
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1. Introduction
- •2. Evaluation of the Craniomaxillofacial Deformity Patient
- •3. Craniofacial Deformities: Review of Etiologies, Distribution, and Their Classification
- •4. Etiology of Skeletal Malocclusion
- •5. Etiology, Distribution, and Classification of Craniomaxillofacial Deformities: Traumatic Defects
- •6. Etiology, Distribution, and Classification of Craniomaxillofacial Deformities: Review of Nasal Deformities
- •7. Review of Benign Tumors of the Maxillofacial Region and Considerations for Bone Invasion
- •8. Oral Malignancies: Etiology, Distribution, and Basic Treatment Considerations
- •9. Craniomaxillofacial Bone Infections: Etiologies, Distributions, and Associated Defects
- •11. Craniomaxillofacial Bone Healing, Biomechanics, and Rigid Internal Fixation
- •12. Metal for Craniomaxillofacial Internal Fixation Implants and Its Physiological Implications
- •13. Bioresorbable Materials for Bone Fixation: Review of Biological Concepts and Mechanical Aspects
- •14. Advanced Bone Healing Concepts in Craniomaxillofacial Reconstructive and Corrective Bone Surgery
- •15. The ITI Dental Implant System
- •16. Localized Ridge Augmentation Using Guided Bone Regeneration in Deficient Implant Sites
- •17. The ITI Dental Implant System in Maxillofacial Applications
- •18. Maxillary Sinus Grafting and Osseointegration Surgery
- •19. Computerized Tomography and Its Use for Craniomaxillofacial Dental Implantology
- •20B. Atlas of Cases
- •21A. Prosthodontic Considerations in Dental Implant Restoration
- •21B. Overdenture Case Reports
- •22. AO/ASIF Mandibular Hardware
- •23. Aesthetic Considerations in Reconstructive and Corrective Craniomaxillofacial Bone Surgery
- •24. Considerations for Reconstruction of the Head and Neck Oncologic Patient
- •25. Autogenous Bone Grafts in Maxillofacial Reconstruction
- •26. Current Practice and Future Trends in Craniomaxillofacial Reconstructive and Corrective Microvascular Bone Surgery
- •27. Considerations in the Fixation of Bone Grafts for the Reconstruction of Mandibular Continuity Defects
- •28. Indications and Technical Considerations of Different Fibula Grafts
- •29. Soft Tissue Flaps for Coverage of Craniomaxillofacial Osseous Continuity Defects with or Without Bone Graft and Rigid Fixation
- •30. Mandibular Condyle Reconstruction with Free Costochondral Grafting
- •31. Microsurgical Reconstruction of Large Defects of the Maxilla, Midface, and Cranial Base
- •32. Condylar Prosthesis for the Replacement of the Mandibular Condyle
- •33. Problems Related to Mandibular Condylar Prosthesis
- •34. Reconstruction of Defects of the Mandibular Angle
- •35. Mandibular Body Reconstruction
- •36. Marginal Mandibulectomy
- •37. Reconstruction of Extensive Anterior Defects of the Mandible
- •38. Radiation Therapy and Considerations for Internal Fixation Devices
- •39. Management of Posttraumatic Osteomyelitis of the Mandible
- •40. Bilateral Maxillary Defects: THORP Plate Reconstruction with Removable Prosthesis
- •41. AO/ASIF Craniofacial Fixation System Hardware
- •43. Orbital Reconstruction
- •44. Nasal Reconstruction Using Bone Grafts and Rigid Internal Fixation
- •46. Orthognathic Examination
- •47. Considerations in Planning for Bimaxillary Surgery and the Implications of Rigid Internal Fixation
- •48. Reconstruction of Cleft Lip and Palate Osseous Defects and Deformities
- •49. Maxillary Osteotomies and Considerations for Rigid Internal Fixation
- •50. Mandibular Osteotomies and Considerations for Rigid Internal Fixation
- •51. Genioplasty Techniques and Considerations for Rigid Internal Fixation
- •52. Long-Term Stability of Maxillary and Mandibular Osteotomies with Rigid Internal Fixation
- •53. Le Fort II and Le Fort III Osteotomies for Midface Reconstruction and Considerations for Internal Fixation
- •54. Craniofacial Deformities: Introduction and Principles of Management
- •55. The Effects of Plate and Screw Fixation on the Growing Craniofacial Skeleton
- •56. Calvarial Bone Graft Harvesting Techniques: Considerations for Their Use with Rigid Fixation Techniques in the Craniomaxillofacial Region
- •57. Crouzon Syndrome: Basic Dysmorphology and Staging of Reconstruction
- •58. Hemifacial Microsomia
- •59. Orbital Hypertelorism: Surgical Management
- •60. Surgical Correction of the Apert Craniofacial Deformities
- •Index
59
Orbital Hypertelorism: Surgical Management
Antonio Fuente del Campo
Orbital hypertelorism is a malformation of the craniofacial skeleton characterized by an increased interorbital distance. The term hypertelorism comes from the Greek language and was first used by Grieg in 1924, who used the term ocular hypertelorism.1
Adaptations and variants of the term have been used since then, and it is sometimes misused. Thus we hear about primary, secondary, apparent, and posttraumatic hypertelorism, and so on. A group of hypertelorizing deformities has even been created, which includes craniostenosis and facial, cranial, or mixed fissures (e.g., bifid skull, frontal dysrhaphia, orbitofacial clefts, meningoencephalocele). Hypertelorism is common to all these conditions. In the cases of coexisting hypertelorism and fissure, the interorbital distance is usually related to the dimension of the fissure.
