
- •Hematuria II: causes and investigation
- •Hematospermia
- •Lower urinary tract symptoms (LUTS)
- •Nocturia and nocturnal polyuria
- •Flank pain
- •Urinary incontinence in adults
- •Genital symptoms
- •Abdominal examination in urological disease
- •Digital rectal examination (DRE)
- •Lumps in the groin
- •Lumps in the scrotum
- •2 Urological investigations
- •Urine examination
- •Urine cytology
- •Radiological imaging of the urinary tract
- •Uses of plain abdominal radiography (KUB X-ray—kidneys, ureters, bladder)
- •Intravenous pyelography (IVP)
- •Other urological contrast studies
- •Computed tomography (CT) and magnetic resonance imaging (MRI)
- •Radioisotope imaging
- •Post-void residual urine volume measurement
- •3 Bladder outlet obstruction
- •Regulation of prostate growth and development of benign prostatic hyperplasia (BPH)
- •Pathophysiology and causes of bladder outlet obstruction (BOO) and BPH
- •Benign prostatic obstruction (BPO): symptoms and signs
- •Diagnostic tests in men with LUTS thought to be due to BPH
- •Why do men seek treatment for their symptoms?
- •Watchful waiting for uncomplicated BPH
- •Medical management of BPH: combination therapy
- •Medical management of BPH: alternative drug therapy
- •Minimally invasive management of BPH: surgical alternatives to TURP
- •Invasive surgical alternatives to TURP
- •TURP and open prostatectomy
- •Indications for and technique of urethral catheterization
- •Indications for and technique of suprapubic catheterization
- •Management of nocturia and nocturnal polyuria
- •High-pressure chronic retention (HPCR)
- •Bladder outlet obstruction and retention in women
- •Urethral stricture disease
- •4 Incontinence
- •Causes and pathophysiology
- •Evaluation
- •Treatment of sphincter weakness incontinence: injection therapy
- •Treatment of sphincter weakness incontinence: retropubic suspension
- •Treatment of sphincter weakness incontinence: pubovaginal slings
- •Overactive bladder: conventional treatment
- •Overactive bladder: options for failed conventional therapy
- •“Mixed” incontinence
- •Post-prostatectomy incontinence
- •Incontinence in the elderly patient
- •Urinary tract infection: microbiology
- •Lower urinary tract infection
- •Recurrent urinary tract infection
- •Urinary tract infection: treatment
- •Acute pyelonephritis
- •Pyonephrosis and perinephric abscess
- •Other forms of pyelonephritis
- •Chronic pyelonephritis
- •Septicemia and urosepsis
- •Fournier gangrene
- •Epididymitis and orchitis
- •Periurethral abscess
- •Prostatitis: presentation, evaluation, and treatment
- •Other prostate infections
- •Interstitial cystitis
- •Tuberculosis
- •Parasitic infections
- •HIV in urological surgery
- •6 Urological neoplasia
- •Pathology and molecular biology
- •Prostate cancer: epidemiology and etiology
- •Prostate cancer: incidence, prevalence, and mortality
- •Prostate cancer pathology: premalignant lesions
- •Counseling before prostate cancer screening
- •Prostate cancer: clinical presentation
- •PSA and prostate cancer
- •PSA derivatives: free-to-total ratio, density, and velocity
- •Prostate cancer: transrectal ultrasonography and biopsies
- •Prostate cancer staging
- •Prostate cancer grading
- •General principles of management of localized prostate cancer
- •Management of localized prostate cancer: watchful waiting and active surveillance
- •Management of localized prostate cancer: radical prostatectomy
- •Postoperative course after radical prostatectomy
- •Prostate cancer control with radical prostatectomy
- •Management of localized prostate cancer: radical external beam radiotherapy (EBRT)
- •Management of localized prostate cancer: brachytherapy (BT)
- •Management of localized and radiorecurrent prostate cancer: cryotherapy and HIFU
- •Management of locally advanced nonmetastatic prostate cancer (T3–4 N0M0)
- •Management of advanced prostate cancer: hormone therapy I
- •Management of advanced prostate cancer: hormone therapy II
- •Management of advanced prostate cancer: hormone therapy III
