
- •ICU Protocols
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1: Airway Management
- •Suggested Reading
- •2: Acute Respiratory Failure
- •Suggested Reading
- •Suggested Reading
- •Website
- •4: Basic Mechanical Ventilation
- •Suggested Reading
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Websites
- •7: Weaning
- •Suggested Reading
- •8: Massive Hemoptysis
- •Suggested Reading
- •9: Pulmonary Thromboembolism
- •Suggested Reading
- •Suggested Reading
- •Websites
- •11: Ventilator-Associated Pneumonia
- •Suggested Readings
- •12: Pleural Diseases
- •Suggested Reading
- •Websites
- •13: Sleep-Disordered Breathing
- •Suggested Reading
- •Websites
- •14: Oxygen Therapy
- •Suggested Reading
- •15: Pulse Oximetry and Capnography
- •Conclusion
- •Suggested Reading
- •Websites
- •16: Hemodynamic Monitoring
- •Suggested Reading
- •Websites
- •17: Echocardiography
- •Suggested Readings
- •Websites
- •Suggested Reading
- •Websites
- •19: Cardiorespiratory Arrest
- •Suggested Reading
- •Websites
- •20: Cardiogenic Shock
- •Suggested Reading
- •21: Acute Heart Failure
- •Suggested Reading
- •22: Cardiac Arrhythmias
- •Suggested Reading
- •Website
- •23: Acute Coronary Syndromes
- •Suggested Reading
- •Website
- •Suggested Reading
- •25: Aortic Dissection
- •Suggested Reading
- •26: Cerebrovascular Accident
- •Suggested Reading
- •Websites
- •27: Subarachnoid Hemorrhage
- •Suggested Reading
- •Websites
- •28: Status Epilepticus
- •Suggested Reading
- •29: Acute Flaccid Paralysis
- •Suggested Readings
- •30: Coma
- •Suggested Reading
- •Suggested Reading
- •Websites
- •32: Acute Febrile Encephalopathy
- •Suggested Reading
- •33: Sedation and Analgesia
- •Suggested Reading
- •Websites
- •34: Brain Death
- •Suggested Reading
- •Websites
- •35: Upper Gastrointestinal Bleeding
- •Suggested Reading
- •36: Lower Gastrointestinal Bleeding
- •Suggested Reading
- •37: Acute Diarrhea
- •Suggested Reading
- •38: Acute Abdominal Distension
- •Suggested Reading
- •39: Intra-abdominal Hypertension
- •Suggested Reading
- •Website
- •40: Acute Pancreatitis
- •Suggested Reading
- •Website
- •41: Acute Liver Failure
- •Suggested Reading
- •Suggested Reading
- •Websites
- •43: Nutrition Support
- •Suggested Reading
- •44: Acute Renal Failure
- •Suggested Reading
- •Websites
- •45: Renal Replacement Therapy
- •Suggested Reading
- •Website
- •46: Managing a Patient on Dialysis
- •Suggested Reading
- •Websites
- •47: Drug Dosing
- •Suggested Reading
- •Websites
- •48: General Measures of Infection Control
- •Suggested Reading
- •Websites
- •49: Antibiotic Stewardship
- •Suggested Reading
- •Website
- •50: Septic Shock
- •Suggested Reading
- •51: Severe Tropical Infections
- •Suggested Reading
- •Websites
- •52: New-Onset Fever
- •Suggested Reading
- •Websites
- •53: Fungal Infections
- •Suggested Reading
- •Suggested Reading
- •Website
- •55: Hyponatremia
- •Suggested Reading
- •56: Hypernatremia
- •Suggested Reading
- •57: Hypokalemia and Hyperkalemia
- •57.1 Hyperkalemia
- •Suggested Reading
- •Website
- •58: Arterial Blood Gases
- •Suggested Reading
- •Websites
- •59: Diabetic Emergencies
- •59.1 Hyperglycemic Emergencies
- •59.2 Hypoglycemia
- •Suggested Reading
- •60: Glycemic Control in the ICU
- •Suggested Reading
- •61: Transfusion Practices and Complications
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Website
- •63: Onco-emergencies
- •63.1 Hypercalcemia
- •63.2 ECG Changes in Hypercalcemia
- •63.3 Superior Vena Cava Syndrome
- •63.4 Malignant Spinal Cord Compression
- •Suggested Reading
- •64: General Management of Trauma
- •Suggested Reading