Others think that the most appropriate term for this malformation is teleorbitism (i.e., increased orbital distance) because it is more specific and concrete, and also because it avoids confusion with similar terms that involve other alterations.
Regardless of the term being used, it should be reserved for congenital malformations characterized by the widening of the nasal root, opening of the ascending processes of the maxillae and outer displacement of the orbits, the eyes, and the lateral canthi (Figure 59.1).
The term posttraumatic hypertelorism is not acceptable, since under these conditions the orbital displacement is not total and is followed only partially by the eyes. The term apparent hypertelorism refers to alterations of soft or bony parts that suggest an increased interorbital distance that really is not present. These are the cases of posttraumatic telecanthus, lateral displacement of the lacrimal point, hidden caruncle, flattening of the nose base, epicanthus, increased interciliary distance, Waardenburg’s syndrome, and so on.
In cases of primary telecanthus, there is an apparent increased interorbital distance, without a real displacement of the eyes or the orbits in relation to the facial midline. In hypertelorism, both the eye globe and the inner canthus of the palpebral fissure have shifted away from the midline. Of course, these alterations are not mutually exclusive, and this is the case of telecanthus secondary to hypertelorism.
Diagnosis
Different methods are used to determine the presence and severity of hypertelorism. They include the measurement of the interpupillary distance, which is difficult to determine and useless in cases with ocular deviations, and the medial intercanthal distance, which is inapplicable in cases with soft tissue alterations in this area.
The intercrestal distance is determined using anteroposterior cephalometry by measuring the space between both posterior lacrimal crests. According to Gunther2 and others3–5 the following figures are considered as normal variants in adults: 20 to 26 mm (average 25 mm) in females and 21 to 28 mm (average 26 mm) in males. Greater figures mean hypertelorism, which may be graded as follows: grade I: 28 to 34 mm, grade II: 34 to 40 mm, and grade III: 40 mm. However, expansive alterations of the midline, such as a frontonasal meningoencephalocele, may increase the intercrestal distance without the presence of true hypertelorism.
Other methods include the circumferential interorbital index and the canthal index. Nevertheless, we think that the lateral intercanthal distance is the simplest and most reliable method for diagnostic purposes. In the case of detachment of one of the lateral canthi, the lateral interorbital distance could be measured on the anteroposterior (AP) cephalometry.
