
- •ICU Protocols
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1: Airway Management
- •Suggested Reading
- •2: Acute Respiratory Failure
- •Suggested Reading
- •Suggested Reading
- •Website
- •4: Basic Mechanical Ventilation
- •Suggested Reading
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Websites
- •7: Weaning
- •Suggested Reading
- •8: Massive Hemoptysis
- •Suggested Reading
- •9: Pulmonary Thromboembolism
- •Suggested Reading
- •Suggested Reading
- •Websites
- •11: Ventilator-Associated Pneumonia
- •Suggested Readings
- •12: Pleural Diseases
- •Suggested Reading
- •Websites
- •13: Sleep-Disordered Breathing
- •Suggested Reading
- •Websites
- •14: Oxygen Therapy
- •Suggested Reading
- •15: Pulse Oximetry and Capnography
- •Conclusion
- •Suggested Reading
- •Websites
- •16: Hemodynamic Monitoring
- •Suggested Reading
- •Websites
- •17: Echocardiography
- •Suggested Readings
- •Websites
- •Suggested Reading
- •Websites
- •19: Cardiorespiratory Arrest
- •Suggested Reading
- •Websites
- •20: Cardiogenic Shock
- •Suggested Reading
- •21: Acute Heart Failure
- •Suggested Reading
- •22: Cardiac Arrhythmias
- •Suggested Reading
- •Website
- •23: Acute Coronary Syndromes
- •Suggested Reading
- •Website
- •Suggested Reading
- •25: Aortic Dissection
- •Suggested Reading
- •26: Cerebrovascular Accident
- •Suggested Reading
- •Websites
- •27: Subarachnoid Hemorrhage
- •Suggested Reading
- •Websites
- •28: Status Epilepticus
- •Suggested Reading
- •29: Acute Flaccid Paralysis
- •Suggested Readings
- •30: Coma
- •Suggested Reading
- •Suggested Reading
- •Websites
- •32: Acute Febrile Encephalopathy
- •Suggested Reading
- •33: Sedation and Analgesia
- •Suggested Reading
- •Websites
- •34: Brain Death
- •Suggested Reading
- •Websites
- •35: Upper Gastrointestinal Bleeding
- •Suggested Reading
- •36: Lower Gastrointestinal Bleeding
- •Suggested Reading
- •37: Acute Diarrhea
- •Suggested Reading
- •38: Acute Abdominal Distension
- •Suggested Reading
- •39: Intra-abdominal Hypertension
- •Suggested Reading
- •Website
- •40: Acute Pancreatitis
- •Suggested Reading
- •Website
- •41: Acute Liver Failure
- •Suggested Reading
- •Suggested Reading
- •Websites
- •43: Nutrition Support
- •Suggested Reading
- •44: Acute Renal Failure
- •Suggested Reading
- •Websites
- •45: Renal Replacement Therapy
- •Suggested Reading
- •Website
- •46: Managing a Patient on Dialysis
- •Suggested Reading
- •Websites
- •47: Drug Dosing
- •Suggested Reading
- •Websites
- •48: General Measures of Infection Control
- •Suggested Reading
- •Websites
- •49: Antibiotic Stewardship
- •Suggested Reading
- •Website
- •50: Septic Shock
- •Suggested Reading
- •51: Severe Tropical Infections
- •Suggested Reading
- •Websites
- •52: New-Onset Fever
- •Suggested Reading
- •Websites
- •53: Fungal Infections
- •Suggested Reading
- •Suggested Reading
- •Website
- •55: Hyponatremia
- •Suggested Reading
- •56: Hypernatremia
- •Suggested Reading
- •57: Hypokalemia and Hyperkalemia
- •57.1 Hyperkalemia
- •Suggested Reading
- •Website
- •58: Arterial Blood Gases
- •Suggested Reading
- •Websites
- •59: Diabetic Emergencies
- •59.1 Hyperglycemic Emergencies
- •59.2 Hypoglycemia
- •Suggested Reading
- •60: Glycemic Control in the ICU
- •Suggested Reading
- •61: Transfusion Practices and Complications
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Website
- •63: Onco-emergencies
- •63.1 Hypercalcemia
- •63.2 ECG Changes in Hypercalcemia
- •63.3 Superior Vena Cava Syndrome
- •63.4 Malignant Spinal Cord Compression
- •Suggested Reading
- •64: General Management of Trauma
- •Suggested Reading