- •65: Severe Head and Spinal Cord Injury
- •Suggested Reading
- •Websites
- •66: Torso Trauma
- •Suggested Reading
- •Websites
- •67: Burn Management
- •Suggested Reading
- •68: General Poisoning Management
- •Suggested Reading
- •69: Syndromic Approach to Poisoning
- •Suggested Reading
- •Websites
- •70: Drug Abuse
- •Suggested Reading
- •71: Snakebite
- •Suggested Reading
- •72: Heat Stroke and Hypothermia
- •72.1 Heat Stroke
- •72.2 Hypothermia
- •Suggested Reading
- •73: Jaundice in Pregnancy
- •Suggested Reading
- •Suggested Reading
- •75: Severe Preeclampsia
- •Suggested Reading
- •76: General Issues in Perioperative Care
- •Suggested Reading
- •Web Site
- •77.1 Cardiac Surgery
- •77.2 Thoracic Surgery
- •77.3 Neurosurgery
- •Suggested Reading
- •78: Initial Assessment and Resuscitation
- •Suggested Reading
- •79: Comprehensive ICU Care
- •Suggested Reading
- •Website
- •80: Quality Control
- •Suggested Reading
- •Websites
- •81: Ethical Principles in End-of-Life Care
- •Suggested Reading
- •82: ICU Organization and Training
- •Suggested Reading
- •Website
- •83: Transportation of Critically Ill Patients
- •83.1 Intrahospital Transport
- •83.2 Interhospital Transport
- •Suggested Reading
- •84: Scoring Systems
- •Suggested Reading
- •Websites
- •85: Mechanical Ventilation
- •Suggested Reading
- •86: Acute Severe Asthma
- •Suggested Reading
- •87: Status Epilepticus
- •Suggested Reading
- •88: Severe Sepsis and Septic Shock
- •Suggested Reading
- •89: Acute Intracranial Hypertension
- •Suggested Reading
- •90: Multiorgan Failure
- •90.1 Concurrent Management of Hepatic Dysfunction
- •Suggested Readings
- •91: Central Line Placement
- •Suggested Reading
- •92: Arterial Catheterization
- •Suggested Reading
- •93: Pulmonary Artery Catheterization
- •Suggested Reading
- •Website
- •Suggested Reading
- •95: Temporary Pacemaker Insertion
- •Suggested Reading
- •96: Percutaneous Tracheostomy
- •Suggested Reading
- •97: Thoracentesis
- •Suggested Reading
- •98: Chest Tube Placement
- •Suggested Reading
- •99: Pericardiocentesis
- •Suggested Reading
- •100: Lumbar Puncture
- •Suggested Reading
- •Website
- •101: Intra-aortic Balloon Pump
- •Suggested Reading
- •Appendices
- •Appendix A
- •Appendix B
- •Common ICU Formulae
- •Appendix C
- •Appendix D: Syllabus for ICU Training
- •Index
194 |
R. Rajani and F.N. Kapadia |
|
|
Step 13: Manage mechanical complications
•Cardiogenic shock, LV failure, and congestive heart failure should be managed with appropriate pharmacological therapy and rarely with mechanical devices (see Chaps. 20 and 21).
•Ventricular, septal, or papillary muscle rupture.
•RV infarction or ischemia may occur in up to 50% of patients with inferior wall MI.
•Suspect RV infarction in patients with inferior wall infarction, hypotension, and clear lung fields.
•In patients with inferior wall infarction, obtain an ECG with right-sided leads. Look for ST-segment elevation (>1 mm) in lead V4r.
•Nitrates, diuretics, and other vasodilators (ACE inhibitors) should be avoided because severe hypotension may result.
•Hypotension is initially treated with an IV fluid bolus.
Step 14: Consider other supportive therapy
•Sedatives and laxatives are useful in the initial stage.
•Hyperglycemia, either stress-induced or due to preexisting diabetes, should be controlled preferably at near-normal levels.
•Routine medication taken by the patient prior to the ACS should be reintroduced as appropriate.
Suggested Reading
1.Passaro D. Anti-platelet treatments in acute coronary syndrome: simplified network metaanalysis. Int J Cardiol. 2011;150(3):364–7.
