
- •ICU Protocols
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1: Airway Management
- •Suggested Reading
- •2: Acute Respiratory Failure
- •Suggested Reading
- •Suggested Reading
- •Website
- •4: Basic Mechanical Ventilation
- •Suggested Reading
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Websites
- •7: Weaning
- •Suggested Reading
- •8: Massive Hemoptysis
- •Suggested Reading
- •9: Pulmonary Thromboembolism
- •Suggested Reading
- •Suggested Reading
- •Websites
- •11: Ventilator-Associated Pneumonia
- •Suggested Readings
- •12: Pleural Diseases
- •Suggested Reading
- •Websites
- •13: Sleep-Disordered Breathing
- •Suggested Reading
- •Websites
- •14: Oxygen Therapy
- •Suggested Reading
- •15: Pulse Oximetry and Capnography
- •Conclusion
- •Suggested Reading
- •Websites
- •16: Hemodynamic Monitoring
- •Suggested Reading
- •Websites
- •17: Echocardiography
- •Suggested Readings
- •Websites
- •Suggested Reading
- •Websites
- •19: Cardiorespiratory Arrest
- •Suggested Reading
- •Websites
- •20: Cardiogenic Shock
- •Suggested Reading
- •21: Acute Heart Failure
- •Suggested Reading
- •22: Cardiac Arrhythmias
- •Suggested Reading
- •Website
- •23: Acute Coronary Syndromes
- •Suggested Reading
- •Website
- •Suggested Reading
- •25: Aortic Dissection
- •Suggested Reading
- •26: Cerebrovascular Accident
- •Suggested Reading
- •Websites
- •27: Subarachnoid Hemorrhage
- •Suggested Reading
- •Websites
- •28: Status Epilepticus
- •Suggested Reading
- •29: Acute Flaccid Paralysis
- •Suggested Readings
- •30: Coma
- •Suggested Reading
- •Suggested Reading
- •Websites
- •32: Acute Febrile Encephalopathy
- •Suggested Reading
- •33: Sedation and Analgesia
- •Suggested Reading
- •Websites
- •34: Brain Death
- •Suggested Reading
- •Websites
- •35: Upper Gastrointestinal Bleeding
- •Suggested Reading
- •36: Lower Gastrointestinal Bleeding
- •Suggested Reading
- •37: Acute Diarrhea
- •Suggested Reading
- •38: Acute Abdominal Distension
- •Suggested Reading
- •39: Intra-abdominal Hypertension
- •Suggested Reading
- •Website
- •40: Acute Pancreatitis
- •Suggested Reading
- •Website
- •41: Acute Liver Failure
- •Suggested Reading
- •Suggested Reading
- •Websites
- •43: Nutrition Support
- •Suggested Reading
- •44: Acute Renal Failure
- •Suggested Reading
- •Websites
- •45: Renal Replacement Therapy
- •Suggested Reading
- •Website
- •46: Managing a Patient on Dialysis
- •Suggested Reading
- •Websites
- •47: Drug Dosing
- •Suggested Reading
- •Websites
- •48: General Measures of Infection Control
- •Suggested Reading
- •Websites
- •49: Antibiotic Stewardship
- •Suggested Reading
- •Website
- •50: Septic Shock
- •Suggested Reading
- •51: Severe Tropical Infections
- •Suggested Reading
- •Websites
- •52: New-Onset Fever
- •Suggested Reading
- •Websites
- •53: Fungal Infections
- •Suggested Reading
- •Suggested Reading
- •Website
- •55: Hyponatremia
- •Suggested Reading
- •56: Hypernatremia
- •Suggested Reading
- •57: Hypokalemia and Hyperkalemia
- •57.1 Hyperkalemia
- •Suggested Reading
- •Website
- •58: Arterial Blood Gases
- •Suggested Reading
- •Websites
- •59: Diabetic Emergencies
- •59.1 Hyperglycemic Emergencies
- •59.2 Hypoglycemia
- •Suggested Reading
- •60: Glycemic Control in the ICU
- •Suggested Reading
- •61: Transfusion Practices and Complications
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Website
- •63: Onco-emergencies
- •63.1 Hypercalcemia
- •63.2 ECG Changes in Hypercalcemia
