
- •ICU Protocols
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1: Airway Management
- •Suggested Reading
- •2: Acute Respiratory Failure
- •Suggested Reading
- •Suggested Reading
- •Website
- •4: Basic Mechanical Ventilation
- •Suggested Reading
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Websites
- •7: Weaning
- •Suggested Reading
- •8: Massive Hemoptysis
- •Suggested Reading
- •9: Pulmonary Thromboembolism
- •Suggested Reading
- •Suggested Reading
- •Websites
- •11: Ventilator-Associated Pneumonia
- •Suggested Readings
- •12: Pleural Diseases
- •Suggested Reading
- •Websites
- •13: Sleep-Disordered Breathing
- •Suggested Reading
- •Websites
- •14: Oxygen Therapy
- •Suggested Reading
- •15: Pulse Oximetry and Capnography
- •Conclusion
- •Suggested Reading
- •Websites
- •16: Hemodynamic Monitoring
- •Suggested Reading
- •Websites
- •17: Echocardiography
- •Suggested Readings
- •Websites
- •Suggested Reading
- •Websites
- •19: Cardiorespiratory Arrest
- •Suggested Reading
- •Websites
- •20: Cardiogenic Shock
- •Suggested Reading
- •21: Acute Heart Failure
- •Suggested Reading
- •22: Cardiac Arrhythmias
- •Suggested Reading
- •Website
- •23: Acute Coronary Syndromes
- •Suggested Reading
- •Website
- •Suggested Reading
- •25: Aortic Dissection
- •Suggested Reading
- •26: Cerebrovascular Accident
- •Suggested Reading
- •Websites
- •27: Subarachnoid Hemorrhage
- •Suggested Reading
- •Websites
- •28: Status Epilepticus
- •Suggested Reading
- •29: Acute Flaccid Paralysis
- •Suggested Readings
- •30: Coma
- •Suggested Reading
- •Suggested Reading
- •Websites
- •32: Acute Febrile Encephalopathy
- •Suggested Reading
- •33: Sedation and Analgesia
- •Suggested Reading
- •Websites
- •34: Brain Death
- •Suggested Reading
- •Websites
- •35: Upper Gastrointestinal Bleeding
- •Suggested Reading
- •36: Lower Gastrointestinal Bleeding
- •Suggested Reading
- •37: Acute Diarrhea
- •Suggested Reading
- •38: Acute Abdominal Distension
- •Suggested Reading
- •39: Intra-abdominal Hypertension
- •Suggested Reading
- •Website
- •40: Acute Pancreatitis
- •Suggested Reading
- •Website
- •41: Acute Liver Failure
- •Suggested Reading
- •Suggested Reading
- •Websites
- •43: Nutrition Support
- •Suggested Reading
- •44: Acute Renal Failure
- •Suggested Reading
- •Websites
- •45: Renal Replacement Therapy
- •Suggested Reading
- •Website
- •46: Managing a Patient on Dialysis
- •Suggested Reading
- •Websites
- •47: Drug Dosing
- •Suggested Reading
- •Websites
- •48: General Measures of Infection Control
- •Suggested Reading
- •Websites
- •49: Antibiotic Stewardship
- •Suggested Reading
- •Website
- •50: Septic Shock
- •Suggested Reading
- •51: Severe Tropical Infections
- •Suggested Reading
- •Websites
- •52: New-Onset Fever
- •Suggested Reading
- •Websites
- •53: Fungal Infections
- •Suggested Reading
- •Suggested Reading
- •Website
- •55: Hyponatremia
- •Suggested Reading
- •56: Hypernatremia
- •Suggested Reading
- •57: Hypokalemia and Hyperkalemia
- •57.1 Hyperkalemia
- •Suggested Reading
- •Website
- •58: Arterial Blood Gases
- •Suggested Reading
- •Websites
- •59: Diabetic Emergencies
- •59.1 Hyperglycemic Emergencies
- •59.2 Hypoglycemia
- •Suggested Reading
- •60: Glycemic Control in the ICU
- •Suggested Reading
- •61: Transfusion Practices and Complications
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Website
- •63: Onco-emergencies
- •63.1 Hypercalcemia
- •63.2 ECG Changes in Hypercalcemia
- •63.3 Superior Vena Cava Syndrome
- •63.4 Malignant Spinal Cord Compression
- •Suggested Reading
- •64: General Management of Trauma
- •Suggested Reading
- •65: Severe Head and Spinal Cord Injury
- •Suggested Reading
- •Websites
- •66: Torso Trauma
- •Suggested Reading
- •Websites
- •67: Burn Management
- •Suggested Reading
- •68: General Poisoning Management
- •Suggested Reading
- •69: Syndromic Approach to Poisoning
- •Suggested Reading
- •Websites
- •70: Drug Abuse
- •Suggested Reading
- •71: Snakebite
- •Suggested Reading
- •72: Heat Stroke and Hypothermia
- •72.1 Heat Stroke
- •72.2 Hypothermia
- •Suggested Reading
- •73: Jaundice in Pregnancy
