
- •ICU Protocols
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1: Airway Management
- •Suggested Reading
- •2: Acute Respiratory Failure
- •Suggested Reading
- •Suggested Reading
- •Website
- •4: Basic Mechanical Ventilation
- •Suggested Reading
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Websites
- •7: Weaning
- •Suggested Reading
- •8: Massive Hemoptysis
- •Suggested Reading
- •9: Pulmonary Thromboembolism
- •Suggested Reading
- •Suggested Reading
- •Websites
- •11: Ventilator-Associated Pneumonia
- •Suggested Readings
- •12: Pleural Diseases
- •Suggested Reading
- •Websites
- •13: Sleep-Disordered Breathing
- •Suggested Reading
- •Websites
- •14: Oxygen Therapy
- •Suggested Reading
- •15: Pulse Oximetry and Capnography
- •Conclusion
- •Suggested Reading
- •Websites
- •16: Hemodynamic Monitoring
- •Suggested Reading
- •Websites
- •17: Echocardiography
- •Suggested Readings
- •Websites
- •Suggested Reading
- •Websites
- •19: Cardiorespiratory Arrest
- •Suggested Reading
- •Websites
- •20: Cardiogenic Shock
- •Suggested Reading
- •21: Acute Heart Failure
- •Suggested Reading
- •22: Cardiac Arrhythmias
- •Suggested Reading
- •Website
- •23: Acute Coronary Syndromes
- •Suggested Reading
- •Website
- •Suggested Reading
- •25: Aortic Dissection
- •Suggested Reading
- •26: Cerebrovascular Accident
- •Suggested Reading
- •Websites
- •27: Subarachnoid Hemorrhage
- •Suggested Reading
- •Websites
- •28: Status Epilepticus
- •Suggested Reading
- •29: Acute Flaccid Paralysis
- •Suggested Readings
- •30: Coma
- •Suggested Reading
- •Suggested Reading
- •Websites
- •32: Acute Febrile Encephalopathy
- •Suggested Reading
- •33: Sedation and Analgesia
- •Suggested Reading
- •Websites
- •34: Brain Death
- •Suggested Reading
- •Websites
- •35: Upper Gastrointestinal Bleeding
- •Suggested Reading
- •36: Lower Gastrointestinal Bleeding
- •Suggested Reading
- •37: Acute Diarrhea
- •Suggested Reading
- •38: Acute Abdominal Distension
- •Suggested Reading
- •39: Intra-abdominal Hypertension
- •Suggested Reading
- •Website
- •40: Acute Pancreatitis
- •Suggested Reading
- •Website
- •41: Acute Liver Failure
- •Suggested Reading
- •Suggested Reading
- •Websites
- •43: Nutrition Support
- •Suggested Reading
- •44: Acute Renal Failure
- •Suggested Reading
- •Websites
- •45: Renal Replacement Therapy
- •Suggested Reading
- •Website
- •46: Managing a Patient on Dialysis
- •Suggested Reading
- •Websites
- •47: Drug Dosing
- •Suggested Reading
- •Websites