- •63.3 Superior Vena Cava Syndrome
- •63.4 Malignant Spinal Cord Compression
- •Suggested Reading
- •64: General Management of Trauma
- •Suggested Reading
- •65: Severe Head and Spinal Cord Injury
- •Suggested Reading
- •Websites
- •66: Torso Trauma
- •Suggested Reading
- •Websites
- •67: Burn Management
- •Suggested Reading
- •68: General Poisoning Management
- •Suggested Reading
- •69: Syndromic Approach to Poisoning
- •Suggested Reading
- •Websites
- •70: Drug Abuse
- •Suggested Reading
- •71: Snakebite
- •Suggested Reading
- •72: Heat Stroke and Hypothermia
- •72.1 Heat Stroke
- •72.2 Hypothermia
- •Suggested Reading
- •73: Jaundice in Pregnancy
- •Suggested Reading
- •Suggested Reading
- •75: Severe Preeclampsia
- •Suggested Reading
- •76: General Issues in Perioperative Care
- •Suggested Reading
- •Web Site
- •77.1 Cardiac Surgery
- •77.2 Thoracic Surgery
- •77.3 Neurosurgery
- •Suggested Reading
- •78: Initial Assessment and Resuscitation
- •Suggested Reading
- •79: Comprehensive ICU Care
- •Suggested Reading
- •Website
- •80: Quality Control
- •Suggested Reading
- •Websites
- •81: Ethical Principles in End-of-Life Care
- •Suggested Reading
- •82: ICU Organization and Training
- •Suggested Reading
- •Website
- •83: Transportation of Critically Ill Patients
- •83.1 Intrahospital Transport
- •83.2 Interhospital Transport
- •Suggested Reading
- •84: Scoring Systems
- •Suggested Reading
- •Websites
- •85: Mechanical Ventilation
- •Suggested Reading
- •86: Acute Severe Asthma
- •Suggested Reading
- •87: Status Epilepticus
- •Suggested Reading
- •88: Severe Sepsis and Septic Shock
- •Suggested Reading
- •89: Acute Intracranial Hypertension
- •Suggested Reading
- •90: Multiorgan Failure
- •90.1 Concurrent Management of Hepatic Dysfunction
- •Suggested Readings
- •91: Central Line Placement
- •Suggested Reading
- •92: Arterial Catheterization
- •Suggested Reading
- •93: Pulmonary Artery Catheterization
- •Suggested Reading
- •Website
- •Suggested Reading
- •95: Temporary Pacemaker Insertion
- •Suggested Reading
- •96: Percutaneous Tracheostomy
- •Suggested Reading
- •97: Thoracentesis
- •Suggested Reading
- •98: Chest Tube Placement
- •Suggested Reading
- •99: Pericardiocentesis
- •Suggested Reading
- •100: Lumbar Puncture
- •Suggested Reading
- •Website
- •101: Intra-aortic Balloon Pump
- •Suggested Reading
- •Appendices
- •Appendix A
- •Appendix B
- •Common ICU Formulae
- •Appendix C
- •Appendix D: Syllabus for ICU Training
- •Index
Severe Head and Spinal Cord Injury |
65 |
|
|
Deepak Agrawal |
|
A 25-year-old adult traveling by a car suffered multiple injuries in a high-speed collision. On arrival to the emergency department, he was found unconscious, with bleeding from the right ear and obvious bleeding from the scalp. His pulse was 56/min and blood pressure (BP) was 180/96 mmHg. The right pupil was dilated and not reacting, and his breathing was labored. Smell of alcohol was also observed.
Head and spinal cord injuries are typically associated with major trauma from motor vehicle accidents, falls, sports injuries, and violence. These injuries are associated with high morbidity and mortality. Prompt and appropriate treatment can change the outcome of these patients.
Step 1: Initialasses sment
Airway, breathing, and circulation (ABC) approach takes precedence in spite of obvious head injury.
Airway and breathing
•Apply the cervical collar and check airway.