2.O’Connor RE, Brady W, Brooks SC, et al. 2010 American Heart Association Guidelines for cardiopulmonary resuscitation and emergency cardiovascular care science: part 10. Circulation. 2010;122:S787–817.
Comment: an updated comprehensive guideline on acute coronary syndrome
3.Antman EM, Cohen M. The TIMI risk score for unstable angina/non-ST elevation MI: a method for prognostication and therapeutic decision making. JAMA. 2000;284(7):835–42.
The 7 TIMI risk score predictor variables were 65 years or older, at least three risk factors for coronary artery disease, prior coronary stenosis of 50% or more, ST-segment deviation on electrocardiogram at presentation, at least two anginal events in prior 24 h, use of aspirin in prior 7 days, and elevated serum cardiac marker.
Website
1.www.acc.org
A comprehensive website of American College of Cardiology
Hypertensive Urgencies |
24 |
and Emergencies |
Simran Singh and Chandrashekhar K. Ponde
A 55-year-old male patient was admitted to the emergency department with severe headache and giddiness. His blood pressure was 240/130 mmHg, pulse was 100/min regular, and sensorium was intact. He had also a left ventricular gallop, and room air oxygen saturation was 90%. Peripheral pulses were well felt. He was a known diabetic and hypertensive but was on irregular treatment.
Severe hypertensive crisis is occasionally seen in the ICU. Proper triaging, monitoring, and a balanced approach to lowering blood pressure are mandatory in these situations as overjealous reduction in pressure may lead to organ underperfusion, and undertreatment will lead to vital organ damage.
Step 1: Assess severity of hypertension and urgency of treatment
•Severe hypertension is defined when blood pressure exceeds 180/110 mmHg in the absence of symptoms beyond mild or moderate headache and without evidence of acute target organ damage.
•Hypertensive urgency is defined when blood pressure exceeds 180/110 mmHg in the presence of significant symptoms, such as severe headache or dyspnea, but has nil or only minimal acute target organ damage.
•Hypertensive emergency is defined when very high blood pressure (often >220/ 140 mmHg) is accompanied by evidence of life-threatening organ dysfunction such as cardiac, renal, retinal, or neurological.
S. Singh, M.D. (*)
Department of Medicine & Intensive Care, P.D. Hinduja National Hospital and Medical Research Centre, Mumbai, India
e-mail: simranjsingh@hotmail.com
C.K. Ponde, M.D., D.M.
Department of Cardiology, P.D. Hinduja National Hospital and Medical Research Centre, Mumbai, India
R. Chawla and S. Todi (eds.), ICU Protocols: A stepwise approach, |
195 |
DOI 10.1007/978-81-322-0535-7_24, © Springer India 2012 |
|
196 |
S. Singh and C.K. Ponde |
|
|
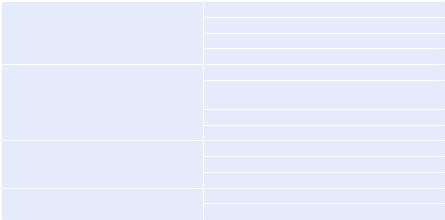
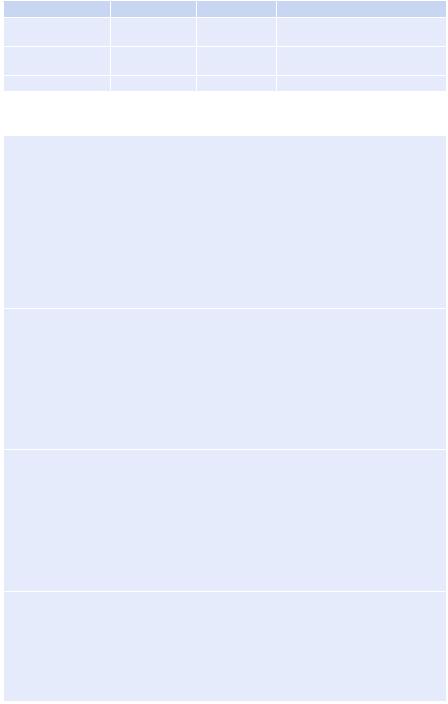
Table 24.1 Target organ damage |
|
Cardiovascular |
Myocardial infarction |
|
Unstable angina |
|
Aortic dissection |
|
Left ventricular failure |
Central nervous system |
Cerebral edema |
|
Altered mental status (hypertensive |
|
encephalopathy) |
|
Intracerebral or subarachnoid bleeding |
|
Cerebral infarct or transient ischemic attack |
Renal |
Microhematuria |
|
Proteinuria |
|
Acute renal failure |
Ophthalmologic |
Retinal hemorrhages or exudates |
|
Papilledema |
Step 2: Assess target organ involvement
•Perform focused history and physical examination