- •48: General Measures of Infection Control
- •Suggested Reading
- •Websites
- •49: Antibiotic Stewardship
- •Suggested Reading
- •Website
- •50: Septic Shock
- •Suggested Reading
- •51: Severe Tropical Infections
- •Suggested Reading
- •Websites
- •52: New-Onset Fever
- •Suggested Reading
- •Websites
- •53: Fungal Infections
- •Suggested Reading
- •Suggested Reading
- •Website
- •55: Hyponatremia
- •Suggested Reading
- •56: Hypernatremia
- •Suggested Reading
- •57: Hypokalemia and Hyperkalemia
- •57.1 Hyperkalemia
- •Suggested Reading
- •Website
- •58: Arterial Blood Gases
- •Suggested Reading
- •Websites
- •59: Diabetic Emergencies
- •59.1 Hyperglycemic Emergencies
- •59.2 Hypoglycemia
- •Suggested Reading
- •60: Glycemic Control in the ICU
- •Suggested Reading
- •61: Transfusion Practices and Complications
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Website
- •63: Onco-emergencies
- •63.1 Hypercalcemia
- •63.2 ECG Changes in Hypercalcemia
- •63.3 Superior Vena Cava Syndrome
- •63.4 Malignant Spinal Cord Compression
- •Suggested Reading
- •64: General Management of Trauma
- •Suggested Reading
- •65: Severe Head and Spinal Cord Injury
- •Suggested Reading
- •Websites
- •66: Torso Trauma
- •Suggested Reading
- •Websites
- •67: Burn Management
- •Suggested Reading
- •68: General Poisoning Management
- •Suggested Reading
- •69: Syndromic Approach to Poisoning
- •Suggested Reading
- •Websites
- •70: Drug Abuse
- •Suggested Reading
- •71: Snakebite
- •Suggested Reading
- •72: Heat Stroke and Hypothermia
- •72.1 Heat Stroke
- •72.2 Hypothermia
- •Suggested Reading
- •73: Jaundice in Pregnancy
- •Suggested Reading
- •Suggested Reading
- •75: Severe Preeclampsia
- •Suggested Reading
- •76: General Issues in Perioperative Care
- •Suggested Reading
- •Web Site
- •77.1 Cardiac Surgery
- •77.2 Thoracic Surgery
- •77.3 Neurosurgery
- •Suggested Reading
- •78: Initial Assessment and Resuscitation
- •Suggested Reading
- •79: Comprehensive ICU Care
- •Suggested Reading
- •Website
- •80: Quality Control
- •Suggested Reading
- •Websites
- •81: Ethical Principles in End-of-Life Care
- •Suggested Reading
- •82: ICU Organization and Training
- •Suggested Reading
- •Website
- •83: Transportation of Critically Ill Patients
- •83.1 Intrahospital Transport
- •83.2 Interhospital Transport
- •Suggested Reading
- •84: Scoring Systems
- •Suggested Reading
- •Websites
- •85: Mechanical Ventilation
- •Suggested Reading
- •86: Acute Severe Asthma
- •Suggested Reading
- •87: Status Epilepticus