•Hypoxia (PaO2 <60 mmHg or O2 saturation <90%) should be avoided. Intubate and ventilate with 100% oxygen in case of threatened airway with manual in-line cervical immobilization.
•Mild hyperventilation (PaCO2 ³32 mmHg and £36 mmHg) is recommended as a temporizing measure for the reduction of raised intracranial pressure (ICP).
•Prophylactic hyperventilation (PaCO2 £25 mmHg) is not recommended.
D. Agrawal, M.S., M.Ch. (*)
Department of Neurosurgery, AIIMS, New Delhi, India e-mail: drdeepak@gmail.com
R. Chawla and S. Todi (eds.), ICU Protocols: A stepwise approach, |
521 |
DOI 10.1007/978-81-322-0535-7_65, © Springer India 2012 |
|
522 |
D. Agrawal |
|
|
Circulation
•Maintain systolic BP >100 mmHg.
•Avoid antihypertensives in suspected head injuries as arterial hypertension is a part of protective Cushing’s reflex to maintain cerebral perfusion.
•Labetalol is the drug of choice for control of hypertensive emergency in the head injury patient (refer to Chap. 24 on hypertension).
Step 2: Secondary assessment
•Assess Glasgow coma score (GCS) and pupillary reaction, and check localizing signs (weakness in limbs).
•All patients with GCS of 8 or less should be intubated and electively ventilated (if not done at Step 1).
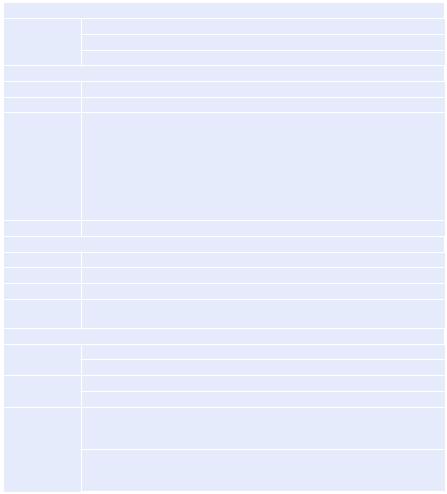
Step 3: Assess severity of head injury
On GCS grading
GCS of 14 or 15: mild head injury
GCS of 9–13: moderate head injury
GCS of 8 or less: severe head injury
Mild head injury
Step A |
Shift to observational area. |
Step B |
Maintain ABC. |
Step C |
Send for a noncontrast CT (NCCT) of the head and cervical spine (if any neck |
|
pain/tenderness) in the following conditions: |
|
Loss of consciousness for more than 5 min |
|
Amnesia |
|
Severe headache |
|
GCS of less than 15 |
|
Focal neurological deficit attributable to the brain |
Step D |
Inform the neurosurgeon. |
Moderate head injury |
|
Step A |
Shift to observational area. |
Step B |
Maintain ABC. |
Step C |
Inform the neurosurgeon. |
Step D |
Send for the plain CT scan of the head cervical spine. (All patients to have the |
|
CT scan of cervical spine including C7 vertebrae.) |
Severe head injury |
|
Step A |
Shift to the resuscitation room. |
|
Simultaneously inform the neurosurgeon. |
Step B |
Repeat ABC. |
|
Maintain temperature. |
Step C |
Send for baseline blood investigation (hemoglobin, hematocrit, platelets, |
|
coagulation profile, random blood sugar, serum sodium and potassium, urea, |
|
creatinine). |
|
Coagulation profile including prothrombin time, APTT, and platelet count |
|
should be done in all patients. Special tests like thromboelastography may be |
|
done, if available, to assess platelet function. |
65 Severe Head and Spinal Cord Injury |
523 |
|
|
|
|
|
Arrange packed RBC or fresh frozen plasma. |
|
|
Arterial blood gas (to be repeated after 1 h). |
|
|
Foley’s catheterization. |
|
|
IV fluid maintenance—avoid dextrose-containing fluids as they may increase |
|
|
cerebral edema. |
|
|
Proton pump inhibitor. |
|
|
Phenytoin sodium IV loading dose of 20 mg/kg can be dissolved in normal |
|
|
saline and infused at a rate no faster than 50 mg/min. Fosphenytoin can also be |
|
|
used at a dose of 25 mg/kg and can be infused at a rate of up to 150 mg/min. |
|
|
Infuse 20% mannitol (1 g/kg IV stat) in 5 min (after BP correction). |
|
|
Give furosemide (0.3–0.5 mg/kg IV stat) (after BP correction). |
|
Step D |
A focused assessment by sonography in trauma (FAST) is required to assess |
|
|
any other site of free blood in case of persistent/recurrent hypotension. |
|
Step E |
Send for the non contrast CT scan of the head cervical spine on portable |
|
|
ventilator with the resident and the nurse, with prior information to the |
|
|
radiographer and radiology resident. All patients to have the CT scan of |
|
|
cervical spine up to C7. |
|
The head injury patient should be monitored closely when he/she is kept for observation or waiting for admission.
