
- •ICU Protocols
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1: Airway Management
- •Suggested Reading
- •2: Acute Respiratory Failure
- •Suggested Reading
- •Suggested Reading
- •Website
- •4: Basic Mechanical Ventilation
- •Suggested Reading
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Websites
- •7: Weaning
- •Suggested Reading
- •8: Massive Hemoptysis
- •Suggested Reading
- •9: Pulmonary Thromboembolism
- •Suggested Reading
- •Suggested Reading
- •Websites
- •11: Ventilator-Associated Pneumonia
- •Suggested Readings
- •12: Pleural Diseases
- •Suggested Reading
- •Websites
- •13: Sleep-Disordered Breathing
- •Suggested Reading
- •Websites
- •14: Oxygen Therapy
- •Suggested Reading
- •15: Pulse Oximetry and Capnography
- •Conclusion
- •Suggested Reading
- •Websites
- •16: Hemodynamic Monitoring
- •Suggested Reading
- •Websites
- •17: Echocardiography
- •Suggested Readings
- •Websites
- •Suggested Reading
- •Websites
- •19: Cardiorespiratory Arrest
- •Suggested Reading
- •Websites
- •20: Cardiogenic Shock
- •Suggested Reading
- •21: Acute Heart Failure
- •Suggested Reading
- •22: Cardiac Arrhythmias
- •Suggested Reading
- •Website
- •23: Acute Coronary Syndromes
- •Suggested Reading
- •Website
- •Suggested Reading
- •25: Aortic Dissection
- •Suggested Reading
- •26: Cerebrovascular Accident
- •Suggested Reading
- •Websites
- •27: Subarachnoid Hemorrhage
- •Suggested Reading
- •Websites
- •28: Status Epilepticus
- •Suggested Reading
- •29: Acute Flaccid Paralysis
- •Suggested Readings
- •30: Coma
- •Suggested Reading
- •Suggested Reading
- •Websites
- •32: Acute Febrile Encephalopathy
- •Suggested Reading
- •33: Sedation and Analgesia
- •Suggested Reading
- •Websites
- •34: Brain Death
- •Suggested Reading
- •Websites
- •35: Upper Gastrointestinal Bleeding
- •Suggested Reading
- •36: Lower Gastrointestinal Bleeding
- •Suggested Reading
- •37: Acute Diarrhea
- •Suggested Reading
- •38: Acute Abdominal Distension
- •Suggested Reading
- •39: Intra-abdominal Hypertension
- •Suggested Reading
- •Website
- •40: Acute Pancreatitis
- •Suggested Reading
- •Website
- •41: Acute Liver Failure
- •Suggested Reading
- •Suggested Reading
- •Websites
- •43: Nutrition Support
- •Suggested Reading
- •44: Acute Renal Failure
- •Suggested Reading
- •Websites
- •45: Renal Replacement Therapy
- •Suggested Reading
- •Website
- •46: Managing a Patient on Dialysis
- •Suggested Reading
- •Websites
- •47: Drug Dosing
- •Suggested Reading
- •Websites
- •48: General Measures of Infection Control
- •Suggested Reading
- •Websites
- •49: Antibiotic Stewardship
- •Suggested Reading
- •Website
- •50: Septic Shock
- •Suggested Reading
- •51: Severe Tropical Infections
- •Suggested Reading
- •Websites
- •52: New-Onset Fever
- •Suggested Reading
- •Websites
- •53: Fungal Infections
- •Suggested Reading
- •Suggested Reading
- •Website
- •55: Hyponatremia
- •Suggested Reading
- •56: Hypernatremia
- •Suggested Reading
- •57: Hypokalemia and Hyperkalemia
- •57.1 Hyperkalemia
- •Suggested Reading
- •Website
- •58: Arterial Blood Gases
- •Suggested Reading
- •Websites
- •59: Diabetic Emergencies
- •59.1 Hyperglycemic Emergencies
- •59.2 Hypoglycemia
- •Suggested Reading
- •60: Glycemic Control in the ICU
- •Suggested Reading
- •61: Transfusion Practices and Complications
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Website
- •63: Onco-emergencies
- •63.1 Hypercalcemia
- •63.2 ECG Changes in Hypercalcemia
- •63.3 Superior Vena Cava Syndrome
- •63.4 Malignant Spinal Cord Compression
- •Suggested Reading
- •64: General Management of Trauma
- •Suggested Reading
- •65: Severe Head and Spinal Cord Injury
- •Suggested Reading
- •Websites
- •66: Torso Trauma
- •Suggested Reading
- •Websites
- •67: Burn Management
- •Suggested Reading
- •68: General Poisoning Management
- •Suggested Reading
- •69: Syndromic Approach to Poisoning
- •Suggested Reading
- •Websites
- •70: Drug Abuse
- •Suggested Reading
- •71: Snakebite
- •Suggested Reading
- •72: Heat Stroke and Hypothermia
- •72.1 Heat Stroke
- •72.2 Hypothermia
- •Suggested Reading