- •Suggested Reading
- •88: Severe Sepsis and Septic Shock
- •Suggested Reading
- •89: Acute Intracranial Hypertension
- •Suggested Reading
- •90: Multiorgan Failure
- •90.1 Concurrent Management of Hepatic Dysfunction
- •Suggested Readings
- •91: Central Line Placement
- •Suggested Reading
- •92: Arterial Catheterization
- •Suggested Reading
- •93: Pulmonary Artery Catheterization
- •Suggested Reading
- •Website
- •Suggested Reading
- •95: Temporary Pacemaker Insertion
- •Suggested Reading
- •96: Percutaneous Tracheostomy
- •Suggested Reading
- •97: Thoracentesis
- •Suggested Reading
- •98: Chest Tube Placement
- •Suggested Reading
- •99: Pericardiocentesis
- •Suggested Reading
- •100: Lumbar Puncture
- •Suggested Reading
- •Website
- •101: Intra-aortic Balloon Pump
- •Suggested Reading
- •Appendices
- •Appendix A
- •Appendix B
- •Common ICU Formulae
- •Appendix C
- •Appendix D: Syllabus for ICU Training
- •Index
Appendices |
843 |
|
|
Appendix B
Common ICU Formulae
A.Pulmonary equations
1.Arterial oxygen tension (PaO2)
On room air = 100 − 1/3 (age)
On supplemental oxygen = FiO2 (in decimals) × 500, Room air FiO2 = 21% (0.21), FiO2 increases by approximately 4% for each litre increase in Supplemental Oxygen
2.Alveolar gas equation
|
|
æ PaCO2 ö |
||
|
PAO2 |
= (FiO2 ´[Patm - PH2O]) - ç |
|
÷ |
|
|
|||
|
|
è R |
ø |
|
|
PAO2 |
= 150 – (1.25 × PaCO2) |
|
|
|
Normal = 100 mmHg (room air, at sea level) |
|
||
|
where PAO2 = alveolar partial pressure of oxygen |
|||
|
FiO2 = fraction of inspired oxygen (in decimals) |
|||
|
Patm = barometric pressure (760 mmHg at sea level) |
|||
|
PH2O = water vapor pressure (47 mmHg at normal body temperature 37°C) |
|||
|
PaCO2 = partial pressure of carbon dioxide in the blood |
|||
|
R = respiratory quotient, assumed to be 0.8 |
|
||
3. |
AlveolarÐarterial oxygen gradient |
|
||
|
PAO2 − PaO2 |
|
||
|
A-a gradient (on room air) = 2.5 + 0.21 × age in years |
|||
|
Normal value = 3–15 mmHg |
|
||
|
Varies with FiO2 |
|
||
|
For FiO2 = 21%; A-a gradient = 5–15 mmHg |
|||
4. |
For FiO2 = 100%; A-a gradient = <150 mmHg |
|||
PaO2/FiO2 ratio |
|
|||
Normal = 300–500 mmHg
<300 = acute lung injury (previous definition) <200 = ARDS (previous definition)
Berlin definition:
200–300 (with PEEP/CPAP >5) = Mild ARDS <200 (with PEEP >5) = Moderate ARDS <100 (With PEEP >5) = Severe ARDS
5.ArteriolarÐalveolar oxygen ratio = PaO2/PAO2
Normal = 0.77–0.82 (most reliable when FiO2 <0.5)
6.Oxygenation index =
é |
FiO |
2(fraction of inspired O2) |