- •Suggested Reading
- •Suggested Reading
- •75: Severe Preeclampsia
- •Suggested Reading
- •76: General Issues in Perioperative Care
- •Suggested Reading
- •Web Site
- •77.1 Cardiac Surgery
- •77.2 Thoracic Surgery
- •77.3 Neurosurgery
- •Suggested Reading
- •78: Initial Assessment and Resuscitation
- •Suggested Reading
- •79: Comprehensive ICU Care
- •Suggested Reading
- •Website
- •80: Quality Control
- •Suggested Reading
- •Websites
- •81: Ethical Principles in End-of-Life Care
- •Suggested Reading
- •82: ICU Organization and Training
- •Suggested Reading
- •Website
- •83: Transportation of Critically Ill Patients
- •83.1 Intrahospital Transport
- •83.2 Interhospital Transport
- •Suggested Reading
- •84: Scoring Systems
- •Suggested Reading
- •Websites
- •85: Mechanical Ventilation
- •Suggested Reading
- •86: Acute Severe Asthma
- •Suggested Reading
- •87: Status Epilepticus
- •Suggested Reading
- •88: Severe Sepsis and Septic Shock
- •Suggested Reading
- •89: Acute Intracranial Hypertension
- •Suggested Reading
- •90: Multiorgan Failure
- •90.1 Concurrent Management of Hepatic Dysfunction
- •Suggested Readings
- •91: Central Line Placement
- •Suggested Reading
- •92: Arterial Catheterization
- •Suggested Reading
- •93: Pulmonary Artery Catheterization
- •Suggested Reading
- •Website
- •Suggested Reading
- •95: Temporary Pacemaker Insertion
- •Suggested Reading
- •96: Percutaneous Tracheostomy
- •Suggested Reading
- •97: Thoracentesis
- •Suggested Reading
- •98: Chest Tube Placement
- •Suggested Reading
- •99: Pericardiocentesis
- •Suggested Reading
- •100: Lumbar Puncture
- •Suggested Reading
- •Website
- •101: Intra-aortic Balloon Pump
- •Suggested Reading
- •Appendices
- •Appendix A
- •Appendix B
- •Common ICU Formulae
- •Appendix C
- •Appendix D: Syllabus for ICU Training
- •Index
Intra-aortic Balloon Pump |
101 |
|
|
Khusrav Bajan |
|
A 55-year-old male patient was admitted to hospital with a history of chest pain for about 3 h. He was drowsy, extremities were cold, and his blood pressure was 84/60 mmHg. He was started on inotropic and vasopressor support, but he remained hypotensive.
Intra-aortic balloon pump (IABP) is a mechanical support device to support cardiac pump function by increasing coronary perfusion and decreasing afterload and used as a salvage therapy in cardiogenic shock. IABP therapy should only be considered for use in patients who have the potential for left ventricular recovery or to support those awaiting cardiac transplantation.
Step 1: Assess the need for IABP—indications
Since the balloon counterpulsation helps to improve myocardial oxygen supply and decrease oxygen demand, the IABP is indicated for conditions with decreased myocardial oxygen supply–demand ratio:
•Cardiogenic shock
•Acute myocardial infarction with pulmonary edema
•Mechanical complications of myocardial infarction (ventricular septal defect, acute mitral regurgitation)
•High-risk angioplasty
•Unstable angina refractory to medical treatment
•In conjunction with thrombolysis in myocardial infarction
•Bridge to cardiac transplant
K. Bajan, M.D. (*)
Emergency Department, P.D. Hinduja Hospital and Medical Research Centre, Mumbai, India
e-mail: drkhusrav@gmail.com
R. Chawla and S. Todi (eds.), ICU Protocols: A stepwise approach, |
815 |
DOI 10.1007/978-81-322-0535-7_101, © Springer India 2012 |
|
816 |
K. Bajan |
|
|
•Ventricular arrhythmias secondary to ischemia
•High-risk cardiac surgeries
•Patients undergoing noncardiac surgery with high cardiac risk
•Postoperative low cardiac output syndrome
•Weaning from bypass open heart surgery
•Stunned myocardium
•Drug-induced cardiac failure
•Myocardial contusion
•Aortic stenosis
Step 2: Check for any contraindications
•Absolute
–Irreversible brain damage
–Chronic end-stage heart disease without the possibility of heart transplant
–Dissecting aortic aneurysms
•Relative
–Aortic incompetence
–Severe peripheral vascular disease where the decision is based on patient risk–benefit ratio
Step 3: Understand principles of IABP
•The IABP is positioned in the descending thoracic aorta just distal to the left subclavian artery.