- •73: Jaundice in Pregnancy
- •Suggested Reading
- •Suggested Reading
- •75: Severe Preeclampsia
- •Suggested Reading
- •76: General Issues in Perioperative Care
- •Suggested Reading
- •Web Site
- •77.1 Cardiac Surgery
- •77.2 Thoracic Surgery
- •77.3 Neurosurgery
- •Suggested Reading
- •78: Initial Assessment and Resuscitation
- •Suggested Reading
- •79: Comprehensive ICU Care
- •Suggested Reading
- •Website
- •80: Quality Control
- •Suggested Reading
- •Websites
- •81: Ethical Principles in End-of-Life Care
- •Suggested Reading
- •82: ICU Organization and Training
- •Suggested Reading
- •Website
- •83: Transportation of Critically Ill Patients
- •83.1 Intrahospital Transport
- •83.2 Interhospital Transport
- •Suggested Reading
- •84: Scoring Systems
- •Suggested Reading
- •Websites
- •85: Mechanical Ventilation
- •Suggested Reading
- •86: Acute Severe Asthma
- •Suggested Reading
- •87: Status Epilepticus
- •Suggested Reading
- •88: Severe Sepsis and Septic Shock
- •Suggested Reading
- •89: Acute Intracranial Hypertension
- •Suggested Reading
- •90: Multiorgan Failure
- •90.1 Concurrent Management of Hepatic Dysfunction
- •Suggested Readings
- •91: Central Line Placement
- •Suggested Reading
- •92: Arterial Catheterization
- •Suggested Reading
- •93: Pulmonary Artery Catheterization
- •Suggested Reading
- •Website
- •Suggested Reading
- •95: Temporary Pacemaker Insertion
- •Suggested Reading
- •96: Percutaneous Tracheostomy
- •Suggested Reading
- •97: Thoracentesis
- •Suggested Reading
- •98: Chest Tube Placement
- •Suggested Reading
- •99: Pericardiocentesis
- •Suggested Reading
- •100: Lumbar Puncture
- •Suggested Reading
- •Website
- •101: Intra-aortic Balloon Pump
- •Suggested Reading
- •Appendices
- •Appendix A
- •Appendix B
- •Common ICU Formulae
- •Appendix C
- •Appendix D: Syllabus for ICU Training
- •Index
Drug Dosing |
47 |
|
|
Pratik Das and Arghya Majumdar |
|
A 55-year-old diabetic and hypertensive male was admitted with acute kidney injury secondary to urosepsis. He was anuric and hemodynamically unstable and had been put on slow extended dialysis. He was a known epileptic on phenobarbitone and levetiracetam. He underwent coronary artery bypass grafting 2 years ago and had congestive cardiac failure. He was on isosorbide mononitrate, digoxin, aspirin, atenolol, hydralazine, pantoprazole, atorvastatin, fenoÞbrate, and insulin. He had been commenced on meropenem and needed noradrenaline infusion.
Polypharmacy is very common in the ICU due to multiple comorbidities of the patient. Adverse side effects and drug interaction, especially in the patient with renal impairment and renal replacement therapy (RRT), should be carefully looked for, and drug dose may need to be adjusted; drugs may need to be withdrawn or substituted.
Step 1: Assess need for dose adjustment in renal failure
¥The pharmacokinetics and pharmacodynamics of most drugs are altered in patients with renal failure, especially those with a predominant renal clearance (e.g., meropenem with 70% renal clearance).
¥The volume of distribution of several drugs and their metabolites is altered in renal failure (e.g., digoxin).
¥The risk of side effects is much higher for some drugs, in patients with renal failure (e.g., phenobarbitone).
P. Das, M.D., D.M. (*)
Consultant Nephrologist, Rabindranath Tagore Hospital, Kolkata, West Bengal, India
A. Majumdar, M.D., M.R.C.P.
Department of Nephrology, AMRI Hospitals, Kolkata, West Bengal, India
R. Chawla and S. Todi (eds.), ICU Protocols: A stepwise approach, |
375 |
DOI 10.1007/978-81-322-0535-7_47, © Springer India 2012 |
|
376 |
P. Das and A. Majumdar |
|
|
¥For drugs with only minor or no dose-related side effects, very precise modiÞcation of the dosage regimen is not essential (e.g., pantoprazole). However, for more toxic drugs, with a small safety margin (e.g., digoxin), dose regimens based on glomerular Þltration rate (GFR) is mandatory.
Step 2: Calculate GFR
¥CockroftÐGault formula:
ÐIt is commonly used to calculate the creatinine clearance (Clcr) and has traditionally been used to approximate the GFR.