ù |
êmean airway pressure (cm H2O) ´ |
|
ú ´ 100, |
|
|
PaO2(mm Hg) |
||
ê |
|
ú |
|
ë |
|
|
û |
0 - 25= Good outcome |
|
|
|
>25–40 = severe hypoxemia |
|
|
|
844 |
Appendices |
|
|
7. Static lung compliance (Crs stat)
Tidal volume
Compliancestatic = Plateau pressure - PEEP(positive end - expiratory pressure)
Normal compliance in an intubated patient = 57–85 mL/cm H2O 8. Dynamic lung compliance (Crs dynamic)
Tidal volume
Compliancedynamic = Peek pressure - PEEP(positive end - expiratory pressure)
Variable depending on peak pressure in an intubated patient Lung + Thoracic wall compliance = 0.1 L (100 ml)/cm H2O
9. Airway resistance
Airway resistance = Peak inspiratory pressure - plateau pressure Peak inspiratory flow
Normal resistance in an intubated patient is 4–6 cm H2O/L/s
10.PaCO2–PetCO2 gradient
Normal = 4–5 mmHg
11.Dead space ventilation VD = PaCO2 - PetCO2
VT PaCO2
VD = Dead Space Ventilation = 1ml/lb (2.2 kg) of ideal body wt =150 ml VT = Tidal Volume
PetCO2 = end-tidal CO2 measured by capnography
Normal VD /VT = 0.5 (50%) in mechanically ventilated patients
0.3(30%) in spontaneously breathing patients
12.Shunt equation (right to left shunt) Qs / Qt = (CcO2 - CaO2 )
(CcO2 - CvO2 )
Qs/Qt = shunt fraction
CcO2 is the end-capillary oxygen content (estimated from the PAO2) CaO2 is the arterial oxygen content
CvO2 is the mixed venous oxygen content Normal = 5%
Alternate equation (in patients breathing 100% oxygen for 20 min)
Qs / Qt = 100 ´ (0.0031´ AaG)/ ((.0031´ AaG)+ 5)
13. PaO2 + PaCO2 <150 mmHg at sea level breathing room air
Appendices |
845 |
|
|
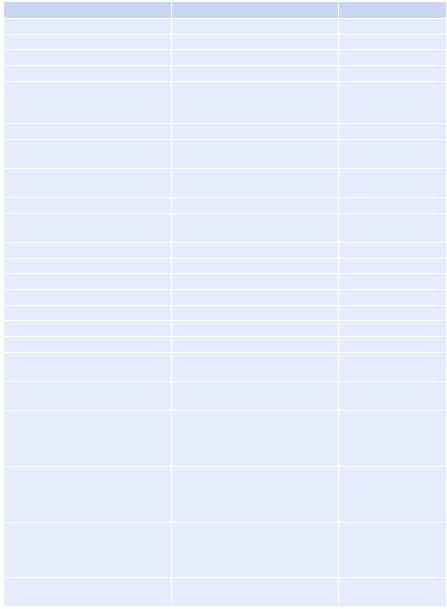
B.Hemodynamic equations
(See Chap. 16)
Parameter |
|
|
Formula |
|
|
Normal range |
||
Pulse pressure |
|
|
Systolic − diastolic BP |
40 mmHg |
||||
Mean arterial pressure (MAP) |
|
1/3 pulse pressure + diastolic BP |
65 mmHg |
|||||
Cardiac output (CO) |
|
|
SV × HR |
|
|
4–7 L/min |
||
Cardiac index (CI) |
|
|
CO/BSA |
|
|
3.5–4.5 L/min/m2 |
||
Stroke volume (SV) |
|
|
CO/HR × 1,000 End diastolic |
60–80 mL |
||||
|
|
|
volume (EDV) (120 ml) – End |
|
||||
|
|
|
systolic volume (ESV) (50 ml) |
|
||||
Stroke volume index (SVI) |
|
|
CI/HR × 1,000, SV/BSA |
33–47 mL/m2/beat |
||||
Systemic vascular resistance |
|
|
[(MAP − CVP)/CO] × 80 |
900–1,200 dyn.s/cm5 |
||||
(SVR) |
|
|
|
|
|
|
|
|
Systemic vascular resistance index |
(MAP – CVP) 80/CI |
1,970–2,390 dyn.s/ |
||||||
(SVRI) |
|
|
|
|
|
|
|
cm5/m2 |
Pulmonary vascular resistance |
|
[(MPAP − PAOP)/CO] × 80 |