•It is connected to an IABP console, which shuttles helium in and out of the balloon, and is timed to inflate and deflate in synchronization with the mechanical cardiac cycle; i.e. the balloon inflates during cardiac diastole and deflates during cardiac systole.
•Inflation at the onset of diastole results in proximal and distal displacement of blood volume in the aorta. This displacement creates elevated pressures by which the coronary artery and systemic perfusion is increased.
•Deflation occurs just prior to the onset of systole. This leads to reduction in the systolic pressure thus decreasing the afterload. Myocardial oxygen demand is decreased as a result of the reduction in systolic pressure and thus improving cardiac output.
Step 4: Techniques and sites of insertion
•It consists of two principal parts:
–The first part is a catheter with two lumens, one for flushing and pressure monitoring and another for delivery of helium gas in a closed balloon (20–50 cm3).
–The second part is a mobile console for delivering helium, controlling balloon inflation and deflation cycling, and displaying pressure waveform and alarms.
•The balloon is inserted from the femoral artery using a Seldinger technique.
•In rare cases, it may be inserted through the axillary artery in patients with severe peripheral arterial disease with bilateral femoral artery occlusion or graft.
101 Intra-aortic Balloon Pump |
817 |
|
|
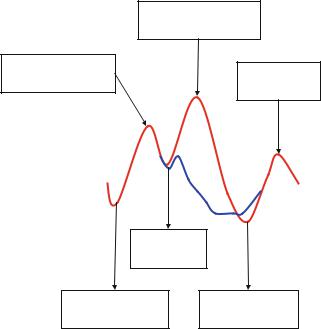
Augmented diastolic pressure
Non-augmented systolic
pressure Reduced systolic pressure
Dicrotic notch
Unassisted aortic enddiastolic pressure
Reduced aortic enddiastolic pressure
Fig. 101.1 IABP waveform (From www.aic.cuhk.edu.hk)
Step 5: Position the balloon
•The tip of the balloon should lie 2–3 cm below the left subclavian artery so that the entire length of the balloon lies in the descending thoracic aorta.
•The tip of the balloon catheter is radiopaque, and hence, a check X-ray should always be taken after insertion to ensure correct balloon placement.
•The balloon should not be too high, so as to avoid blocking the branches of the arch of aorta, especially the left subclavian artery, and should not be too low, so as to avoid blocking the renal arteries.
Step 6: Set cycling time for IABP (Fig. 101.1)
•The mechanical cardiac cycle represented by the arterial pressure waveform is observed to assess appropriate timing.
•Electrocardiographic synchronization may also be done for cycling.
•Inflation of the intra-aortic balloon occurs at the onset of diastole noted by the dicrotic notch on the arterial waveform.
•A sharp deep “V” should be observed when the balloon inflates. As balloon inflates, aortic diastolic pressure is augmented and a second peak is observed. This peak is referred to as diastolic augmentation.
•Diastolic augmentation (30%) is ideally higher than the patient’s systolic pressure and is generated by the displacement of blood volume within the aorta.
818 |
K. Bajan |
|
|
•Deflation occurs at end-diastole prior to the next systole. The precise timing of deflation is found by observing the arterial pressure tracing. The optimal deflation point is selected to achieve the greatest reduction (20%) in the next unassisted systole.
•An effective IABP cycling will result in increase of mean arterial pressure, decrease in heart rate, decrease in pulmonary capillary wedge pressure, and increase in cardiac output.
Step 7: Beware of complications
•Trauma to the arterial wall incurred while inserting and advancing the guidewire or balloon (laceration, dissection, subadventitial hematoma) (1–5%)
•Limb ischemia associated with the position of the balloon catheter, which disappears with catheter removal (5–11%)
•Dislodged thrombus created during balloon removal, resulting in distal embolization (peripheral, renal) (1–5%)
•Hematologic (thrombocytopenia, red blood cell hemolysis, hemorrhage) (1–5%)
•Balloon leak/rupture (1–4%)
•Infection (2–4%)
•Cholesterol embolization—presents with fever, thrombocytopenia, livedo reticularis
Step 8: Know the factors affecting IABP complications
•The following factors increase IABP complications:
–Peripheral artery disease
–Old age
–Female sex
–Diabetes mellitus
–Hypertension
–Prolonged support
–Large catheter size (>9.5 Fr)
–Low cardiac index
–Low body surface area
•The following factors are associated with less IABP complications:
–Decrease in balloon size
–Sheathless technique
Step 9: Take routine care of IABP
•Specialized nursing care with 1:1 nursing every shift is needed to take care of patients.
•The chest X-ray to document position of the catheter tip, which should be at the bifurcation of the left and right main bronchi.
•Three times daily documentation of peripheral pulses.
•Daily measurement of hematocrit, platelet count, and creatinine.
•Anticoagulation parameters.