- •Management of advanced prostate cancer: androgen-independent/ castration-resistant disease
- •Palliative management of prostate cancer
- •Prostate cancer: prevention; complementary and alternative therapies
- •Bladder cancer: epidemiology and etiology
- •Bladder cancer: pathology and staging
- •Bladder cancer: presentation
- •Bladder cancer: diagnosis and staging
- •Muscle-invasive bladder cancer: surgical management of localized (pT2/3a) disease
- •Muscle-invasive bladder cancer: radical and palliative radiotherapy
- •Muscle-invasive bladder cancer: management of locally advanced and metastatic disease
- •Bladder cancer: urinary diversion after cystectomy
- •Transitional cell carcinoma (UC) of the renal pelvis and ureter
- •Radiological assessment of renal masses
- •Benign renal masses
- •Renal cell carcinoma: epidemiology and etiology
- •Renal cell carcinoma: pathology, staging, and prognosis
- •Renal cell carcinoma: presentation and investigations
- •Renal cell carcinoma: active surveillance
- •Renal cell carcinoma: surgical treatment I
- •Renal cell carcinoma: surgical treatment II
- •Renal cell carcinoma: management of metastatic disease
- •Testicular cancer: epidemiology and etiology
- •Testicular cancer: clinical presentation
- •Testicular cancer: serum markers
- •Testicular cancer: pathology and staging
- •Testicular cancer: prognostic staging system for metastatic germ cell cancer
- •Testicular cancer: management of non-seminomatous germ cell tumors (NSGCT)
- •Testicular cancer: management of seminoma, IGCN, and lymphoma
- •Penile neoplasia: benign, viral-related, and premalignant lesions
- •Penile cancer: epidemiology, risk factors, and pathology
- •Squamous cell carcinoma of the penis: clinical management
- •Carcinoma of the scrotum
- •Tumors of the testicular adnexa
- •Urethral cancer
- •Wilms tumor and neuroblastoma
- •7 Miscellaneous urological diseases of the kidney
- •Cystic renal disease: simple cysts
- •Cystic renal disease: calyceal diverticulum
- •Cystic renal disease: medullary sponge kidney (MSK)
- •Acquired renal cystic disease (ARCD)
- •Autosomal dominant (adult) polycystic kidney disease (ADPKD)
- •Ureteropelvic junction (UPJ) obstruction in adults
- •Anomalies of renal ascent and fusion: horseshoe kidney, pelvic kidney, malrotation
- •Renal duplications
- •8 Stone disease
- •Kidney stones: epidemiology
- •Kidney stones: types and predisposing factors
- •Kidney stones: mechanisms of formation
- •Evaluation of the stone former
- •Kidney stones: presentation and diagnosis
- •Kidney stone treatment options: watchful waiting
- •Stone fragmentation techniques: extracorporeal lithotripsy (ESWL)
- •Intracorporeal techniques of stone fragmentation (fragmentation within the body)
- •Kidney stone treatment: percutaneous nephrolithotomy (PCNL)
- •Kidney stones: open stone surgery
- •Kidney stones: medical therapy (dissolution therapy)
- •Ureteric stones: presentation
- •Ureteric stones: diagnostic radiological imaging
- •Ureteric stones: acute management
- •Ureteric stones: indications for intervention to relieve obstruction and/or remove the stone
- •Ureteric stone treatment
- •Treatment options for ureteric stones
- •Prevention of calcium oxalate stone formation
- •Bladder stones
- •Management of ureteric stones in pregnancy
- •Hydronephrosis
- •Management of ureteric strictures (other than UPJ obstruction)
- •Pathophysiology of urinary tract obstruction
- •Ureter innervation
- •10 Trauma to the urinary tract and other urological emergencies
- •Renal trauma: clinical and radiological assessment
- •Renal trauma: treatment
- •Ureteral injuries: mechanisms and diagnosis
- •Ureteral injuries: management
- •Bladder and urethral injuries associated with pelvic fractures
- •Bladder injuries
- •Posterior urethral injuries in males and urethral injuries in females
- •Anterior urethral injuries
- •Testicular injuries
- •Penile injuries
- •Torsion of the testis and testicular appendages
- •Paraphimosis
- •Malignant ureteral obstruction
- •Spinal cord and cauda equina compression
- •11 Infertility
- •Male reproductive physiology