- •65: Severe Head and Spinal Cord Injury
- •Suggested Reading
- •Websites
- •66: Torso Trauma
- •Suggested Reading
- •Websites
- •67: Burn Management
- •Suggested Reading
- •68: General Poisoning Management
- •Suggested Reading
- •69: Syndromic Approach to Poisoning
- •Suggested Reading
- •Websites
- •70: Drug Abuse
- •Suggested Reading
- •71: Snakebite
- •Suggested Reading
- •72: Heat Stroke and Hypothermia
- •72.1 Heat Stroke
- •72.2 Hypothermia
- •Suggested Reading
- •73: Jaundice in Pregnancy
- •Suggested Reading
- •Suggested Reading
- •75: Severe Preeclampsia
- •Suggested Reading
- •76: General Issues in Perioperative Care
- •Suggested Reading
- •Web Site
- •77.1 Cardiac Surgery
- •77.2 Thoracic Surgery
- •77.3 Neurosurgery
- •Suggested Reading
- •78: Initial Assessment and Resuscitation
- •Suggested Reading
- •79: Comprehensive ICU Care
- •Suggested Reading
- •Website
- •80: Quality Control
- •Suggested Reading
- •Websites
- •81: Ethical Principles in End-of-Life Care
- •Suggested Reading
- •82: ICU Organization and Training
- •Suggested Reading
- •Website
- •83: Transportation of Critically Ill Patients
- •83.1 Intrahospital Transport
- •83.2 Interhospital Transport
- •Suggested Reading
- •84: Scoring Systems
- •Suggested Reading
- •Websites
- •85: Mechanical Ventilation
- •Suggested Reading
- •86: Acute Severe Asthma
- •Suggested Reading
- •87: Status Epilepticus
- •Suggested Reading
- •88: Severe Sepsis and Septic Shock
- •Suggested Reading
- •89: Acute Intracranial Hypertension
- •Suggested Reading
- •90: Multiorgan Failure
- •90.1 Concurrent Management of Hepatic Dysfunction
- •Suggested Readings
- •91: Central Line Placement
- •Suggested Reading
- •92: Arterial Catheterization
- •Suggested Reading
- •93: Pulmonary Artery Catheterization
- •Suggested Reading
- •Website
- •Suggested Reading
- •95: Temporary Pacemaker Insertion
- •Suggested Reading
- •96: Percutaneous Tracheostomy
- •Suggested Reading
- •97: Thoracentesis
- •Suggested Reading
- •98: Chest Tube Placement
- •Suggested Reading
- •99: Pericardiocentesis
- •Suggested Reading
- •100: Lumbar Puncture
- •Suggested Reading
- •Website
- •101: Intra-aortic Balloon Pump
- •Suggested Reading
- •Appendices
- •Appendix A
- •Appendix B
- •Common ICU Formulae
- •Appendix C
- •Appendix D: Syllabus for ICU Training
- •Index
Acute Heart Failure |
21 |
|
|
Rajesh Chawla and Rajeeve Kumar Rajput |
|
A 60-year-old male patient, a known case of coronary artery disease (CAD) and type 2 diabetes, presented with history of acute onset of breathlessness and orthopnea for 2 days. On examination, he was found to have tachycardia, tachypnea, and bilateral basal crepitations, and SpO2 was 87%.
Heart failure is defined as a pathophysiological state in which heart is unable to pump blood at a rate commensurate with the requirements of the metabolic demand.
New York Heart Association (NYHA) classification of heart failure comprises of four classes which has therapeutic and prognostic significance.
Class I—patients have no limitation of physical activity. Class II—patients have slight limitation of physical activity.
Class III—patients have marked limitation of physical activity.
Class IV—patients have symptoms even at rest and are unable to carry on any physical activity without discomfort.
The management of heart failure comprises of stabilizing the clinical state of the patient, making a diagnosis, detect etiology and initiate definitive treatment.
R. Chawla, M.D., F.C.C.M. (*)
Department of Respiratory, Critical Care & Sleep Medicine, Indraprastha Apollo Hospitals, New Delhi, India
e-mail: drchawla@hotmail.com
R.K. Rajput, M.D., D.M.