ÐIt is fairly accurate for chronic kidney disease with a stable serum creatinine, but in acute kidney injury (AKI) with unstable serum creatinine, this formula may not be accurate and may overestimate the GFR.
Clcr = |
(140 - age in years) ´ lean body weight |
´ 0.85 for female |
) |
|
|||
( |
|||
|
72 ´ serumcreatinine in mg / dL |
|
|
¥In ICU, actual body weight is difÞcult to measure in most situations, and ideal body weight is taken instead for calculation of GFR.
¥Ideal body weight (IBW) may be calculated in the ICU by the following formulas:
ÐMales (IBW in kg): 50 + 2.3 (height in inches −60)
ÐFemales (IBW in kg): 45.5 + 2.3 (height in inches −60)
¥ModiÞcation of diet in renal disease (MDRD) formula for estimation of GFR and eGFR and radioisotope methods are other ways of calculating GFR but not commonly used in the ICU.
¥Anuric AKI patients have a GFR less than 10 mL/min, as a rule, irrespective of serum creatinine value and need no calculation.
¥For the patient on dialysis, GFR is taken as less than 15 mL/min.
Step 3: Calculate loading dose of a drug
¥The patient with renal failure of any severity should receive the same loading dose as the patient with normal renal function to achieve a rapid therapeutic level.
Step 4: Calculate maintenance dose
¥Before adjusting the maintenance dose, the route of excretion should be ascertained. The maintenance dose should be adjusted only for drugs with the following properties:
ÐGreater than 50% renal excretion
ÐLow rate of protein binding
ÐSmall volume of distribution
¥The maintenance dosage in patients with renal insufÞciency can be adjusted in three ways:
ÐDosing interval prolongation, dosage reduction, or both (Table 47.1)
47 Drug Dosing |
|
377 |
|
|
|
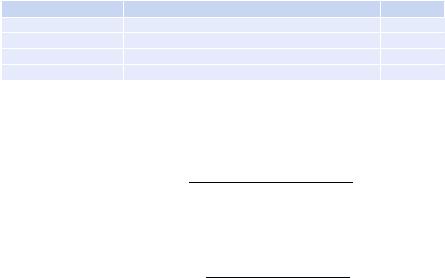
Table 47.1 Meropenem (>70%) renal excretion |
|
|
Creatinine clearance |
Dose (based on unit dose of 500 mg, 1 g, and 2 g) |
Frequency |
>50 |
One unit dose |
Every 8 h |
26Ð50 |
One unit dose |
Every 12 h |
10Ð25 |
One-half unit dose |
Every 12 h |
<10 |
One-half unit dose |
Every 24 h |
¥Increasing the dosage interval to correspond to the degree of renal dysfunction can be calculated from the following formula:
= Normal Clcr ´ normal interval
Dosing interval
Patient Clcr
¥Dosage reduction without changing the dosing interval can be calculated from the following formula:
= Patient Clcr ´ normal dose
Maintenance dose
Normal Clcr
ÐDosage interval extension allows for adequate peak concentration but may risk subtherapeutic trough levels.
ÐDosage reduction may provide for more constant drug levels but increases the risk of toxicity from higher plasma trough concentrations.
Step 5: Utilization of the drug dosing chart (See Appendix A.2)
¥Every critical care unit should use a detailed drug dosing chart in renal failure and should consult this prior to prescription.
¥Package insert of a medicine is a Òready reckonerÓ for drug dose modiÞcation.
¥The dosage modiÞcations are an approximation and guided by features of drug toxicity and, if feasible, drug levels.
¥Remember to supplement some medications postdialysis like carbapenems.
¥These are approximations and drug dosing need to be individualized in critically ill patient depending on various factors as described in previous steps.
Step 6: Dosing on continuous renal replacement therapy (CRRT)
¥CRRT is most often used for the management of critically ill patients who are too hemodynamically unstable to tolerate intermittent hemodialysis.
¥There is very limited information about how CRRT affects the clearance of individual pharmacologic agents.
¥During CRRT, most drugs can be approximately dosed for a GFR of 10Ð30 mL/ min.
¥However, for some drugs, the diffusion process signiÞcantly increases drug clearance during CRRT due to high-ßux dialysis.

378 |
P. Das and A. Majumdar |
|
|
Suggested Reading
1.Aronoff GR, Bennet WM, Berns JS, et al. Drug prescribing in renal failure. 5th ed. Philadelphia/ New Delhi: American College of Physicians/Jaypee Brothers Medical Publishers (P) Ltd; 2007.
Websites
1.http://kdpnet.louisville.edu/renalbook/ An online pocketbook for drug calculation
2.www.globalrph.com
A comprehensive user-friendly site for drug dose calculation

Part VI
Infectious Diseases
Subhash Todi