- •Etiology and evaluation of male infertility
- •Lab investigation of male infertility
- •Oligospermia and azoospermia
- •Varicocele
- •Treatment options for male factor infertility
- •12 Disorders of erectile function, ejaculation, and seminal vesicles
- •Physiology of erection and ejaculation
- •Impotence: evaluation
- •Impotence: treatment
- •Retrograde ejaculation
- •Peyronie’s disease
- •Priapism
- •13 Neuropathic bladder
- •Innervation of the lower urinary tract (LUT)
- •Physiology of urine storage and micturition
- •Bladder and sphincter behavior in the patient with neurological disease
- •The neuropathic lower urinary tract: clinical consequences of storage and emptying problems
- •Bladder management techniques for the neuropathic patient
- •Catheters and sheaths and the neuropathic patient
- •Management of incontinence in the neuropathic patient
- •Management of recurrent urinary tract infections (UTIs) in the neuropathic patient
- •Management of hydronephrosis in the neuropathic patient
- •Bladder dysfunction in multiple sclerosis, in Parkinson disease, after stroke, and in other neurological disease
- •Neuromodulation in lower urinary tract dysfunction
- •14 Urological problems in pregnancy
- •Physiological and anatomical changes in the urinary tract
- •Urinary tract infection (UTI)
- •Hydronephrosis
- •15 Pediatric urology
- •Embryology: urinary tract
- •Undescended testes
- •Urinary tract infection (UTI)
- •Ectopic ureter
- •Ureterocele
- •Ureteropelvic junction (UPJ) obstruction
- •Hypospadias
- •Normal sexual differentiation
- •Abnormal sexual differentiation
- •Cystic kidney disease
- •Exstrophy
- •Epispadias
- •Posterior urethral valves
- •Non-neurogenic voiding dysfunction
- •Nocturnal enuresis
- •16 Urological surgery and equipment
- •Preparation of the patient for urological surgery
- •Antibiotic prophylaxis in urological surgery
- •Complications of surgery in general: DVT and PE
- •Fluid balance and management of shock in the surgical patient
- •Patient safety in the operating room
- •Transurethral resection (TUR) syndrome
- •Catheters and drains in urological surgery
- •Guide wires
- •JJ stents
- •Lasers in urological surgery
- •Diathermy
- •Sterilization of urological equipment
- •Telescopes and light sources in urological endoscopy
- •Consent: general principles
- •Cystoscopy
- •Transurethral resection of the prostate (TURP)
- •Transurethral resection of bladder tumor (TURBT)
- •Optical urethrotomy
- •Circumcision
- •Hydrocele and epididymal cyst removal
- •Nesbit procedure
- •Vasectomy and vasovasostomy
- •Orchiectomy
- •Urological incisions
- •JJ stent insertion
- •Nephrectomy and nephroureterectomy
- •Radical prostatectomy
- •Radical cystectomy
- •Ileal conduit
- •Percutaneous nephrolithotomy (PCNL)
- •Ureteroscopes and ureteroscopy
- •Pyeloplasty
- •Laparoscopic surgery
- •Endoscopic cystolitholapaxy and (open) cystolithotomy
- •Scrotal exploration for torsion and orchiopexy
- •17 Basic science of relevance to urological practice
- •Physiology of bladder and urethra
- •Renal anatomy: renal blood flow and renal function
- •Renal physiology: regulation of water balance
- •Renal physiology: regulation of sodium and potassium excretion
- •Renal physiology: acid–base balance
- •18 Urological eponyms
- •Index

Chapter 11 |
465 |
|
|
Infertility
Male reproductive physiology 466
Etiology and evaluation of male infertility 470
Lab investigation of male infertility 472
Oligospermia and azoospermia 476
Varicocele 478
Treatment options for male factor infertility 480

466 CHAPTER 11 Infertility
Male reproductive physiology
Hypothalamic–pituitary–testicular axis
The hypothalamus secretes luteinizing hormone–releasing hormone (LHRH), also known as gonadotrophin-releasing hormone (GnRH). This causes pulsatile release of anterior pituitary gonadotrophins, called folli- cle-stimulating hormone (FSH) and luteinizing hormone (LH), which act on the testis.
FSH stimulates the seminiferous tubules to secrete inhibin and produce sperm; LH acts on Leydig cells to produce testosterone (Fig. 11.1).
