
- •ICU Protocols
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1: Airway Management
- •Suggested Reading
- •2: Acute Respiratory Failure
- •Suggested Reading
- •Suggested Reading
- •Website
- •4: Basic Mechanical Ventilation
- •Suggested Reading
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Websites
- •7: Weaning
- •Suggested Reading
- •8: Massive Hemoptysis
- •Suggested Reading
- •9: Pulmonary Thromboembolism
- •Suggested Reading
- •Suggested Reading
- •Websites
- •11: Ventilator-Associated Pneumonia
- •Suggested Readings
- •12: Pleural Diseases
- •Suggested Reading
- •Websites
- •13: Sleep-Disordered Breathing
- •Suggested Reading
- •Websites
- •14: Oxygen Therapy
- •Suggested Reading
- •15: Pulse Oximetry and Capnography
- •Conclusion
- •Suggested Reading
- •Websites
- •16: Hemodynamic Monitoring
- •Suggested Reading
- •Websites
- •17: Echocardiography
- •Suggested Readings
- •Websites
- •Suggested Reading
- •Websites
- •19: Cardiorespiratory Arrest
- •Suggested Reading
- •Websites
- •20: Cardiogenic Shock
- •Suggested Reading
- •21: Acute Heart Failure
- •Suggested Reading
- •22: Cardiac Arrhythmias
- •Suggested Reading
- •Website
- •23: Acute Coronary Syndromes
- •Suggested Reading
- •Website
- •Suggested Reading
- •25: Aortic Dissection
- •Suggested Reading
- •26: Cerebrovascular Accident
- •Suggested Reading
- •Websites
- •27: Subarachnoid Hemorrhage
- •Suggested Reading
- •Websites
- •28: Status Epilepticus
- •Suggested Reading
- •29: Acute Flaccid Paralysis
- •Suggested Readings
- •30: Coma
- •Suggested Reading
- •Suggested Reading
- •Websites
- •32: Acute Febrile Encephalopathy
- •Suggested Reading
- •33: Sedation and Analgesia
- •Suggested Reading
- •Websites
- •34: Brain Death
- •Suggested Reading
- •Websites
- •35: Upper Gastrointestinal Bleeding
- •Suggested Reading
- •36: Lower Gastrointestinal Bleeding
- •Suggested Reading
- •37: Acute Diarrhea
- •Suggested Reading
- •38: Acute Abdominal Distension
- •Suggested Reading
- •39: Intra-abdominal Hypertension
- •Suggested Reading
- •Website
- •40: Acute Pancreatitis
- •Suggested Reading
- •Website
- •41: Acute Liver Failure
- •Suggested Reading
- •Suggested Reading
- •Websites
- •43: Nutrition Support
- •Suggested Reading
- •44: Acute Renal Failure
- •Suggested Reading
- •Websites
- •45: Renal Replacement Therapy
- •Suggested Reading
- •Website
- •46: Managing a Patient on Dialysis
- •Suggested Reading
- •Websites
- •47: Drug Dosing
- •Suggested Reading
- •Websites
- •48: General Measures of Infection Control
- •Suggested Reading
- •Websites
- •49: Antibiotic Stewardship
- •Suggested Reading
- •Website
- •50: Septic Shock
- •Suggested Reading
- •51: Severe Tropical Infections
- •Suggested Reading
- •Websites
- •52: New-Onset Fever
- •Suggested Reading
- •Websites
- •53: Fungal Infections
- •Suggested Reading
- •Suggested Reading
- •Website
- •55: Hyponatremia
- •Suggested Reading
- •56: Hypernatremia
- •Suggested Reading
- •57: Hypokalemia and Hyperkalemia
- •57.1 Hyperkalemia
- •Suggested Reading
- •Website
- •58: Arterial Blood Gases
- •Suggested Reading
- •Websites
- •59: Diabetic Emergencies
- •59.1 Hyperglycemic Emergencies
- •59.2 Hypoglycemia
- •Suggested Reading
- •60: Glycemic Control in the ICU
- •Suggested Reading