Department of Cardiology, Indraprastha Apollo Hospitals, New Delhi, India
R. Chawla and S. Todi (eds.), ICU Protocols: A stepwise approach, |
165 |
DOI 10.1007/978-81-322-0535-7_21, © Springer India 2012 |
|
166 |
R. Chawla and R.K. Rajput |
|
|
Step 1: Initial resuscitation (see Chap. 78)
•Administer oxygen in high concentration to maximize tissue oxygenation as hypoxia can depress myocardial function.
•Assess the response clinically, by SpO2 and arterial blood gas assessment.
•Continuous positive airway pressure (CPAP) or noninvasive ventilation (NIV) is indicated if the patient does not respond to oxygen alone.
•With aggressive conservative management, intubation can be avoided in many patients of heart failure presenting with respiratory distress.
•If poor gas exchange is present despite conservative management, the patient should be intubated and initiated on invasive ventilation.
•Invasive ventilation helps in reducing oxygen demand and reverses respiratory muscle fatigue.
•Assess the circulatory status by pulse and blood pressure and the status of major organ perfusion.
•Assess the volume status, whether volume depleted or congested.
•Some patients with pulmonary edema are centrally fluid depleted. It may be very difficult to assess this in critically ill patients, so invasive monitoring may be required.
•Initiate inotropes or vasopressors or advanced cardiac support based on severity of the hemodynamic compromise.
•Therapy should be directed to treat the cause of heart failure to improve circulation and optimize BP and cardiac output.
Step 2: Take clinical history
•Clinical history should be obtained to find out the cause of acute heart failure.
•History of cardinal cardiac symptoms such as dyspnea, angina, palpitation syncope, fatigue, weakness, swelling of ankles or abdomen, and previous cardiac surgery.
•Make an attempt to detect whether acute heart failure is due to acute coronary syndrome, which requires urgent revascularization.
•Look for precipitating conditions such as severe anemia, sepsis, severe hypertension, arrhythmia, thyroid disorders, medical, and dietary noncompliance.
Step 3: Do quick physical examination
Look for signs of congestion/cardiac involvement:
•Raised jugular venous pressure, peripheral edema, ascites, hepatomegaly
•Displaced apical pulse due to cardiomegaly
•Gallop rhythm
•Cardiac murmur
Look for signs of low cardiac output:
•Hypotension
•Level of consciousness, confusion
•Cool peripheries and low volume carotid pulse
21 Acute Heart Failure |
|
167 |
|
|
|
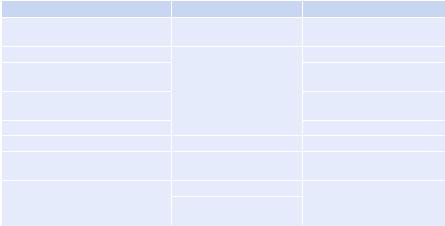
Table 21.1 Types of heart failure |
|
|
Forward |
Backward left |
Backward right |
Fatigue or weakness, confusion, |
Mild exertion dyspnea, |
Dyspnea not prominent |
drowsiness |
orthopnea |
|
Pallor, peripheral cyanosis |
Pulmonary edema |
Acute tricuspid regurgitation |
Cold, clammy skin |
|
V wave on central venous |
|
|
pressure trace |
Low BP, oliguria |
|
Hemodynamic compromise, |
|
|
arrhythmia |
Cardiogenic shock |
|
Cardiogenic shock |
Cause |
Cause |
Cause |
Acute myocardial infarction (MI), |
Acute valvular disease |
Acute pulmonary embolism |
acute valvular dysfunction |
|
|
Pulmonary embolism, cardiac |
Acute MI |
Right ventricular infarction |
tamponade |
Sudden rise in BP (flash |
|
|
pulmonary edema) |
|
•Tachycardia or bradycardia
•Decreased urine output
•Peripheral cyanosis
The signs may also depend on whether it is rightor left-sided heart failure,
systolic or diastolic failure, or forward or backward failure (Table 21.1).