80–120 dyn.s/cm5 |
|||||
Pulmonary vascular resistance |
|
[(MPAP − PAOP)/CI] × 80 |
255–285 dyn.s/cm5/m2 |
|||||
index |
|
|
|
|
|
|
|
|
Oxygen delivery (DO2) |
|
|
CO (L) × CaO2 (ml/dl) × 10 |
700–1,400 mL/min |
||||
Oxygen delivery index (DO |
I) |
|
CaO |
2 |
× CI × 10 |
|
500–600 mL/min/m2 |
|
2 |
|
|
|
|
|
|
|
|
Oxygen consumption (VO2) |
|
|
CO (L) × (CaO2 − CvO2) × 10 |
180–280 mL/min |
||||
Oxygen consumption index (VO |
I) |
CI × (CaO |
− CvO |
) × 10 |
120–160 mL/min/m2 |
|||
|
2 |
|
|
|
2 |
2 |
|
|
Oxygen extraction ratio (O2ER) |
|
VO2/DO2 × 100 |
|
25% |
||||
Oxygen extraction index (O2EI) |
|
[(SaO2 − SvO2)/SaO2] × 100 |
20–25% |
|||||
Arterial oxygen content (CaO2) |
|
(1.39 × Hb SaO2) + (0.003 × PaO2) |
17–20 mL/dL |
|||||
Mixed venous oxygen content |
|
(1.39 × Hb × SvO2) + (0.003 × |
12–15 mL/dL |
|||||
(CvO2) |
|
|
PvO2) |
|
|
|
||
A-V oxygen content difference |
|
CaO2 − CvO2 |
|
4–6 mL/dL |
||||
(C(a-v)O2) |
|
|
|
|
|
|
|
|
Systolic pressure variation (SPV) |
[(SPmax − SPmin)/ |
<5 mmHg unlikely to |
||||||
|
|
|
(SPmax + SPmin)/2] × 100 |
be preload responsive |
||||
|
|
|
|
|
|
|
|
>5 mmHg likely to |
|
|
|
|
|
|
|
|
be preload responsive |
Pulse pressure variation (PPV) |
|
(SVmax − SVmin)/ |
<10% unlikely to be |
|||||
|
|
|
[(SVmax + SVmin)/2] × 100 |
preload responsive |
||||
|
|
|
|
|
|
|
|
>13–15% likely to be |
|
|
|
|
|
|
|
|
preload responsive |
Stroke volume variation (SVV) |
|
SV × (MAP − PAWP) × 0.0136 |
<10% unlikely to be |
|||||
|
|
|
|
|
|
|
|
preload responsive |
|
|
|
|
|
|
|
|
>13–15% likely to be |
|
|
|
|
|
|
|
|
preload responsive |
Left ventricular stroke work |
|
|
SVI × (MAP − PAWP) × 0.0136 |
58–104 g m/beat |
||||
(LVSW) |
|
|
|
|
|
|
|
|
846 |
|
Appendices |
|
|
|
(continued) |
|
|
Parameter |
Formula |
Normal range |
Left ventricular stroke work index |
SV × (MPAP − RAP) × 0.0136 |
50–62 g m/m2/beat |
(LVSWI) |
|
|
Right ventricular stroke work |
SVI × (MPAP − RAP) × 0.0136 |
8–16 g m/beat |
(RVSW) |
|
|
Right ventricular stroke work index |
Diastolic BP − PAWP |
5–10 g m/m2/beat |
(RVSWI) |
|
|
Coronary artery perfusion pressure |
|
60–80 mmHg |
(CPP) |
|
|
CVP central venous pressure, MPAP mean pulmonary artery pressure, HR heart rate, BP blood pressure, PAOP pulmonary artery occlusion pressure, SaO2 arterial oxygen saturation, SvO2 mixed venous oxygen saturation, PaO2 arterial oxygen partial pressure, PvO2, mixed venous oxygen partial pressure
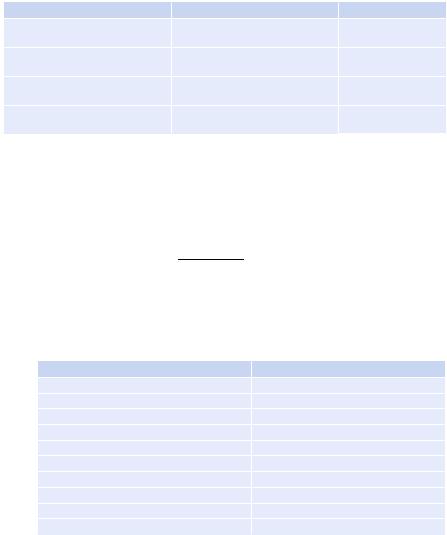
C.AcidÐbase equations