- •61: Transfusion Practices and Complications
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Website
- •63: Onco-emergencies
- •63.1 Hypercalcemia
- •63.2 ECG Changes in Hypercalcemia
- •63.3 Superior Vena Cava Syndrome
- •63.4 Malignant Spinal Cord Compression
- •Suggested Reading
- •64: General Management of Trauma
- •Suggested Reading
- •65: Severe Head and Spinal Cord Injury
- •Suggested Reading
- •Websites
- •66: Torso Trauma
- •Suggested Reading
- •Websites
- •67: Burn Management
- •Suggested Reading
- •68: General Poisoning Management
- •Suggested Reading
- •69: Syndromic Approach to Poisoning
- •Suggested Reading
- •Websites
- •70: Drug Abuse
- •Suggested Reading
- •71: Snakebite
- •Suggested Reading
- •72: Heat Stroke and Hypothermia
- •72.1 Heat Stroke
- •72.2 Hypothermia
- •Suggested Reading
- •73: Jaundice in Pregnancy
- •Suggested Reading
- •Suggested Reading
- •75: Severe Preeclampsia
- •Suggested Reading
- •76: General Issues in Perioperative Care
- •Suggested Reading
- •Web Site
- •77.1 Cardiac Surgery
- •77.2 Thoracic Surgery
- •77.3 Neurosurgery
- •Suggested Reading
- •78: Initial Assessment and Resuscitation
- •Suggested Reading
- •79: Comprehensive ICU Care
- •Suggested Reading
- •Website
- •80: Quality Control
- •Suggested Reading
- •Websites
- •81: Ethical Principles in End-of-Life Care
- •Suggested Reading
- •82: ICU Organization and Training
- •Suggested Reading
- •Website
- •83: Transportation of Critically Ill Patients
- •83.1 Intrahospital Transport
- •83.2 Interhospital Transport
- •Suggested Reading
- •84: Scoring Systems
- •Suggested Reading
- •Websites
- •85: Mechanical Ventilation
- •Suggested Reading
- •86: Acute Severe Asthma
- •Suggested Reading
- •87: Status Epilepticus
- •Suggested Reading
- •88: Severe Sepsis and Septic Shock
- •Suggested Reading
- •89: Acute Intracranial Hypertension
- •Suggested Reading
- •90: Multiorgan Failure
- •90.1 Concurrent Management of Hepatic Dysfunction
- •Suggested Readings
- •91: Central Line Placement
- •Suggested Reading
- •92: Arterial Catheterization
- •Suggested Reading
- •93: Pulmonary Artery Catheterization
- •Suggested Reading
- •Website
- •Suggested Reading
- •95: Temporary Pacemaker Insertion
- •Suggested Reading
- •96: Percutaneous Tracheostomy
- •Suggested Reading
- •97: Thoracentesis
- •Suggested Reading
- •98: Chest Tube Placement
- •Suggested Reading
- •99: Pericardiocentesis
- •Suggested Reading
- •100: Lumbar Puncture
- •Suggested Reading
- •Website
- •101: Intra-aortic Balloon Pump
- •Suggested Reading
- •Appendices
- •Appendix A
- •Appendix B
- •Common ICU Formulae
- •Appendix C
- •Appendix D: Syllabus for ICU Training
- •Index
53 Fungal Infections |
423 |
|
|
Suggested Reading
1.Hsueh PR, Graybill JR, et al. Consensus statement on the management of invasive candidiasis in intensive care units in the Asia-Pacific region. Int J Antimicrob Agents. 2009;34(3):205–9.
Candida albicans remains the predominant cause of invasive candidiasis in ICUs, followed by Candida tropicalis, Candida glabrata, and Candida parapsilosis. Invasive isolates of Candida spp. remain highly susceptible to fluconazole (>90% susceptible), although among Asia-Pacific countries the susceptibility rate of C. glabrata to fluconazole varies widely from 22% to 72%.