Therefore, the clinical assessment of these patients should not be based on a single measurement but rather on several measurements so as to establish the accurate and integral diagnosis.5,6
Malformation Analysis
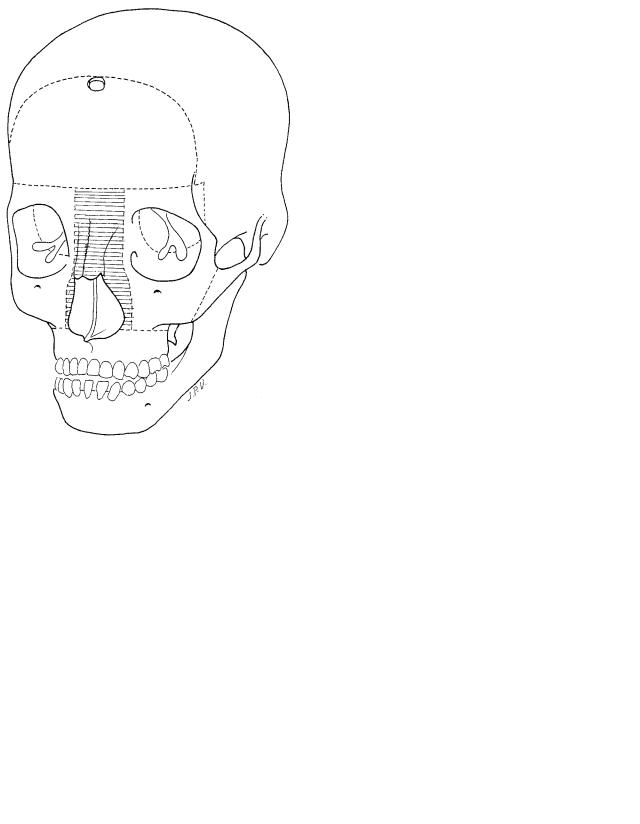
In the radiographic cephalometry of a patient with grade III hypertelorism (Figure 59.2), the ethmoid looks wider and shorter, and it is usually found at a level lower than normal. The cribiform plate may be normal, but it is usually wider and depressed. The crista galli may be very large, duplicated, or absent. The greater wings of the sphenoid bone are small. There is a more marked orbital divergence in the frontal arch than in the maxillary arch, but this separation really occurs in the frames and not in the orbital apex. The upper inner angle
738
59. Orbital Hypertelorism: Surgical Management
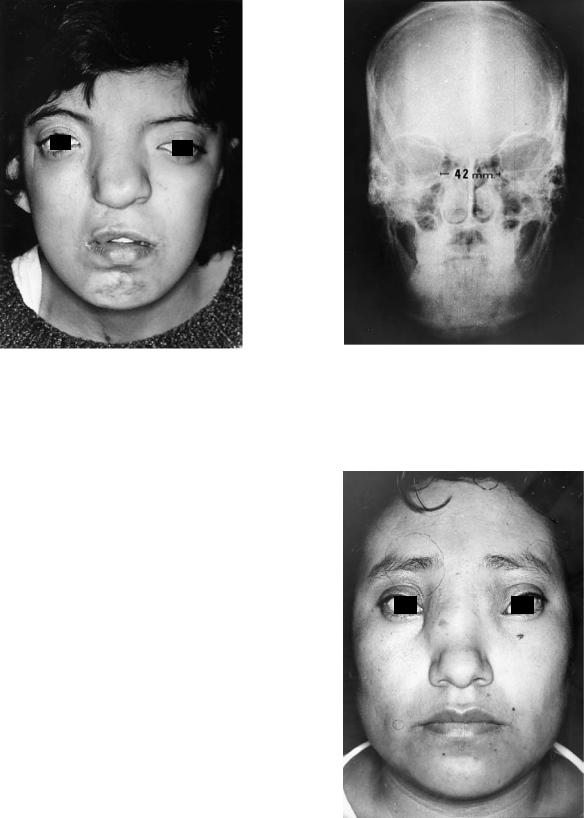
FIGURE 59.1 A 28-year-old female patient, with grade III hypertelorism and Tessier 2–12 right facial cleft.
of the orbit is rounded, and its medial wall becomes oblique downward and outward.
Often there are decreased vertical dimensions of the centrofacial skeleton, including the ethmoid, the vomer, and the medial segment of the maxillae, resulting in an oval palate and an anterior open bite. There may also be micro-orbitism, with microphthalmia or anophthalmia, associated with orbitopalpebral clefts, bone defects of the fronto-orbital region, hairline alterations, such as the “widow’s peak” and various irregularities associated with dystopia or eyebrow distortion.
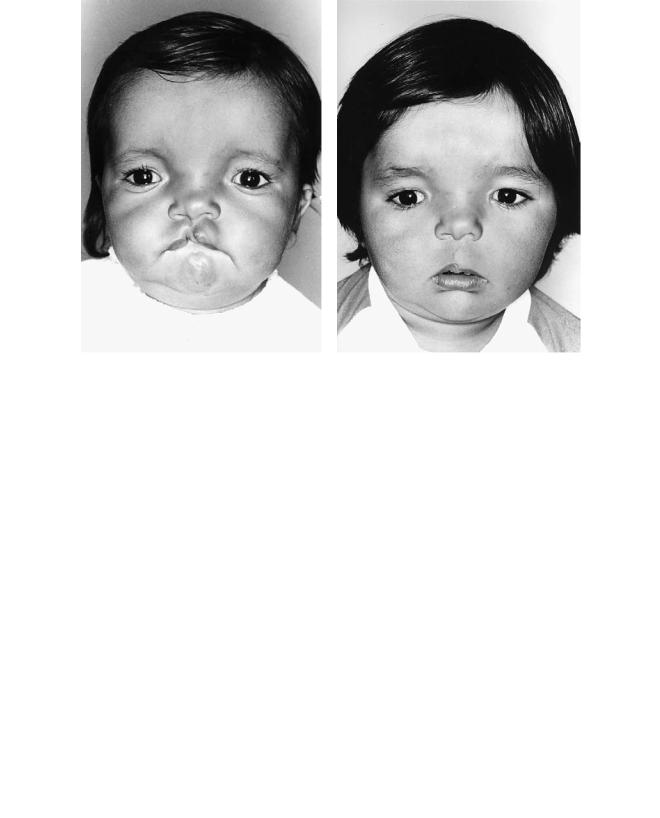
Orbital hypertelorism associated with craniofacial clefts (Tessier 0, 1, 2, 3, 11, 12, 13, 14), presents with a wide nose, vertically divided by one or several central and/or paramedian clefts. The nose may be short or practically absent and associated with a frontonasal or frontonasoethmoidal meningoencephalocele (Figure 59.3).
In unilateral paranasal clefts, usually only the orbit on the involved side shows an increased distance from the facial midline, including the eye globe and the inner canthus, while the contralateral orbit has a virtually normal position and shape.
Etiopathology
739
FIGURE 59.2 Anteroposterior radiographic cephalometry, from a patient with hypertelorism grade III (42 mm of intercrestal distance).
According to Tessier,5 the interorbital distance develops similar to the ethmoid, the frontal bone, and the maxillae, the result depending on the effects between the active divergent
FIGURE 59.3 A 34-year-old female patient, whose hypertelorism is associated with a frontonasoethmoidal meningoencephalocele (grade III).