Testosterone
Testosterone is secreted by the interstitial Leydig cells, which lie adjacent to the seminiferous tubules in the testis. It promotes development of the male reproductive system and secondary sexual characteristics.
Steroidogenesis is stimulated by a cAMP-protein kinase C mechanism, which converts cholesterol to pregnenolone. Further steps in the biosynthesis pathway produce intermediary substances (dehydroepiandrosterone and androstenedione) prior to producing testosterone.
In the blood, testosterone is attached to sex hormone–binding globulin (SHBG) and albumin. At androgen-responsive target tissues, testosterone is converted into a potent androgen, dihydrotestosterone (DHT), by intracellular 5A-reductase (see p. 64).
Spermatogenesis
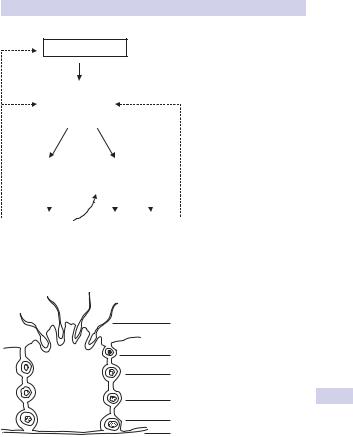
Seminiferous tubules are lined with Sertoli cells, which surround developing germ cells (spermatogonia) providing nutrients and stimulating factors, as well as secreting androgen-binding factor and inhibin (Fig. 11.2).
Primordial germ cells (spermatogonia) divide via mitosis to form primary spermatocytes. These undergo a first meiotic division to create secondary spermatocytes (46 chromosomes), followed by a second meiotic division to form spermatids (23 chromosomes). Finally, these differentiate into spermatozoa.
Spermatogenesis takes 74 days. The nonmotile spermatozoa leave the seminiferous tubules and pass to the epididymis, where they undergo maturation (gain motility and the ability to fertilized). Ductal transit time takes another 2 weeks, so the total time from beginning of spermatogenesis to ejaculation is 3 months.
Motile sperm are stored in the globus minor of the epididymis until ejaculation. Spermatozoa that are not released are reabsorbed by phagocytosis.
Mature sperm
Mature sperm have a head, middle piece, and tail (Fig. 11.3). The head is composed of a nucleus covered by an acrosome cap, containing vesicles filled with lytic enzymes that break down the outer layer of the female ovum. The middle piece contains mitochondria and contractile filaments, which extend into the tail to aid motility.
MALE REPRODUCTIVE PHYSIOLOGY 467
– ve
HYPOTHALAMUS
LHRH
– ve |
|
|
ANTERIOR |
|
|
–ve |
||
|
|
|
PITUITARY |
|
|
|
|
|
|
|
|
GLAND |
|
|
|
|
|
|
LH |
|
FSH |
|||||
|
|
|
TESTIS |
|
|
|
|
|
|
|
|
|
|
||||
Interstitial cells |
Seminiferous tubules |
|||||||
(Leydig cells) |
(Sertoli cells) |
|||||||
|
|
|
|
|
||||
|
|
|
|
|
|
|||
Testosterone |
|
Sperm Inhibin |
||||||
|
Lumen |
|
|
|
|
|
||
Figure 11.1 Hypothalamic–pituitary–testicular axis.
|
Spermatozoa |
|
Spermatid |
|
2º spermatocyte |
Sertoli cell |
1º spermatocyte |
|
|
|
Spermatogonia |
|
Basal lamina |
Figure 11.2 Spermatogenesis in the seminiferous tubules of the testis.

468 CHAPTER 11 Infertility
Head:
Plasma membrane
Acrosomal cap
Nucleus
Middle piece:
Proximal centriole
Mitochrondria
Microtubules
Tail:
Principal piece
Figure 11.3 A spermatozoon.
Tail:
End piece
After deposition at the cervix, sperm penetrate cervical mucus and travel through the uterus to the site of fertilization in the fallopian tube. Along the way, within the female reproductive tract, they undergo capacitation—a further activation of their ability to fertilize marked by an increase in their motility.
When a sperm penetrates the oocyte, it binds to the zona pellucida, which alters its permeability so that other sperm cannot penetrate the ovum, leading to enzyme release, penetration into the cytoplasm of the oocyte, fusion, and fertilization.
This page intentionally left blank