1.Validity of the data
Henderson’s equation
H + ´ HCO3 = 24
PaCO2
H+ = hydrogen ion
HCO3 = Bicarbonate
PaCO2 = Partial pressure of carbon dioxide
pH |
[H+] (mmol/L) |
7.60 |
25 |
7.55 |
28 |
7.50 |
32 |
7.45 |
35 |
7.40 |
40 |
7.35 |
45 |
7.30 |
50 |
7.25 |
56 |
7.20 |
63 |
7.15 |
71 |
Rule of thumb: H+ = 80 minus the last two digits of pH after decimal (for pH 7.20–7.50)
For example, pH 7.35: H+ = 80–35 = 45
2.Respiratory acidosis or respiratory alkalosis
•Acute respiratory acidosis or alkalosis: DpH = 0.008 × DPaCO2 (from 40)
•Chronic respiratory acidosis or alkalosis: DpH = 0.003 × DPaCO2 (from 40)
•Acute respiratory acidosis = ↑PaCO2 10 mmHg = ↑HCO3 1 mmol/L
•Chronic respiratory acidosis = ↑PaCO2 10 mmHg = ↑HCO3 3 mmol/L
•Acute respiratory alkalosis = ↓PaCO2 10 mmHg = ↓HCO3 2 mmol/L
•Chronic respiratory alkalosis = ↓PaCO2 10 mmHg = ↓HCO3 4 mmol/L
• |
Acute respiratory acidosis or alkalosis: SBE (standard base excess) = zero |
• |
Chronic respiratory acidosis or alkalosis: Change in bicarbonate= 0.4×SBE |
Appendices |
847 |
|
|
3.Metabolic acidosis
•Predicted PaCO2 = 1. 5 × [HCO3− + 8] ±2
•Change in bicarbonate = change in standard base excess (SBE)
•1 mEq/L fall in HCO3 = 1.2 mmHg fall in PaCO2
•Bicarbonate deficit (mEq/L) = [0.5 × body weight (kg) × (24 − [HCO3−])] Rule of thumb: Expected PaCO2 = the last two digits of pH after decimal
4.Metabolic alkalosis
•Predicted PaCO2 = 0.7 × [HCO3 + 21] ± 2
•Change in bicarbonate = 0.6 × standard base excess (SBE)
•1 mEq/L rise in HCO3 = 0.7 mmHg rise in PaCO2
•Bicarbonate excess [0.4 × body weight (kg) × ([HCO3−] − 24)]
Rule of thumb: Expected PaCO2 = the last two digits of pH after decimal
5.Blood anion gap
•Anion gap (AG) = Na+ − (Cl− + HCO3−)
– Normal value: 10 ± 4 mmol/L
•Correction for albumin: For every change (increased or decreased) of 1 g/dL in albumin, a change of 2.5 mmol/L in the anion gap
•Correction for pH: In acidosis, decrease by 2 mmol/L; in alkalosis, increase by 2 mmol/L
6.Delta gap/Delta ratio
•Delta gap = delta AG − delta HCO3−
•Delta ratio = delta AG/delta HCO3
•Where Delta AG = patient’s AG − 12 mEq/L {normal AG}
•Delta HCO3− = 24 mEq/L {normal HCO3−} − patient’s HCO3
• Normal delta gap (in pure anion gap metabolic acidosis) = 0 ± 6
•Normal delta ratio =1.1
–High delta gap/delta ratio > 1 signifies a concomitant metabolic alkalosis or chronic respiratory acidosis.
–Low delta gap/delta ratio < 1 signifies a concomitant normal anion gap metabolic acidosis or chronic respiratory alkalosis.