In case neurosurgical facilities are not available in the hospital, the patient should not be denied initial assessment and management (Step 1) as these are critical to final outcome. The patient can be transferred to the nearest neurosurgical facility after initial management.
Step 4: Shift to the intensive care unit (ICU)
All patients with nonoperable lesions and requiring intubation should be shifted to the ICU for further management.
Step 5: Start analgesia and sedation
•Sedatives and analgesics can affect outcomes in head-injured patients.
•Adequate pain control and sedation can be used as initial measures to control raised ICP. Short-acting agents such as fentanyl, midazolam, or propofol are preferred for frequent neurological assessments.
•Propofol infusion and high-dose barbiturate administration are recommended to control elevated ICP refractory to maximum standard medical and/or surgical treatment.
•Hemodynamic stability is essential before and during barbiturate therapy.
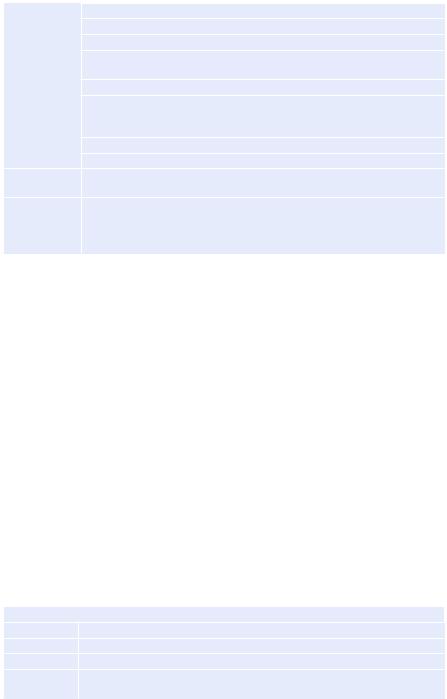
Commonly used sedatives
Fentanyl |
2 mcg/kg test dose, 2–5 mcg/kg/h continuous infusion |
Midazolam |
2 mg test dose, 2–4 mg/h continuous infusion |
Sufentanil |
10–30 mcg test bolus, 0.05–2 mcg/kg continuous infusion |
Propofol |
0.5 mg/kg test bolus, 20–75 mcg/kg/min continuous infusion (not to exceed |
|
5 mg/kg/h) |
524 |
D. Agrawal |
|
|
•Continuous use may increase the risk of ventilator-associated pneumonia; hence, daily interruption of sedation along with other VAP prevention measures should be used.
Step 6: ICP monitoring
Indications of ICP monitoring
ICP should be monitored in patients with GCS of 8 or less and an abnormal computed tomography (CT) scan.
An abnormal CT scan of the head is one that reveals hematomas, contusions, swelling, herniation, or compressed basal cisterns.
ICP should be monitored in patients with severe traumatic brain injury (TBI) with a normal CT scan if two or more of the following features are noted at admission: age over 40 years, unilateral or bilateral motor posturing, or systolic BP less than 90 mmHg.
All children (<12 years) should have ICP monitoring irrespective of CT findings if GCS is 8 or less.
