
- •Strategies for Use of a Limited Influenza Vaccine Supply
- •Antigen sparing methods
- •Rationing methods and controversies
- •Pandemic Vaccine
- •Development
- •Mock vaccines
- •Production capacity
- •Transition
- •Solutions
- •Strategies for expediting the development of a pandemic vaccine
- •Enhance vaccine efficacy
- •Controversies
- •Organising
- •The Ideal World – 2025
- •References
- •Useful reading and listening material
- •Audio
- •Online reading sources
- •Sources
- •Laboratory Findings
- •Introduction
- •Laboratory Diagnosis of Human Influenza
- •Appropriate specimen collection
- •Respiratory specimens
- •Blood specimens
- •Clinical role and value of laboratory diagnosis
- •Patient management
- •Surveillance
- •Laboratory Tests
- •Direct methods
- •Immunofluorescence
- •Enzyme immuno assays or Immunochromatography assays
- •Reverse transcription polymerase chain reaction (RT-PCR)
- •Isolation methods
- •Embryonated egg culture
- •Cell culture
- •Laboratory animals
- •Serology
- •Haemagglutination inhibition (HI)
- •Complement fixation (CF)
- •Ezyme immuno assays (EIA)
- •Indirect immunofluorescence
- •Rapid tests
- •Differential diagnosis of flu-like illness
- •Diagnosis of suspected human infection with an avian influenza virus
- •Introduction
- •Specimen collection
- •Virological diagnostic modalities
- •Other laboratory findings
- •New developments and the future of influenza diagnostics
- •Conclusion
- •Useful Internet sources relating to Influenza Diagnosis
- •References
- •Clinical Presentation
- •Uncomplicated Human Influenza
- •Complications of Human Influenza
- •Secondary Bacterial Pneumonia
- •Primary Viral Pneumonia
- •Mixed Viral and Bacterial Pneumonia
- •Exacerbation of Chronic Pulmonary Disease
- •Croup
- •Failure of Recovery
- •Myositis
- •Cardiac Complications
- •Toxic Shock Syndrome
- •Reye’s Syndrome
- •Complications in HIV-infected patients
- •Avian Influenza Virus Infections in Humans
- •Presentation
- •Clinical Course
- •References
- •Treatment and Prophylaxis
- •Introduction
- •Antiviral Drugs
- •Neuraminidase Inhibitors
- •Indications for the Use of Neuraminidase Inhibitors
- •M2 Ion Channel Inhibitors
- •Indications for the Use of M2 Inhibitors
- •Treatment of “Classic” Human Influenza
- •Antiviral Treatment
- •Antiviral Prophylaxis
- •Special Situations
- •Children
- •Impaired Renal Function
- •Impaired Liver Function
- •Seizure Disorders
- •Pregnancy
- •Treatment of Human H5N1 Influenza
- •Transmission Prophylaxis
- •General Infection Control Measures
- •Special Infection Control Measures
- •Contact Tracing
- •Discharge policy
- •Global Pandemic Prophylaxis
- •Conclusion
- •References
- •Drug Profiles
- •Amantadine
- •Pharmacokinetics
- •Toxicity
- •Efficacy
- •Resistance
- •Drug Interactions
- •Recommendations for Use
- •Warnings
- •Summary
- •References
- •Oseltamivir
- •Introduction
- •Structure
- •Pharmacokinetics
- •Toxicity
- •Efficacy
- •Treatment
- •Prophylaxis
- •Selected Patient Populations
- •Efficacy against Avian Influenza H5N1
- •Efficacy against the 1918 Influenza Strain
- •Resistance
- •Drug Interactions
- •Recommendations for Use
- •Summary
- •References
- •Rimantadine
- •Introduction
- •Structure
- •Pharmacokinetics
- •Toxicity
- •Efficacy
- •Treatment
- •Prophylaxis
- •Resistance
- •Drug Interactions
- •Recommendations for Use
- •Adults
- •Children
- •Warnings
- •Summary
- •References
- •Zanamivir
- •Introduction
- •Structure
- •Pharmacokinetics
- •Toxicity
- •Efficacy
- •Treatment
- •Prophylaxis
- •Children
- •Special Situations
- •Avian Influenza Strains
- •Resistance
- •Drug Interactions
- •Recommendations for Use
- •Dosage
- •Summary
- •References
Zanamivir 213