Step 4: Send investigations
•ECG may suggest acute MI, pulmonary embolism, and arrhythmia
•Chest radiograph:
–Cardiac size, shape
–Presence of pulmonary congestion—alveolar and interstitial edema
–Rule out pneumothorax, pneumonitis
•Hemogram
•Urea, electrolytes
•Arterial blood gases with lactate levels
•Blood glucose
•Coagulation profile—prothrombin time/partial thromboplastin time
•Cardiac markers—CPK, CPK-MB, troponins T and I
•B-type natriuretic peptide of less than 100 pg/mL rules out heart failure
•Liver function tests
•Echocardiography most helpful—global and regional LV function, valvular abnormalities, diastolic function, diagnostic of cardiac tamponade and RV dysfunction due to pulmonary embolism
•Invasive hemodynamic monitoring—cardiogenic shock, unstable hemodynamics, poor response to therapy
•Holter monitoring, TEE (Trans esophageal echocardiography) in selected cases
•Cardiac catheterization, coronary angiography
168 |
R. Chawla and R.K. Rajput |
|
|
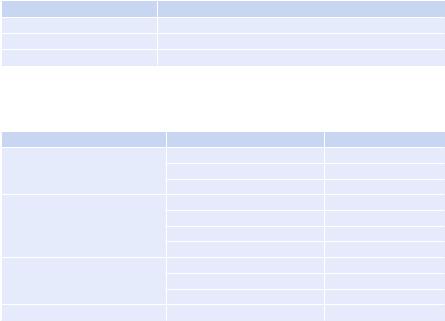
Table 21.2 Vasodilators—doses |
|
Vasodilator |
Dosing |
Nitroglycerine |
Start 10–20 mg/min, increase up to 200 mg/min |
Nitroprusside |
Start with 0.1 mg/Kg/min and increase up to 5 mg/Kg/min |
Nesiritide |
Bolus 2 mg/Kg + infusion 0.01 mcg/Kg/min |
Table 21.3 Diuretics—doses and clinical indications |
|
|
Fluid retention |
Diuretic |
Daily dose (mg) |
Moderate |
Furosemide |
20–40 |
|
Bumetanide |
0.5–1 |
|
Torsemide |
10–20 |
Severe |
Furosemide |
40–100 |
|
Furosemide infusion |
(5–40 mg/h) |
|
Bumetanide |
1–10 |
|
Torsemide |
20–100 |
Refractory to loop diuretic |
Add hydrochlorothiazide |
50–100 |
|
Metolazone |
2.5–10 |
|
Spironolactone |
25–50 |
With alkalosis |
Acetazolamide |
250–375 |
Step 5: Specific treatment
1.Reduce demand
•Control heart rate.
•Relieve anxiety—provide reassurance and anxiolytics.
•Prevent and treat pain—1.5–3 mg morphine or 50–100 mcg fentanyl IV can be given.
•Use b-blockers cautiously in selective cases. Carvedilol (3.125–25 mg) or metoprolol (12.5–50 mg) can be used. Start with low dose and titrate gradually to higher dose to achieve the heart rate of less than 60/min.
•The patient on chronic b-blocker should have their dose reduced during acute decompensated heart failure.