7.Urine anion gap (UAG)
•UAG (mmol/L) = urine [(Na + K) − Cl]
–Normal: usually zero or positive
–Nonanion gap metabolic acidosis due to gastrointestinal loss: UAG negative
–Nonanion gap metabolic acidosis due to renal cause (renal tubular acidosis): UAG positive
8.Stewarts approach
•Strong ion difference (SID): [Na+]+[K+]+[Ca2+]+[Mg2+]−[Cl−]−[lactate]
–Normal value: 40 mEq/L
–Increase in SID = alkalosis (increase in pH)
–Decrease in SID = acidosis (decrease in pH)
•Strong ion gap (SIG): SID − SIDeff
–SIDeff = effective strong ion difference (depends on pH, albumin, phosphate)
848 |
Appendices |
|
|
–12.2×PCO2/(10 − pH) + [albumin] × (0.123 × pH − 0.631) + [PO4−] × (0.3 09 × pH − 0.469)
–Normal SIG = 0
–Positive SIG = Increase in organic acid D. Electrolyte equations
1.Hyponatremia
•Sodium deficit = (desired [Na+] − current [Na+]) × 0.6 × body weight in kg
•Increase in serum sodium = (infusate sodium − serum sodium)/[(0.6 × body weight) + 1]
Rule of thumb:
–For hypertonic (3%) saline, infusion rate (mL/h) = weight (kg) × desired rate of correction (mEq/h)
–e.g. to correct sodium by 0.5 meq/l/hr, the desired rate of 3% saline infusion in a 60 kg man would be = 60 × 0.5 = 30 ml/hr
–0.9% NaCl corrects at 1–2 mmol/L for every 1 L NaCl
•Calculated urine osmolarity=the last two digits of urine-specific gravity×30
2.Hypernatremia
|
æ plasmaNa+ |
ö |
||
• |
Free water deficit (L) = 0.4 ´ body weight ´ ç |
|
-1÷ |
|
140 |
||||
|
è |
ø |
||
3.Correction sodium for hyperglycemia
•For each 100 mg/dL increase in blood glucose above 200 mg/dL, serum sodium decreases by 2.4 mEq/L.
4.Serum osmolality
•Calculated Sosm = (2 × serum [Na]) + [glucose, in mg/dL]/18 + [blood urea nitrogen, in mg/dL]/2.8
•Calculated Sosm with standard units (mmol/L) = (2 × serum [Na]) + [glucose] + [urea]
–Normal value = 270 and 290 mOsm/kg H2O
•Osmolar gap = measured osmolality − calculated osmolality
–Normal value = <10 mOsm/kg H2O
5.Corrected calcium
• Corrected calcium (mg/dL) = measured total calcium (mg/dL) + [0.8 × (4.0 − albumin)]
•Corrected calcium (mmol/L) = measured total calcium (mmol/L)+ [0.02 × (Normal albumin [40 g/l] – patients albumin)]
E. Renal equations
1.Measured creatinine clearance (CCr) L/day
•[24-h urine creatinine (mg/dL) × 24-h urine volume (L/day)]/serum creatinine (mg/dL)
•CCr ml/min = [(CCr L/day × 1000 ml/L)]/1440 min/day
•CCr ml/min × 1.73/BSA = CCr ml/min/1.73 sq.m
–Normal values = 95 ± 20 mL/min per 1.73 m2 in women and 120 ± 25 mL/ min per 1.73 m2 in men

Appendices |
849 |
|
|
2. Estimated creatinine clearance (CockroftÐGault equation)
• (140 - Age in years × Weight in kg) / Serum creatinine in mg/dl × 72
• For female patient multiply with 0.85
3.Fractional excretion of sodium (FENa+)
[UrineNa+ ] ´[plasma creatinine]
[Urine creatinine] ´[plasmaNa+ ]
–Normal value = <1
4.Fractional excretion of urea (FEurea)
[Urineurea] ´[plasma creatinine]
[BUN] ´[urinecreatinine]
– <35 in prerenal azotemia, 50–65 in acute tubular necrosis
F.Nutrition equations
1.Ideal or predicted body weight (IBW)
• Male IBW (kg) = 50 + (0.91 × (height in cm − 152.4))
• Male IBW (kg) = 50 kg for 5 ft; add 2.3 kg for every 1 in. above 5 ft
•Female IBW (kg) = 45.5 + (0.91 × (height in cm − 152.4))
•Female IBW (kg) = 45.5 kg for 5 ft; add 2.3 kg for every 1 in. above 5 ft
