
Lesson topic №27 ХСН (Сhronic heart failure )
.pdf
Сhronic heart failure in the outpatient setting
Gerasimenko I.A. Department of polyclinic therapy with course of general medical practice (family medicine)

Heart failure
Heart failure is not a single pathological diagnosis, but a clinical syndrome consisting of cardinal symptoms (e.g. breathlessness, ankle swelling, and fatigue) that may be accompanied by signs (e.g. elevated jugular venous pressure, pulmonary crackles, and peripheral oedema). It is due to a structural and/or functional abnormality of the heart that results in elevated intracardiac pressures and/or inadequate cardiac output at rest and/or during exercise.

Causes of heart failure
Cause |
Examples of presentations |
|
|
Coronary artery disease |
Myocardial infarction |
|
Angina or “angina-equivalent” |
|
Arrhythmias |
|
|
Hypertension |
Heart failure with preserved systolic function Malignant |
|
hypertension/acute pulmonary oedema |
|
|
Valve disease |
Primary valve disease e.g., aortic stenosis Secondary |
|
valve disease, e.g. functional regurgitation |
|
Congenital valve disease |
|
|
Arrhythmias |
Atrial tachyarrhythmias |
|
Ventricular arrhythmias |
|
|
CMPs |
Dilated |
|
Hypertrophic |
|
Restrictive |
|
ARVC |
|
Peripartum |
|
Takotsubo syndrome |
|
Toxins: alcohol, cocaine, iron, copper |
|
|

Causes of heart failure
Cause |
Examples of presentations |
|
|
Congenital heart disease |
Congenitally corrected/repaired transposition of great |
|
arteries |
|
Shunt lesions |
|
Repaired tetralogy of Fallot Ebstein’s anomaly |
|
|
Infective |
Viral myocarditis |
|
Chagas disease |
|
HIV |
|
Lyme disease |
|
|
Drug-induced |
Anthracyclines |
|
Trastuzumab |
|
VEGF inhibitors |
|
Immune checkpoint inhibitors |
|
Proteasome inhibitors |
|
RAF+MEK inhibitors |
|
|
Infiltrative |
Amyloid |
|
Sarcoidosis |
|
Neoplastic |
|
|