740
forces, such as the excessive intracranial pressure (endocranial hypertension) and the convergence forces represented by the cohesive forces of the bones and the temporal muscles. The presence of vertical compression and/or any deformity of the anterior cranial fossa may increase its dimensions and result in ethmoidal prolapse, which prevents the natural displacement of the orbits toward the midline, thus causing hypertelorism.6,7
The etiologic role previously attributed to the ethmoidal pneumatization that laterally deflects the orbits has lost support. On the contrary, it is now believed that when the orbits remain lateralized without reaching their normal position near to the midline, the resulting space between them is occupied by the ethmoid. When this does not happen, probably due to cell degeneration, craniofacial clefts and encephalomeningoceles occur, which are frequently associated with orbital hypertelorism, or teleorbitism.8,9
Treatment
In 1967 Tessier, who is recognized worldwide as the pioneer of this surgery, has described these procedures as consisting of the interorbital surgical reduction which is determined by evaluating the clinical appearance of the patient, his or her anthropometry, and the AP x-ray cephalometry. The orbits are shifted toward the midline, eliminating part of the ethmoid until a normal interorbital distance is obtained. Later on, Converse proposed a modification aimed at assuring the preservation of olfaction.10
The treatment of these patients should focus on the correction of the bony malformations together with the alterations of the soft parts. Many of them, in addition to the increased distance between the orbits, also have nasal hypoplasia and maxillary alterations, such as an anterior open bite.
The described basic surgical procedures can be extracranial (subcranial) or intracranial. The former are indicated only in some cases of grade I hypertelorism. In grade II and III cases, the procedures of choice are intracranial.
Surgical Procedures
The approach in both procedures (subcranial and intracranial), is a coronal incision extending from the preauricular region of one side to the other side, far away from the hairline and the craniotomy area. Laterally, the incision should be created downward in front of the origin of the helix, for a better exposure upon flap rotation. Dissection of the frontal plane is started on a supraperiosteal plane and 3 cm above the orbital roof, the periosteum is incised horizontally. It is dissected subperiosteally upward, with the shape of a posterior pedicle flap, until the frontal bone is exposed. The temporal muscle is de-
A. Fuente del Campo
tached from its medial portion, sectioning it at the level of the temporal crest. Upon doing so, it is important to spare a strip of its fascia so that later on it can be easily sutured at its origin.
The periosteum is vertically incised on the nasal dorsum and laterally at the level of the malar process of the frontal bone, to allow the distension of the flap and facilitate the approach. The subperiosteal dissection is continued to the face along the periorbital region, the malar bone, the inside of both orbits, the nasal pyramid, and the maxilla. The supraorbital neurovascular bundles are released from their bony canal using a fine chisel. A small, curved elevator allows the surgeon to dissect around the lacrimal ducts and the medial canthal ligaments without detaching them.11–13
Intracranial Procedures
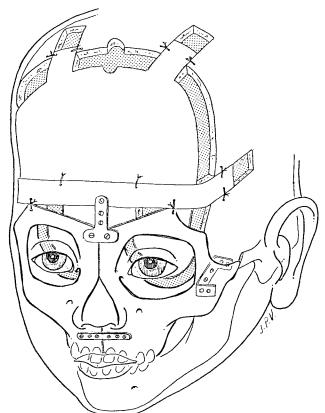
There are two basic intracranial procedures: orbital medialization and hemifacial rotation. The intracranial approach is done through a rectangular bifrontal craniotomy, which allows adequate access to the anterior cranial floor. The lower limit of the craniotomy is about 1 or 2 cm above the rim of the roof of both orbits. Once the orbital roof and the cribriform plate are exposed, the osteotomies are started through this approach, alternating the high-speed saw and a 6-mm chisel along the orbital roof to descend toward the inner surface of the lateral wall. These osteotomies should be done 1 cm behind the central axis of the eye globe, so that the medialization of the orbit totally displaces the eye (Figure 59.4).
The temporal intracranial fossa is dissected on its medial portion and gauze pads are placed between the bone and the meninges to protect the brain and its vessels during the osteotomy of the orbital roof (greater wing of the sphenoid bone) and the upper part of the lateral wall. The temporal muscle is laterally displaced to complete the lateral wall osteotomy from a lateral approach with a reciprocating saw until the orbital floor is reached.
During this maneuver, the content of the orbit is protected with a malleable retractor that allows the eye to be raised while the orbital floor osteotomy is performed using the same instrument. The orbital roof osteotomy is continued toward the midline, going down through the medial wall, behind the lacrimal apparatus, until the osteotomy performed on the floor is reached.
Laterally, the osteotomy is completed at the level of the zygomatic arch. The latter is sectioned diagonally and downward from above and from the back to the front to prevent the orbital medialization from resulting in a bone step and the subsequent depression of the soft parts at this level. This variant of the osteotomy allows to displace the malar bones maintaining the continuity with the orbits, thus achieving a more natural and cosmetic effect.