•History—duration and severity of hypertension and previous BP records
•Relevant symptoms:
–Headache and chest pain
–Dyspnea, edema, and acute fatigue
–Epistaxis
–Seizure
–Change in the level of consciousness
–Palpitation, diaphoresis, and tremors suggestive of pheochromocytoma
–Weight gain and thinning of skin suggestive of Cushing’s syndrome
•History of comorbid conditions—diabetes, smoking, hyperlipidemia, and chronic kidney disease:
–History of adherence to any prescribed antihypertensive medication is necessary
–Recent use of OCP (oral contraceptive pill), MAOI (monoamine oxidase inhibitors), nonsteroidal anti-inflammatory drug, cyclosporine, steroids, over- the-counter medicines, and herbal remedies
–Use of alcohol, cocaine, amphetamine, and phencyclidine
•Physical examination:
–Feel all peripheral pulses
–Measure the blood pressure using appropriate technique
–Measure the blood pressure in both arms and at least one leg if pedal pulses are diminished
–Carry out fundoscopy to look for papilledema and hypertension retinopathy
–Other systems examination—look for pedal edema, assess jugular venous pressure, and auscultate for abdominal bruits, crepitations and gallop, and basal crepitations
–Check the mental status
•Look for target organ damage (Table 24.1).
24 Hypertensive Urgencies and Emergencies |
197 |
|
|
Step 3: Send relevant investigations
•Initial evaluation
–Electrocardiogram—ST, T wave changes, evidence of left ventricular hypertrophy
–Hematocrit, white blood cell count, and peripheral blood smear—anemia, evidence of hemolysis
–Urea and creatinine
–Urinalysis with microscopic examination—hematuria and proteinuria
–Chest radiograph—cardiomegaly and pulmonary congestion
–Thyroid function tests
–Noncontrast computed tomography of the head (if neurologic findings are abnormal)
–Echocardiogram (left ventricular dysfunction, valve abnormalities, wall motion abnormalities)
–Lipid profile
•Tests to be done once the patient stabilizes
–Renal artery imaging (if renal stenosis is suspected)
–Other evaluations as guided by clinical presentation, namely, urinary VMA/ metanephrines/5-HIAA-phochromocytoma
–Plasma cortisol and dexamethasone suppression test—Cushing’s syndrome
Step 4: Understand treatment goals
•Hypertensive urgency
–Immediate goal—lower blood pressure within 24–72 h
–Treatment setting—clinical discretion is required
–Medications—oral medications with rapid onset of action; occasionally intravenously
•Hypertensive emergency
–Immediate goal—lower BP by 15–25% within 2 h, 25% within 12 h, 30% within 48 h
–Treatment setting—intensive care unit and intra-arterial monitoring
–Medications—intravenous
Step 5: Get familiar with drugs used in hypertensive urgencies and emergencies (Tables 24.2 and 24.3)
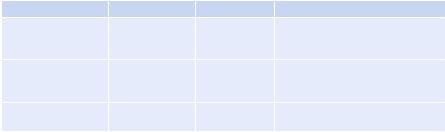
Table 24.2 Drugs for hypertensive urgencies |
|
||
Agent |
Dose |
Onset of action |
Comment |
Captopril |
12.5–25 mg PO |
15–60 min |
Can precipitate acute renal failure |
|
|
|
in patients with bilateral renal |
|
|
|
artery stenosis |
Nifedipine (extended |
10–20 mg PO |
20 min |
Avoid short-acting or sublingual |
release) |
|
|
nifedipine due to risk of sudden |
|
|
|
hypotension, stroke, cardiac event |
Labetalol |
200–400 mg PO |
20–120 min |
Heart failure, bradycardia, |
|
|
|
bronchospasm |
|
|
|
(continued) |
198 |
|
|
S. Singh and C.K. Ponde |
|
|
|
|
Table 24.2 |
(continued) |
|
|
Agent |
Dose |
Onset of action |