Causes of heart failure
Cause |
Examples of presentations |
|
|
Storage disorders |
Haemochromatosis |
|
Fabry disease |
|
Glycogen storage diseases |
|
|
Endomyocardial disease |
Radiotherapy |
|
Endomyocardial fibrosis/eosinophilia Carcinoid |
|
|
Pericardial disease |
Calcification Infiltrative |
|
|
Metabolic |
Endocrine disease |
|
Nutritional disease (thiamine, vitamin B1 and selenium |
|
deficiencies) |
|
Autoimmune disease |
|
|
Neuromuscular disease |
Friedreich’s ataxia |
|
Muscular dystrophy |
|
|
Heart failure
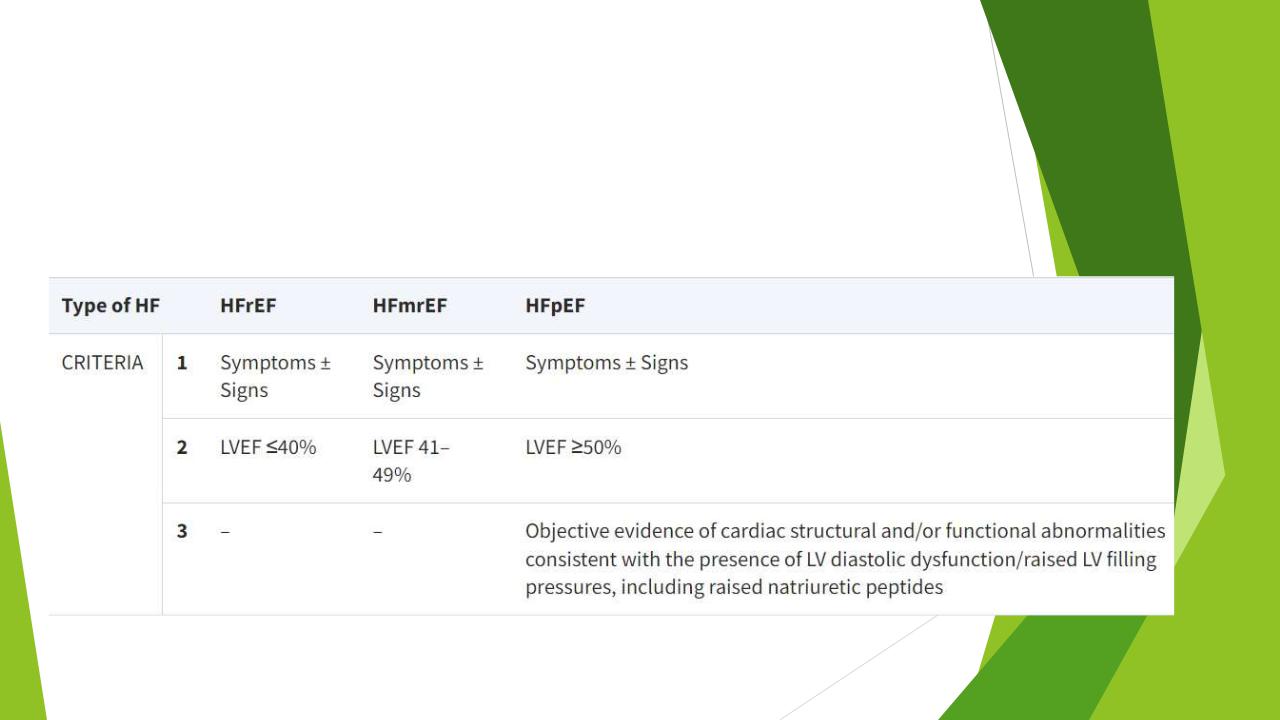
Traditionally, HF has been divided into distinct phenotypes based on the measurement of left ventricular ejection fraction (LVEF)

Heart failure
Reduced LVEF is defined as ≤40%, i.e. those with a significant reduction in LV systolic function. This is designated as Heart failure with reduced ejection fraction (HFrEF).
Patients with a LVEF between 41% and 49% have mildly reduced LV systolic function, i.e. HFmrEF.
Patients with symptoms and signs of HF, with evidence of structural and/or functional cardiac abnormalities and/or raised natriuretic peptides (NPs), and with an LVEF ≥50%, have Heart failure with preserved ejection fraction (HFpEF).

Classification
The simplest terminology used to describe the severity of HF is the New York Heart Association (NYHA) functional classification.

Classification
HF stages (by VasilenkoStrazhesko)
Stage I - the initial stage the latent heart failure, marked only with exertion (dyspnea, palpitations, fatigue). Hemodynamics is normal.
Stage II - a long standing, severe form of heart failure. Overt hemodynamic abnormalities are present at rest.
Substage A – hemodynamic abnormalities are moderate and are present only in one (large or small) circulation circle, i.e. one ventricular (left or right) failure.
Substage B – hemodynamic abnormalities are severe and are present throughout the cardiovascular system (manifested in the large AND small circulation circles), i.e. biventricular failure.
Stage III - the final, dystrophic stage with severe hemodynamics impairment, significant disorders of metabolism and irreversible changes in the structure of tissues and organs.

Diagnosis of chronic heart failure
The diagnosis of CHF requires the presence of symptoms and/or signs of HF and objective evidence of cardiac dysfunction.
The diagnosis of CHF is made more likely in patients with a history of MI, arterial hypertension, CAD, diabetes mellitus, alcohol misuse, chronic kidney disease (CKD), cardiotoxic chemotherapy, and in those with a family history of CMP or sudden death.