The osteotomy of the orbital rims is completed using a oscillating saw to section the lower limit in a horizontal direction from the malar bone to the piriform aperture. It is per-
59. Orbital Hypertelorism: Surgical Management |
741 |
a |
b |
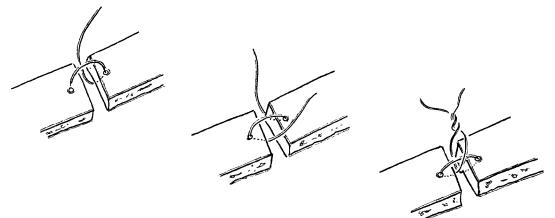
FIGURE 59.4 Orbital medialization through an intracranial approach. (a) Osteotomies and interorbital bone resection. (b) New position and osteosynthesis of the orbits.
formed underneath the emergence of the infraorbital nerve using the upper vestibular approach for this purpose. Then the interorbital bone resection estimated previously (Figure 59.4a) is performed. It includes part of the ascending processes of the maxillae, the ethmoid and the frontal bone.14,15
In cases with a normal nasal pyramid, we detach the latter from the frontal bone (nasal salvage) by means of a vertical osteotomy at the level of the frontonasal suture (Figure 59.5). The septum is also sectioned at this level and the nasal pyramid is pulled frontward and rotated downward, making sure that its mucosa is left intact.16
Then the interorbital bone resection is performed, making sure that the cribriform plate of the ethmoid is spared, thus olfaction is preserved.
Once the osteotomies have been performed, the orbits are slowly and progressively mobilized until the soft parts are released and the rims come to be in contact medially, at the desired distance; the frontal bone is repositioned to its original position and is immobilized with an anchored wire osteosynthesis (Figure 59.6). The orbital frames are anchored to the frontal bone at their new position and the nasal pyramid is
FIGURE 59.5 Nasal salvage. Vertical osteotomy to detach the nasal pyramid from the frontal bone and to perform the interorbital bone resection without affecting the original nasal structure.
742 |
A. Fuente del Campo |
FIGURE 59.6 Anchored osteosynthesis, used for the cranial bones.
repositioned between both orbits at the appropriate height (Figure 59.4b).
The excellent stability of the repositioned fragments and the absence of antagonistic forces at this level make it unnecessary to use plates and screws. The lateral bone defects resulting from displacing the orbits are filled with bone grafts taken from the resected interorbital segment or from the parietal bone.
In cases with a deformed or hypoplastic nasal pyramid, such as central fissures and meningoencephaloceles, it is necessary to reconstruct the nose structure with bone grafts. Although the rib is more malleable, we prefer to use the parietal bone because of its proximity to the surgical area and to avoid chest scars, especially in males, in whom scars are conspicuous.
The soft tissues are reattached to the skeleton by sutures and the temporal muscle to its original insertion site.
In any case, if the medial canthus ligaments are detached, it is necessary to fix them by means of a transnasal canthopexy. Lateral canthopexy is indicated to provide direction to the palpebral fissures but without lateral traction that opposes the medial canthopexy.
In many cases the interciliary distance is increased and therefore it is necessary to resect a vertical ellipse of skin between both eyebrows (Figure 59.7).
Facial Bipartition
This procedure, proposed by van der Meulen,17,18 is used to correct hypertelorism in cases that also have centrofacial shortening and anterior open bite.
During the planning stage, it is important to consider the required proportion of interorbital reduction and centrofacial descent so as to close the open bite. The interorbital bone resection is done in a triangular fashion with upper base, in order to perform medial rotation of both hemifaces, to put both of them in contact at the midline (Figure 59.8).
The geometric method described by Ortiz Monasterio19 for this procedure is very didactic. It considers the hemiface as a trapezoidal structure, the upper limit of which is represented by the lower osteotomy of the craniotomy and its lower limit by the alveolar ridge of the maxilla on the same side.
After bifrontal craniotomy, the same periorbital and intraorbital osteotomies described for the orbital medialization are performed, except for the one underneath the infraorbital nerve in the maxilla. Also, the osteotomy on the lateral wall of the orbit is prolonged downward to the pterygomaxillary joint.
Once the desired interorbital distance has been estimated, the triangular interorbital redundant bone segment is resected, with an upper base at the level of the lower limit of the craniotomy [Figure 59.8(a)]. Depending on the location of its vertex, the resulting effect of the hemiface rotation may vary. If placed at the level of the maxillary alveolar ridge, it allows hemiface rotation to horizontalize the maxillae, but if the vertex is located on the nasal spine, they are horizontalized and expanded in a transverse fashion. It is important to plan the modifications of the maxillae to achieve a stable occlusion.20
In the first case, it is necessary to resect the nasal spine and the junction between the palatine processes all along the nasal floor. These osteotomies are performed through a superior buccal vestibular incision that extends from one canine to the other.
The dysjunction of the pterygomaxillary joint is performed by introducing a curved chisel behind the alveolar process. This maneuver may be done from above through the temporal fossa or through the mouth in the upper vestibule.