2.HarrisÐBenedict equation with LongÕs modiÞcation (calories requirement)
• For women, basal metabolic rate (BMR) = 65.5 + (9.6 × weight in kg) + (1.8 × height in cm) − (4.7 × age in years)
•For men, BMR = 66 + (13.7 × weight in kg) + (5 × height in cm) − (6.8 × age in years)
•Actual energy needs=BMR×AF×IF (AF, activity factor; IF, injury factor)
•Activity factor (AF): Confined to bed = 1.2; out of bed = 1.3
• Injury factor (IF): Minor surgery = 1.2; skeletal trauma = 1.3; major sepsis = 1.6; severe burn = 2.1
•Normal calories requirement = 25–30 kcal/kg of predicted body weight
3.Protein requirement
•1 g of nitrogen = 6.25 g of protein
•Non-protein calories (NPC)–nitrogen ratio = 150:1
•Nitrogen balance = (protein intake/6.25) − (24-h urinary urea nitrogen + 4)
•Negative nitrogen balance >5 = severe stress
• 1 g of nitrogen loss = 30 g lean body mass lost
•1 g of glucose = 4 kcal
•1 g of protein = 4 kcal
•1 g of lipid = 9 kcal
•Protein loss in dialysis = 4–6 g/h in hemodialysis; 40–60 g in peritoneal dialysis
4.Respiratory quotient (RQ):
•Carbon dioxide production (VCO2)/oxygen consumption (VO2)
•Normal value on balanced diet = 0.7–1.0
•> 1: Excess carbohydrate
•<0.7: Excess fat

850 |
Appendices |
|
|
G.Intra-abdominal pressure equation
•Abdominal perfusion pressure (APP) = mean arterial pressure (MAP) − IAP (intra-abdominal pressure)
•Normal intra-abdominal pressure = 5–7 mmHg
•Filtration gradient (FG) = glomerular filtration pressure (GFP) − proximal tubular pressure (PTP) = MAP − 2 × IAP
H.Statistical equations
•Sensitivity: True positives/(true positive [TP] + false negative [FN])
•Specificity: True negative/(true negative [TN] + false positive [FP])
•Positive predictive value: True positive/ (true positive + false positive)
•Negative predictive value: True negative/(true negative + false negative)
•Positive likelihood ratio (LR+): sensitivity/(1 − specificity)
•Negative likelihood ratio (LR−): (1 − sensitivity)/specificity
•Prevalence (pretest probability): (TP + FN)/(TP + FP + TN + FN)
•Pretest odds: Prevalence/(1 − prevalence)
•Posttest odds: Pretest odds × LR
•Posttest probability: Posttest odds/(posttest odds + 1)
•Event rate (ER): Total events/total subjects (event + nonevent)
•Absolute risk reduction (ARR): Control event rate (CER) − experimental event rate (EER)
•Relative risk reduction (RRR): (CER − EER)/CER
•Relative risk (RR): EER/CER
•Odds ratio: (experimental event [EE]/experimental nonevent [EN])/(control event [CE]/control nonevent [CN])
•Number needed to treat (NNT): 1/ARR
•Number needed to harm (NNH): 1/(CER − EER)
• |
Rate of Type I error = Number of False positives = Alpha |
• |
Rate of Type II error = Number of False negatives = Beta |
•Power of a test = (1-Beta) I. Neurology equations
•CBF = (CAP − JVP) ÷ CVR
(CBF, cerebral blood flow; CAP, carotid artery pressure; JVP, jugular venous pressure; CVR, cerebrovascular resistance)
•CPP = MAP − ICP
(CPP, cerebral perfusion pressure; MAP, mean arterial pressure; ICP, intracranial pressure)
– Keep CPP between 60 and 75 mmHg
•Increased WBC in traumatic tap:
Rule of thumb: Subtract one WBC for every 500–1,500 RBCs (if peripheral WBC is normal)
J.Hematology equation
•ANC = WBC × [(segs/100) + (bands/100)] (ANC, absolute neutrophil count)
•Corrected reticulocyte count (CRC)= reticulocytes (%) ´ Hct (L / L)
0.45L/L