2.Darouiche RO. Candida in the ICU. Clin Chest Med. 2009;30(2):287–93.
Although treatment for documented, deep-seated Candida infections in nonneutropenic patients has been studied extensively, guidelines for the management of suspected but undocumented cases of invasive Candida infections in critically ill patients have not been clearly established.
3.Pappas PG, Kauffman CA, Andes D, Benjamin DK Jr, Calandra TF, Edwards JE Jr, Filler SG, et al. Clinical practice guidelines for the management of candidiasis: 2009 update by the Infectious Diseases Society of America. Clinl Infec Dis. 2009;48:503–35.
4.Lam SW, Eschenauer GA. Evolving role of early antifungals in the adult intensive care unit. Crit Care Med. 2009;37(5):1580–93.
The use of early antifungal therapy should be reserved for patients with a high risk (10–15%) of developing invasive candidiasis (IC). There is no single predictive rule that can adequately forecast IC in critically ill patients. Clinicians should assess patients on a case-by-case basis and determine the need for early antifungal treatment strategies based on frequent evaluations of risk factors and clinical status.

Host |
54 |
Infections in the Immunocompromised |
|
Subhash Todi and Om Srivastav
A 29-year-old female patient, 2 years after kidney transplant, on mycophenolate, sirolimus, and prednisolone, presented with semiconsciousness, ulcerating lesions around right elbow, and oliguria for the past 6 h.
Managing infection in an immunocompromised patient is a challenge to any ICU physician, as the presentation is varied and subtle and needs high index of suspicion for diagnosis and multiple possible etiologies. A methodological approach to investigation and choice of empirical therapy is warranted in these patients. Complexity of the problem necessitates close liaison between the microbiologist, infectious disease consultant, and hemato-oncologist.
Step 1: Resuscitate
•If assisted respiration is required, initially noninvasive ventilation should be tried.
•The patient should be closely monitored, and if no improvement or deterioration occurs in 2 h, invasive ventilation should be initiated.
•Invasive catheters and lines should be avoided as these patients are coagulopathic and neutropenic and have a high risk of line sepsis.
•Careful maintenance of the peripheral channel is extremely vital in these patients.
Step 2: Take a focused history (Table 54.1)
•This should be done to determine the type and duration of the immunocompromised state.
S. Todi, M.D., M.R.C.P. (*)
Critical Care & Emergency, A.M.R.I. Hospital, Kolkata, India e-mail: drsubhashtodi@gmail.com
Om. Srivastav, M.D.
Infectious Disease, Jaslok Hospital, Mumbai, India
R. Chawla and S. Todi (eds.), ICU Protocols: A stepwise approach, |
425 |
DOI 10.1007/978-81-322-0535-7_54, © Springer India 2012 |
|
426 |
S. Todi and Om. Srivastav |
|
|
|
|
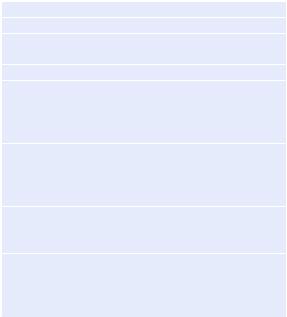
Table 54.1 Syndromic |
Pneumonia |
|
approach to infection in |
Focal/nodular infiltrate |
|
immunocompromised |
||
Bacteria, Aspergillus, mycobacteria, Nocardia, Histoplasma |
||
patients |
||
Diffuse Infiltrate |
||
|
||
|
Virus (cytomegalo, herpes), Pneumocystis, Strongyloides |
|
|
Meningoencephalitis |
|
|
Bacteria: Neisseria, Hemophilus, Pneumococcus, Listeria |
|
|
Mycobacteria: typical and atypical |
|
|
Fungus: Cryptococcus |
|
|
Focal CNS lesions |
|
|
Toxoplasma |
|
|
Tuberculoma |
|
|
Nocardia |
|
|
Severe sepsis or septic shock |
|
|
Gram-positive and Gram-negative bacteria |
|
|
Candidemia |
|
|
Gastroenteritis |
|
|
Strongyloides |
|
|
Cryptococcosis |
|
|
Amebiasis |
•Disease states such as hematological malignancy (leukemia and lymphoma), solid organ tumor, and conditions associated with neutropenic state should be looked for.