Once the osteotomies have been completed, both hemifaces are rotated medially and caudally until they are in contact with each other on the midline and with the inferior border of the frontal bone. This rotation corrects orbital excyclorotation and the antimongoloid tilting of the palpebral fissures.
a |
|
|
|
|
|
|
|
b |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
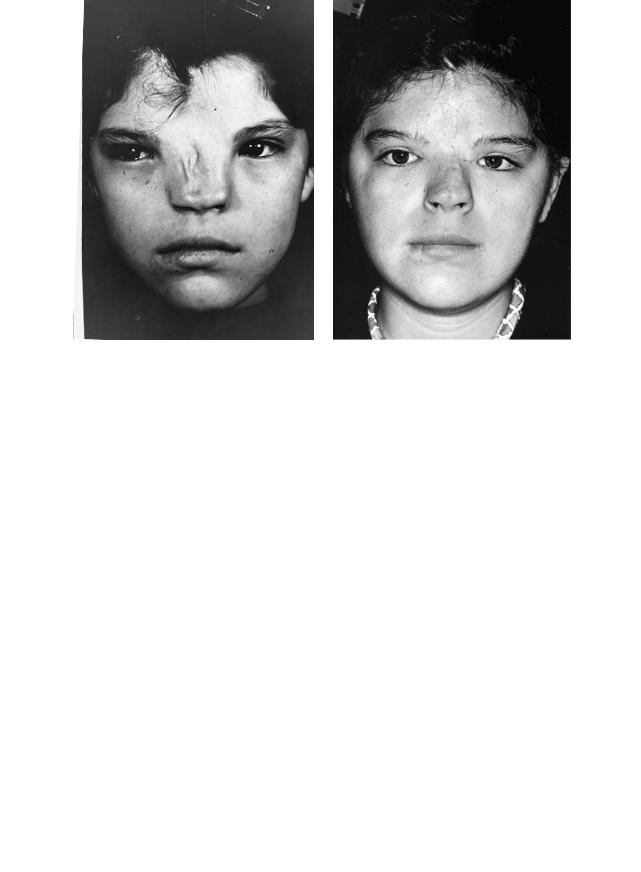
FIGURE 59.7 (a) A 19-year-old female patient with grade III hypertelorism and Tessier 0–14, and right 1–13 facial clefts. (b) Eighteen months after facial bipartition by intracranial approach and centrofacial skin resection.
a |
b |
FIGURE 59.8 Facial bipartition through an intracranial approach. (a) Osteotomies and triangular interorbital bone resection. (b) Medial rotation of both hemifaces and location of the plates used for fixation.
744 |
A. Fuente del Campo |
FIGURE 59.9 Facial bipartition and medial rotation with advancement. Location of the fixation plates: fronto-orbital, maxilla, and lateroinferior orbital angles.
Often, this displacement also takes the hemifaces to a more anterior plane, giving a better projection to the orbits and malar bones.
In these cases with tridimensional mobilization it is especially important to achieve a stable fixation. For this effect, we use titanium miniplates and screws. A T-shaped plate is placed vertically but inverted on the midline of the frontoorbital region (Figure 59.8b) with the double function of maintaining the medialization of the orbits and the centrofacial elongation. To align and stabilize the alveolar processes, another miniplate is placed on a horizontal position at the premaxillary level with a minimum of three screws at each end, making sure that the dental roots are spared.
In cases in which this maneuver is combined with the advancement of the orbits (Apert syndrome), we use one more plate on each side. The plate is bent in an L or U shape, depending on the case, and it is located under pressure in between the lateral-inferior orbital angle and the temporal bone. It has seldom been necessary to fix these plates with screws (Figure 59.9).21
The fronto-orbital triangular defect resulting from the rotation of the hemifaces is filled with bone grafts. In cases in which “nasal salvage” osteotomies are performed, the nasal pyramid is rotated back to its original position and fixed at
the desired height by means of an osteosynthesis wire or screw (Figure 59.10).
Extracranial Procedures
These procedures are limited to patients with grade I hypertelorism, provided that the cribriform plate is not descended more than 10 mm below the upper orbital rim, as measured on the AP cephalometry.
With extracranial procedures in hypertelorism of a higher grade it is not possible to obtain cosmetic results as good as those of intracranial procedures. Nevertheless, such procedures might be indicated for cases having any other contraindication for an intracranial approach. The subcranial approach may be used both for orbital medialization and centrofacial rotation.
The orbital medialization is started in the interorbital region, resecting two vertical paramedian segments, trying to spare the medial wall of the orbits and the nasal pyramid. The latter is indicated only if we wish to preserve the original shape of the nose.
Starting on the superior end of the resected bony area, the osteotomy is continued toward the medial orbital wall, aiming it backwards horizontally, going 0.5 cm behind the vertical axis of the eye globe. We continue downwards along the medial wall and proceed along the orbital floor and the full thickness of the orbital lateral wall, ending the osteotomy at the junction between this wall and the roof. The osteotomy is completed by sectioning the zygomatic arch and, horizontally, the maxilla, from the malar bone to the piriform aperture as described for the intracranial procedure (Figure 59.11a).
Once the orbital pieces have been mobilized, they are taken to the midline, having previously resected a proportional segment of the ethmoidal cells (Figure 59.11b).
The centrofacial rotation is done in a similar fashion, but the side-wall osteotomy goes down all the way to the pterygomaxillary junction, and the horizontal osteotomy of the maxilla is avoided. Both bone segments are rotated toward the midline and immobilized with wire at the nasal level and with a titanium miniplate and screws in the alveolar region (Figure 59.12).