Comment |
Clonidine |
0.1–0.2 mg PO |
30–60 min |
Rebound hypertension due to |
|
|
|
abrupt withdrawal |
Prazosin |
1–2 mg PO |
2–4 h |
First-dose hypotension, syncope, |
|
|
|
tachycardia |
Amlodipine |
5–10 mg |
30–50 min |
Headache, tachycardia, flushing |
Table 24.3 Drugs for hypertensive emergencies
Sodium nitroprusside
Dose: 0.25–10 mcg/Kg/min IV infusion
Onset/duration of action after discontinuation: seconds/2–3 min Comments
Arterial and venodilator with rapid onset and offset of action Preferred agents for most hypertensive emergencies
Titrate to goal BP
Infusion bag and delivery set must be light resistant or covered Nausea, vomiting, muscle twitching on prolonged use (>24–48 h)
Thiocyanate/cyanide intoxication, metabolic acidosis in patients with renal impairment Thiocyanate level >10 mg/dL should be avoided
Nitroglycerine
Dose: 5–100 mcg/min IV infusion
Onset/duration of action after discontinuation: 2–5 min/5–15 min
Comments
Mostly venodilator with modest arterial dilation
Headache, tachycardia, flushing, vomiting
Develops tolerance with prolonged use
Methemoglobinemia
Useful in emergencies with cardiac failure or ischemia
Labetalol
Dose: 10–80 mg IV bolus every 10 min to a maximum dose of 300 mg
Infusion: 0.5–2 mg/min
Onset/duration of action after discontinuation: 5–10 min/3–6 h
Comments
Combined a- and b-blockade
Bradycardia, bronchospasm
Avoid in congestive heart failure (CHF), bronchial asthma
Commonly used in pregnancy-induced hypertension
Enalapril
Dose: 1.25 mg every 6 h
Onset/duration of action after discontinuation: 15–30 min/6–12 h
Comments
Mainly afterload reduction
Contraindicated in pregnancy, renal artery stenosis
Useful in patients with CHF
(continued)

24 Hypertensive Urgencies and Emergencies |
199 |
|
|
Table 24.3 (continued)
Esmolol
Dose: 500 mcg/Kg IV bolus can be repeated after 5 min
Infusion: 50–200 mcg/Kg/min
Onset/duration of action after discontinuation: 1–5 min/15–30 min
Comments
Avoid in patients with heart block, CHF, asthma
Short-acting cardioselective b-blocker
Bradycardia, CHF, heart block, may precipitate bronchospasm
Hydralazine
Dose: 10–20 mg IV bolus may be repeated every 30 min till goal BP is reached or unacceptable tachycardia develops
Onset/duration of action after discontinuation: 10–30 min/2–4 h Comments
Direct arteriolar vasodilator Reflex tachycardia, flushing
Avoid in patients with increased ICP, ischemic heart disease, and aortic dissection (without b-blockade)
Phentolamine
Dose: 5–15 mg IV bolus, repeat every 5–15 min
Infusion: 0.2–5 mg/min
Onset/duration of action after discontinuation: 1–2 min/10–30 min
Comments
Pure a-blockade
Reflex tachycardia, orthostatic hypotension
Used in syndromes with excess catecholamine (pheochromocytoma)
Nicardipine
Dose: 5 mg/h IV infusion; titrate up by 2.5 mg/h every 20 min up to maximum dose of 15 mg/h
Onset/duration of action after discontinuation: 15–30 min/1–4 h Comments
Dihydropyridine calcium channel blocker Reflex tachycardia
Avoid in acute heart failure
Useful in subarachnoid hemorrhage
Fenoldopam
0.1 mcg/Kg/min IV infusion, titrate up every 15 min to a maximum of 0.8 mcg/Kg/min Onset/duration of action after discontinuation: 3–5 min/30 min
Comments
Selective peripheral dopamine-1 receptor agonist Arterial vasodilator
Improves renal perfusion, useful in patients with hypertensive emergencies with renal failure
Contraindicated in glaucoma