Monitoring method
The ventricular catheter connected to an external strain gauge is the most accurate, low-cost, and reliable method of monitoring ICP with the additional benefit of having a therapeutic role by cerebrospinal fluid drainage. However, they carry a higher risk of infection and may be difficult to insert in brain swelling with effaced ventricles.
ICP transduction via fiber-optic or microstrain gauge devices placed in parenchyma is easy to insert, equally accurate, but much more expensive.
Treatment target
Treatment should be initiated with ICP thresholds above 20 mmHg.
A combination of ICP values, and clinical and brain CT findings, should be used to determine the need for treatment. Decompressive craniectomy may be considered for persistently high ICP (>20 mmHg) despite maximal medical therapy but its role is debatable.
Step 7: Start mannitol (refer to Chap. 31)
•In absence of hypotension, mannitol is effective for the control of raised ICP at doses of 0.25–1 g/kg body weight.
•Mannitol is contraindicated in extradural hematoma and should be given only after reviewing the CT scan of the head and under neurosurgical supervision.
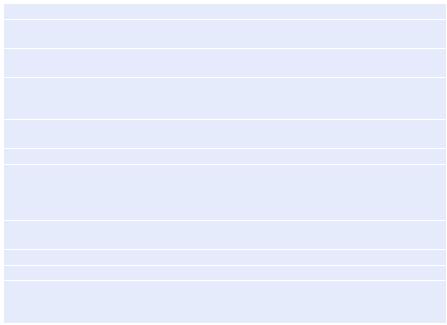
Step 8: Tracheostomy
•Plan an early tracheostomy (within 72 h) for all patients whose motor response is 4 or less.
Step 9: Deep venous thrombosis (DVT) prophylaxis
•Intermittent pneumatic compression stockings or graduated compression stockings should be used (except in lower limb injuries) and continued till the patient is ambulatory.
•Low-molecular-weight heparin or low-dose unfractionated heparin should be used in combination with mechanical prophylaxis when it is safe, preferably after 72 h of intracranial hemorrhage/craniotomy with close monitoring and repeat NCCT head to detect expansion of hematoma.
65 Severe Head and Spinal Cord Injury |
525 |
|
|
Step 10: Seizure prophylaxis
•Phenytoin (5 mg/kg/day) or valproate (15 mg/kg/day) should be given for at least a week in all patients.
•Prophylactic use of phenytoin or valproate is not recommended for preventing late posttraumatic seizures. However, their use in the first week following injury decreases the incidence of early posttraumatic seizures.
Step 11: Maintain nutrition
•Good caloric intake (30–50 kcal/kg/day) and protein intake of 2 g/kg/day should be maintained. To achieve full caloric replacement in 7 days, nutritional replacement should begin no later than 72 h after injury.
Step 12: Other drugs/interventions
•Avoid steroids. Use of steroids is not recommended for improving outcome or reducing ICP.
•Use of high-dose methylprednisolone increases mortality, and therefore, it is contraindicated.
•Prophylactic mild hypothermia (33–35°C) remains experimental and is not recommended for routine clinical use presently.
Step 13: Surgical intervention
•Head injuries: Decompressive craniectomy
•If the patient continues to have persistently raised ICP (>20 mmHg) in spite of maximal medical management, decompressive craniectomy is the only available option to decrease ICP.
•Recent evidence has shown poor neurological outcome in patient undergoing decompressive craniectomy.
Management of High Cervical Spinal Cord Injuries
A 50-year-old male fell from a 20-ft height. On arrival to the emergency department, he was found to be conscious, with labored breathing and no limb movement. His pulse was 52/min and his BP was 70/40 mmHg.
Steps 1 and 2 Remain the same as for severe head injuries |
|
Step 3 |
ICU care |
|
Management of patients with acute spinal cord injury (SCI), particularly |
|
patients with severe cervical level injuries, is recommended in an ICU or |
|
similar monitored setting. |
Step 4 |
BP management |
|
Maintain mean arterial BP at 85–90 mmHg for the first 7 days following acute |
|
SCI as it improves spinal cord perfusion. |
|
If central venous pressure exceeds 10 cm of water, dopamine and/or noradrena- |
|
line infusion may be given to maintain BP at this level. |