We recommend preserving the original insertion of the medial canthal ligaments. Whenever this is not possible, it is necessary to reattach them by means of a canthopexy.
In some cases, the shape of the naso-orbital region is not adequate to achieve a cosmetic result by means of paranasal bone resections. Therefore, we prefer to rotate the nasal pyramid toward the front and perform the frontoethmoidal resection at the center as we described it for the intracranial approach (nasal salvage).
Soft Tissues
The treatment of hypertelorism should focus on both of the bony structural and the soft tissue alterations. The management
59. Orbital Hypertelorism: Surgical Management |
745 |
|||||||
a |
|
|
|
|
|
b |
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
FIGURE 59.10 (a) A 4-year-old male patient with hypertelorism, open bite, and Tessier 2–12 cleft. (b) Two years after facial bipartition and cleft repair.
a |
b |
FIGURE 59.11 Orbital medialization through subcranial approach. (a) Osteotomies and interorbital bone resection. (b) New position and osteosynthesis of the orbital segments.

746 |
A. Fuente del Campo |
a |
b |
FIGURE 59.12 Subcranial orbital rotation. (a) Osteotomies and triangular interorbital bone resection. (b) Medial rotation of both orbital pieces and their fixation by means of osteosynthesis and one plate on the maxillae.
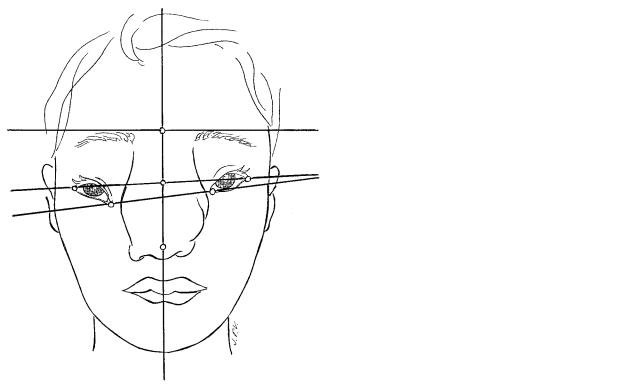
FIGURE 59.13 Lines, points, and distances considered in evaluating the proportional centrofacial T. (Reprinted with permission from Ann Plast Surg.)
59. Orbital Hypertelorism: Surgical Management |
747 |
TABLE 59.1 Nasoorbital anthropometry of 100 patients. |
|
|
tures, we routinely use the centrofacial anthropometry, which |
|||
|
|
|
|
|
|
allows us to determine precisely the proportional alterations |
|
|
Mean |
|
|
||
|
|
|
|
of the patient and plan the desired result based on the mea- |
||
|
distance (mm) |
General |
||||
|
|
|
|
surements considered to be normal. For this purpose, we use |
||
Points measured |
Men |
Women |
mean (mm) |
|||
|
|
|
|
|
|
a method that we have called proportional centrofacial T, as |
Medial intercanthal |
31.8 |
31.5 |
|
31.65 |
|
|
|
|
we reported in 1989, which is based on an anthropometric |
||||
Lateral intercanthal |
90.5 |
89.8 |
|
90.15 |
|
|
|
|
study of 50 males and 50 females and allowed us to obtain |
||||
Interciliary line to nasal tip |
60.3 |
53.7 |
|
57.00 |
|
|
Lateral canthal line to nasal tip |
40.7 |
37.4 |
|
39.05 |
|
normal average values, as well as the normal proportional in- |
Interciliary line to lateral |
19.6 |
16.3 |
|
17.95 |
|
terrelation of the following measurements (Figure 59.13): me- |
canthal line |
|
|
|
|
|
dial intercanthal distance (MID), lateral intercanthal distance |
Lateral canthal line to |
2.2 |
1.8 |
|
2.00 |
|
|
|
|
(LID), interciliary line (ICL) to lateral canthal line (LCL), in- |
||||
medial canthal line |
|
|
|
|
|
|
|
|
|
|
|
terciliary line (ICL) to tip of the nose (NT), lateral canthal |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
line to tip of the nose, and medial canthal line (MCL) to lat- |
|
|
|
|
|
|
eral canthal line (Table 59.1).22 The point of maximal nose |
of the bone structures and their displacement is not more im- |
projection was considered as the tip of the nose. We refer to |
|||||
portant than that of the soft tissues; each of the facial struc- |
the tip of the nose and not to the subnasal point or other points |
|||||
tures must be correctly repositioned according to the appro- |
of bone landmarks because the purpose is to correct the soft |
|||||
priate proportions. |
|
|
|
|
|
tissues. We do not consider other points of central facial land- |
Once the bony reconstruction has been completed, we at- |
marks, such as the nasion or glabella, because distortions were |
|||||
tach the soft tissues to their corresponding position on the |
found in these patients. |
|||||
bone structure by means of deep 4-0 Vicryl sutures. Other- |
The proportional relationship among the average measure- |
|||||
wise, the outcome would leave much to be desired due to skin |
ments of these normal subjects was determined to assist in |
|||||
laxity, the scar, and the fibrous tissue that will fill the result- |
the assessment of our patients and to determine the desirable |
|||||
ing dead spaces between the soft tissues and the bone. |
outcome. We found that the distance from the ICL to the tip |
|||||
To be more accurate in the repositioning of facial struc- |
of the nose represented 60% of the lateral intercanthal dis- |
|||||
a |
|
|
|
|
|
b |
FIGURE 59.14 (a) Anthropometric lines, points, and distances to be considered for the soft tissue reconstruction of a patient with hypertelorism and encephalomeningocele. (b) Osteotomies and in-
terorbital bone resection planned for the simultaneous correction of hypertelorism and the cranial bone defect of the same patient.