2.Decrease preload
•Vasodilator—nitroglycerine, isosorbide nitrate (Table 21.2)
•Diuretics (Table 21.3)
•Fluid restriction
•Mechanical ventilation
•In refractory volume overload state along with renal compromise, continuous ultrafiltration (SCUF) should be considered
3.Reduce afterload
•Control of blood pressure—nitroglycerine, nitroprusside
•Inotropes—dobutamine
•Intra-aortic balloon pump (IABP)—specially in acute coronary syndrome
21 Acute Heart Failure |
169 |
|
|
||
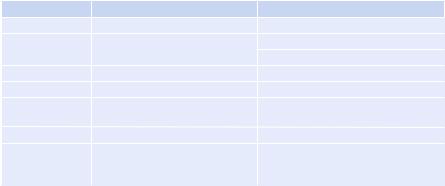
Table 21.4 Inotropes—mode of administration and doses |
||
|
Bolus |
Infusion rate |
Dobutamine |
No |
2–20 mg/Kg/min |
Dopamine |
No |
3–5 mg/Kg/min: inotropic |
|
|
>5 mg/Kg/min: vasopressor |
Milrinone |
25–75 mg/Kg over 10–20 min |
0.375–0.75 mg/Kg/min |
Enoximone |
90 mcg/Kg/min over 10–30 mins |
5–20 mcg/Kg/min |
Levosimendan |
12 mg/Kg over 10 min (optional) |
0.1 mg/Kg/min which can be decreased |
|
|
to 0.05 or increased to 0.2 mg/Kg/min |
Norepinephrine |
No |
0.2–1.0 mg/Kg/min |
Epinephrine |
Bolus: 1 mg can be given IV |
0.05–0.5 mg/Kg/min |
|
during resuscitation, repeated |
|
|
every 3–5 min |
|
4.Increase contractility (Table 21.4)
•Dopaminergic agonists—dopamine, dobutamine
•Sympathomimetic agents—adrenaline, norepinephrine
•Phosphodiesterase inhibitors—amrinone, milrinone:
–Mainly useful in patients with refractory acute severe heart failure
–Postoperative decompensation
•Levosimendan (calcium channel sensitizer)
•Nesiritide
•In patients with severe hypotension, use vasopressor judiciously to maintain adequate perfusion pressure and taper them off at the earliest.
5.Optimize blood supply—early reperfusion therapy
•Thrombolytic agents, streptokinase, rTPA, tenecteplase
•Percutaneous coronary intervention (PCI)
6.Ensure adequate oxygen
•Face mask/noninvasive ventilation or CPAP
•Intubation and ventilation in refractory heart failure:
–Mechanical assist devices—IABP
–Left or right ventricular assist devices in refractory cases
•Early referral to appropriate centers should be considered
Step 6: General care
•Thromboprophylaxis
•Adequate nutrition
•Correct electrolyte imbalance
•Prevent and treat infection
Step 7: Treat the specific cause
•Pulmonary embolism—thrombolysis or surgical thrombectomy if indicated (see Chap. 5)
•Valvular defect—repair or replace
•Coronary artery disease—CABG or PTCA
•Cardiac tamponade—urgent pericardiocentesis
170 |
R. Chawla and R.K. Rajput |
|
|
The patient with acute shortness of breath, initial clinical evaluation
Abnormal ECG? X-ray chest—cardiomegaly
Known heart disease or chronic HF Gallop,cardiac murmur, bilateralcrepts
Yes
Evaluate by echocardiography
Abnormal
Heart failure confirmed
Specific investigations to assess type, severity, and etiology
No |
Consider noncardiac cause |
|
Pulmonary disease |
|
|
Normal
Normal
Increased |
BNP |
|
|
Treat Heart failure
(Refer to Figure 2)
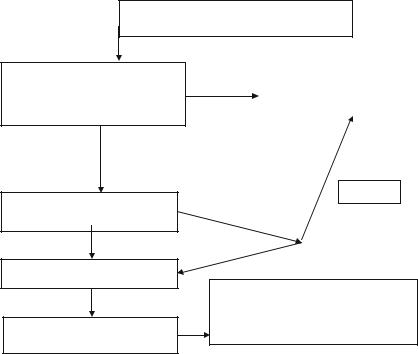
Fig. 21.1 Initial assessment of the patient presenting with acute dyspnea
Step 8: Long-term care
•Advise regarding diet, salt intake, rehabilitation.
•Essential medication known to improve survival like b-blockers, ACE inhibitors or ARBs, and mineralocorticoid inhibitors should be started.
•Statins should be prescribed specially for CAD patients.
•Regular follow-up is very critical.
•Patients who remain symptomatic (NYHA III, IV) despite optimal medical treatment and have LVEF less than 30% with wide QRS more than 120 ms are candidates for biventricular pacing.
•AICD implantation is recommended to prevent sudden cardiac death in the following conditions:
–All patients with LVEF less than 30% in nonischemic cardiomyopathy.
–LVEF less than 30% at least 6 weeks after myocardial infarction.
–Secondary prevention: Episodes of Prior Ventricular fibrillation/ventricular tachycardia and resuscitated sudden cardiac arrest.
•Patients who are very symptomatic despite best medical treatment are candidate for cardiac transplantation or assist devices.
An approach to the management of heart failure is summarized in Figs. 21.1 and
21.2.