•History of any organ transplant and duration since transplant should be taken.
•HIV status should be determined, with proper consent.
•History of chemotherapy or radiotherapy should be taken.
•Detailed drug history should be elicited.
•Neurological, respiratory, gastrointestinal symptoms need to be elicited to narrow down differential diagnosis of opportunistic infection.
Step 3: Perform focused physical examination (Table 54.1)
•Any breach of skin or mucosal abrasion, skin ulcer, oral ulcer, oral thrush, and perianal lesion should be searched for.
•Look for skin rash.
•All insertion sites of invasive lines should be inspected for tenderness or discharge.
•All suture lines and drain sites should be inspected in postoperative patients after removing the dressing.
•Look at the back for decubitus ulcer.
•Do neurological, respiratory, and gastrointestinal system examination to determine organ system involvement.
Step 4: Send basic investigations
•There is a broad differential diagnosis of opportunistic infection—bacterial, viral, or fungal—in immunocompromised patients.
54 Infections in the Immunocompromised Host |
427 |
|
|
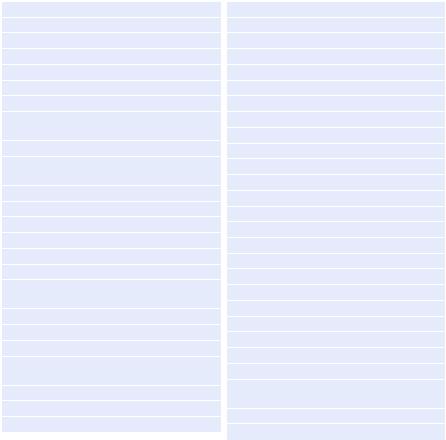
Table 54.2 Immunodeficiency states
T-lymphocyte deficiency
Causes
HIV/AIDS
Lymphoma
Corticosteroids
Drugs (methotrexate)
Organisms
Intracellular bacteria (mycobacteria,
Legionella)
Virus (herpes, cytomegalovirus)
Fungi (Pneumocystis, Cryptococcus,
Histoplasma)
Parasites (Strongyloides, Toxoplasma)
Nocardia
B-lymphocyte deficiency
Causes
Multiple myeloma
Acute leukemia
Drugs (corticosteroid, azathioprine, mycophenolate)
Plasmapheresis
Burn
Organisms
Encapsulated bacteria (Neisseria, Pneumococcus, Hemophilus)
Salmonella
Campylobacter
Giardia
Neutropenia
Causes
Chemotherapy
Hematological malignancy
Myelodysplasia
Severe viral infection
Hypersplenism
Organisms
Gram-negative bacilli (enteric and nonenteric)
Staphylococcus aureus
Coagulase-negative Staphylococcus
Streptococci, enterococci
Fungi (Aspergillus spp., Candida spp.)
Neutrophil dysfunction
Causes
Diabetes
Uremia
Alcoholism
Cirrhosis
Burn
Organisms
Staphylococcus aureus
Streptococci
Mucor (Zygomycoses)
Gram negative bacilli (enteric and non-enteric)
Coagulase negative staphylococcus
Fungi (Aspergillus spp., Candida spp.)
•These patients are also prone to infections which are common in nonimmunocompromised patients.
•In these patients, infection mimics drug reaction, transfusion reaction, radiationinduced complications, and disease-associated problems, which all need to be properly investigated.
•Focused investigation, initially noninvasive and then invasive, should be performed to confirm the causative organism in order to narrow down anti-infective agents.