748
tance. The vertical measurement between the ICL and the tip of the nose is divided by the LCL into an upper third (20% of the lateral intercanthal distance) and two lower thirds (40% of the same distance). Variants of 2 mm are considered as normal. The MCL was found to be, on average, 2 mm below the LCL. The medial intercanthal distance represents one third of the lateral intercanthal distance, same as the length of each of the palpebral fissures. Based on these relationships, the proportional centrofacial T helps us to accurately plan the surgery directly on each patient, particularly in patients with soft tissue malformations (clefts, meningoencephaloceles; see Figure 59.14).
Orbital hypertelorism or teleorbitism is an impressive and socially disabling deformity. Owing to its complexity, it requires the use of radical, ambitious and aggressive techniques that give the patient an appearance that is consistent with the patterns considered as normal. To facilitate the social adaptation of children to their environment and to allow the development of a normal binocular vision, these patients should be treated surgically before they reach school age, preferably between the age of 2 to 3 years.
This is a complex surgery, full of important details, requiring accurate assessment, planning, and execution. Therefore, a skilled and experienced multidisciplinary surgical and parasurgical team is necessary.
References
1.Grieg DM. Hypertelorism, a hitherto undifferentiated congenital craniofacial deformity. Edinb Med J. 1924;31:560.
2.Gunther H. Konstitutionelle Anomalien der Augenabstandes und der Interorbitalbreite. Virchows Arch Pathol Anat. 1933;290:373.
3.Currarino G, Silverman FN. Orbital hypertelorism, arrhinencephaly. Radiology. 1960;74:206.
4.Hasman CF. Growth of interorbital distance and skull thickness as observed in roentgenographic measurements. Radiology. 1966;86:87.
5.Tessier P. Orbital hypertelorism I. Scand J Plast Reconstr Surg. 1972;6:135.
6.Tessier P. Orbital hypertelorism II. Scand J Plast Reconstr Surg. 1973;7:39.
A. Fuente del Campo
7.Tessier P. Orbital hypertelorism. Symposium on Plastic Surgery in the Orbital Region. Vol. 12. St. Louis: CV Mosby; 1976:255– 267.
8.Walker DG. Malformations of the Face. Edinburgh: Livingstone; 1961.
9.Vermeij-Keers C, Poelman RE, Smits van Pooje AE, Van de Meulen JC. Hypertelorism and the median cleft face syndrome. An embryological analysis. Ophthalmic Paediatr Genet. 1984;4:97.
10.Converse JM, Ransohoff J, Mathews ES, Smith B, Moleonar A. Ocular hypertelorism and pseudohypertelorism. Plast Reconstr Surg. 1970;45:1.
11.Fuente del Campo A, Ortiz Monasterio F. Hipertelorismo o teleorbitismo. An Medicos. 1978;23:153.
12.Psillakis JM. Surgical treatment of hypertelorism. In: Caronni E, ed. Craniofacial Surgery. Boston: Little-Brown; 1985.
13.Raposo Do Amaral C. Surgical Treatment of Orbital Hyperand Hypotelorism. In: Marchac D, ed. Craniofacial Surgery. Berlin: Springer-Verlag; 1987.
14.Tessier P, Tulasne JF. Stability in correction of hyperteleorbitism and Treacher Collins syndromes. Clin Plast Surg. 1989; 16:195.
15.Ortiz Monasterio F, Fuente del Campo A. Nasal correction in hyperteleorbitism: the short and the long nose. Scand J Plast Surg. 1981;15:277.
16.Fuente del Campo A. Nose salvation in craniofacial surgery. Presented at the V International Congress of the International Society of Craniofacial Surgery. Oaxaca, Mexico; 1993.
17.Van Der Meulen JC. Medial Faciotomy. Br J Plast Surg. 1979;33:339.
18.van der Meulen JC, Vaandragen JH. Surgery related to correction of hypertelorism. Plast Reconstr Surg 1983;61:6.
19.Ortiz Monasterio F, Medina O, Musolas A. Geometrical planning for the correction of orbital hypertelorism. Plast Reconstr Surg. 1990;86:650.
20.Tessier P. Facial bipartition: a concept more than a procedure. In: Marchac D, ed. Craniofacial Surgery. Berlin: SpringerVerlag; 1987.
21.Fuente del Campo A. Rigid fixation and osteotomy design in frontal orbital advancement osteotomies. Clin Plast Surg. 1989; 16:205.
22.Fuente del Campo A, Escanero A, Baldizon N, Dimopulos A. Transfacial surgical treatment and anthropometric considerations of frontoethmoidal meningoencephaloceles. Ann Plast Surg. 1989;23:377.