19.Hayden FG, Belshe RB, Clover RD, Hay AJ, Oakes MG, Soo W. Emergence and apparent transmission of rimantadine-resistant influenza A virus in families. N Engl J Med 1989; 321: 1696-702. Abstract: http://amedeo.com/lit.php?id=2687687
20.Hayden FG, Sperber SJ, Belshe RB, Clover RD, Hay AJ, Pyke S. Recovery of drugresistant influenza A virus during therapeutic use of rimantadine. Antimicrob Agents Chemother 1991; 35: 1741-7. Abstract: http://amedeo.com/lit.php?id=1952841
21.Holazo AA, Choma N, Brown SY, Lee LF, Wills RJ. Effect of cimetidine on the disposition of rimantadine in healthy subjects. Antimicrob Agents Chemother 1989; 33: 820-3. Abstract: http://amedeo.com/lit.php?id=2764530 – Full text at http://www.pubmedcentral.gov/articlerender.fcgi?pubmedid=2764530
22.Jefferson T, Deeks JJ, Demicheli V, Rivetti D, Rudin M. Amantadine and rimantadine for preventing and treating influenza A in adults. Cochrane Database Syst Rev 2004; CD001169. Abstract: http://amedeo.com/lit.php?id=15266442
23.Jefferson T, Demicheli V, Rivetti D, Jones M, Di Pietrantonj C, Rivetti A. Antivirals for influenza in healthy adults: systematic review. Lancet 2006; 367: 303-13. Abstract: http://amedeo.com/lit.php?id=16443037
24.Li KS, Guan Y, Wang J, et al. Genesis of a highly pathogenic and potentially pandemic H5N1 influenza virus in eastern Asia. Nature 2004; 430: 209-13. Abstract: http://amedeo.com/lit.php?id=15241415
25.Monto AS, Ohmit SE, Hornbuckle K, Pearce CL. Safety and efficacy of long-term use of rimantadine for prophylaxis of type A influenza in nursing homes. Antimicrob Agents Chemother 1995; 39: 2224-8. Abstract: http://amedeo.com/lit.php?id=8619572 – Full text at http://aac.asm.org/cgi/reprint/39/10/2224
26.Patriarca PA, Kater NA, Kendal AP, Bregman DJ, Smith JD, Sikes RK. Safety of prolonged administration of rimantadine hydrochloride in the prophylaxis of influenza A virus infections in nursing homes. Antimicrob Agents Chemother 1984; 26: 101-3. Abstract: http://amedeo.com/lit.php?id=6476812
27.Stephenson I, Nicholson KG. Influenza: vaccination and treatment. Eur Respir J 2001; 17: 1282-93. Abstract: http://amedeo.com/lit.php?id=11491177 – Full text at http://erj.ersjournals.com/cgi/content/full/17/6/1282
28.Sugrue RJ, Hay AJ. Structural characteristics of the M2 protein of influenza A viruses: evidence that it forms a tetrameric channel. Virology 1991; 180: 617-24. Abstract: http://amedeo.com/lit.php?id=1989386
29.Wills RJ, Belshe R, Tomlinsin D, et al. Pharmacokinetics of rimantadine hydrochloride in patients with chronic liver disease. Clin Pharmacol Ther 1987; 42: 449-54. Abstract: http://amedeo.com/lit.php?id=3665342
30.Wintermeyer SM, Nahata MC. Rimantadine: a clinical perspective. Ann Pharmacother 1995; 29: 299-310. Abstract: http://amedeo.com/lit.php?id=7606077
Zanamivir
Introduction
Zanamivir is an orally inhaled powder currently approved in 19 countries for the treatment of, and in two for the prophylaxis of influenza A and B. Zanamivir is a competitive inhibitor of the neuraminidase glycoprotein, which is essential in the infective cycle of influenza viruses. It closely mimics sialic acid, the natural substrate of the neuraminidase (Varghese 1992, Varghese 1995).
Zanamivir is administered via inhalation, resulting in direct delivery to the respiratory tract, where the concentration has been calculated to be more than 1,000 times as high as the IC50 for neuraminidase. The inhibitory effect starts within 10 seconds.
214 Drug Profiles
When systemic involvement of influenza infection is suspected – as has recently been suggested by some reports on avian H5N1 influenza in humans (de Jong 2005)
– zanamivir might not be the suitable drug.