Step 5: Identify underlying immune deficiency states and suspected pathogens (Table 54.2)
•Based on history, physical examination, and basic investigation, an approximation of underlying immunodeficiency states needs to be recognized.
428 |
|
S. Todi and Om. Srivastav |
|
||
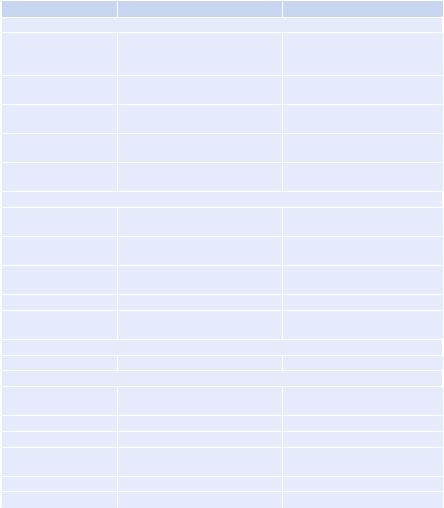
Table 54.3 Diagnostic test and treatment of opportunistic pathogens |
||
Organism |
Test |
Treatment |
Bacteria |
|
|
Gram-positive/negative |
Gram Stain: BAL, Fluid, Urine |
Vancomycin/teicoplanin/ |
|
Cultures (aerobic and anaerobic): |
daptomycin (Gm+) Carbapenem, |
|
Blood, BAL, Fluids, Urine |
piperacillin–tazobactam (Gm−) |
Mycobacterium |
Induced sputum/BAL/AFB stain |
Four-drug therapy |
tuberculosis |
|
|
Nontuberculosis |
Induced sputum/BAL/AFB stain |
Variable |
mycobacteria |
|
|
Nocardia spp. |
Sputum/biopsy/modified AFB |
Trimethoprim-Sulphamethoxazole |
|
stain |
(TMP-SMX) |
Legionella |
Sputum/BAL culture/urine |
Macrolide / Respiratory |
|
antigen |
fluoroquinolone |
Fungi |
|
|
Candida |
Blood culture/biopsy |
Echinocandin, amphotericin B, |
|
|
azoles |
Aspergillus |
BAL/TBB/sputum Fungal stain, |
Amphotericin B/voriconazole |
|
galactomannan, H & P |
|
Pneumocystis jiroveci |
Induced sputum/BAL/DFA |
TMP-SMX/corticosteroid |
|
|
(pao2 < 70) |
Cryptococcus |
Serum/CSF antigen/blood culture |
Ampho B/flucytosine |
Histoplasma |
Urine antigen/histology/fungal |
Ampho B/itraconazole |
|
culture |
|
Parasites |
|
|
Toxoplasma |
CSF/blood PCR |
Pyrimethamine/sulfadiazine |
Virus |
|
|
Cytomegalovirus |
Blood CMVPCR/PP65 antigen/ |
Ganciclovir/foscarnet |
|
BAL Biopsy—H & P, culture |
|
Varicella zoster |
BAL/CSF PCR, histology |
Acyclovir |
Herpes simplex |
CSF/blood PCR |
Acyclovir |
Influenza |
Nasopharyngeal swab BAL DFA/ |
Oseltamivir/zanamivir |
|
culture |
|
Epstein–Barr |
CSF PCR |
Lymphoma chemo |
RSV |
Nasopharyngeal swab/BAL DFA |
Palivizumab |
For doses, see Appendix 1 |
|
|
•Specific immunodeficiency states are associated with alteration of natural defense system (neutrophils, T cell, B cells).
•Patients with specific defense system alteration have propensity to be infected with certain groups of organisms, which need to be recognized.
Step 6: Initiate empirical anti-infective agents (Table 54.3)
•Guided by the type and duration of immunosuppression and primary organ system involvement, broad-spectrum anti-infective agents should be initiated against suspected organisms.