Over the last few years, a number of events have resulted in changes to the zanamivir prescribing information which now contains warnings of bronchospasm, dyspnoea, rash, urticaria and allergic type reactions, including facial and oropharyngeal oedema. However, apart from these rare episodes, the drug has a good safety profile if begun early (Hayden 1997).
Co-administration of orally inhaled zanamivir with inactivated trivalent influenza vaccine does not seem to adversely affect the production of antihaemagglutinin antibodies (Webster 1999); a protective antibody response develops within 12 days (Cox 2001).
Structure
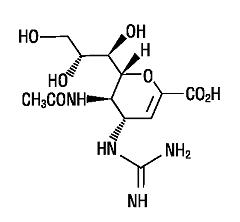
The chemical name of zanamivir is 5-(acetylamino)-4-[(aminoiminomethyl)- amino]-2,6-anhydro-3,4,5-trideoxy-D-glycero-D-galacto-non-2-enonic acid. It has the following structural formula:
Pharmacokinetics
Data on orally inhaled zanamivir indicate that 10-20 % of the active compound reaches the lungs. The rest is deposited in the oropharynx and approximately 4 % to 17 % of the inhaled dose is systemically absorbed. The peak serum concentrations are reached within 1 to 2 hours following a 10 mg dose. Plasma protein binding is limited (< 10 %). Zanamivir is excreted unchanged in the urine with the excretion of a single dose completed within 24 hours (Cass 1999b). The serum half-life of zanamivir after administration by oral inhalation ranges from 2.5 to 5.1 hours.
Studies have demonstrated that intravenously administered zanamivir is distributed to the respiratory mucosa and is protective against infection and illness following experimental human influenza A virus inoculation (Calfee 1999).
Zanamivir 215
Toxicity
Zanamivir has a good safety profile and the overall risk of occurrence of any respiratory event is low (Loughlin 2002). Results from in vitro and in vivo animal studies suggest that zanamivir has low acute toxicity and no significant systemic toxicity or respiratory tract irritancy at plasma exposures more than 100-fold higher than those anticipated following clinical use (Freund 1999).
Recommended dosages of zanamivir usually do not adversely affect pulmonary function in patients with respiratory disorders. However, in some patients, bronchospasm and a decline in lung function (FEV1 or peak expiratory flow) have been reported after usage of zanamivir. In most cases, these patients had underlying pulmonary conditions such as asthma or chronic obstructive pulmonary disease. Because of the risk of serious adverse events, zanamivir is not generally recommended for the treatment of patients with underlying airways disease. Zanamivir should also be discontinued in patients who develop bronchospasm or who have a decline in respiratory function. If symptoms are severe, immediate treatment and hospitalisation may be required.
Allergic reactions, including oropharyngeal oedema and serious skin rashes may rarely occur during treatment with zanamivir. In these cases, the drug should be stopped and appropriate treatment instituted.
The frequency of other side effects has been reported to be roughly identical in both treatment and placebo groups: diarrhoea, nausea, dizziness, headaches, less frequently malaise, abdominal pain, and urticaria occurred at similar frequencies and could be related to lactose vehicle inhalation. The most frequent laboratory abnormalities in Phase 3 treatment studies included elevations of liver enzymes and CPK, lymphopenia, and neutropenia. These were reported in similar proportions of zanamivir and lactose vehicle placebo recipients with acute influenza-like illness (Relenza 2003).
However, in children aged 5 to 12 years, nasal signs and symptoms (zanamivir 20 %, placebo 9 %), cough (zanamivir 16 %, placebo 8 %), and throat/tonsil discomfort and pain (zanamivir 11 %, placebo 6 %) were reported more frequently with zanamivir than placebo. In a subset with chronic respiratory disease, lower respiratory adverse events (described as asthma, cough, or viral respiratory infections which could include influenza-like symptoms) were reported in 7 out of 7 zanamivir recipients and 5 out of 12 placebo recipients.
The following adverse reactions have been identified during post-marketing use of zanamivir, but it is not possible to reliably estimate their frequency or establish a cause relationship to zanamivir exposure (Relenza 2003):
!Allergic or allergic-like reaction, including oropharyngeal oedema.
!Arrhythmias, syncope.
!Seizures.
!Bronchospasm, dyspnoea
Zanamivir has not been studied in pregnant women. In animal studies, zanamivir has not been shown to cause birth defects or other problems.
In rats, zanamivir is excreted in milk, but zanamivir has not been studied in nursing mothers and there is no information as to the possible excretion of zanamivir in human milk.
