
6. The content of the lecture material.
1 Classification
1.1 Variation in definition and terminology
1.2 Classification by cause and symptoms
2 Signs and symptoms
3 Pathophysiology
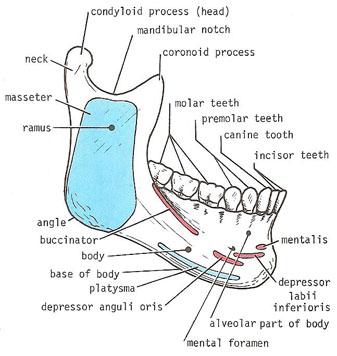
3.1 Anatomy and physiology of the mastication system
3.1.1 Temporomandibular joints
3.1.2 Muscles of mastication
3.2 Mechanisms of main signs and symptoms
3.2.1 Joint noises
3.2.2 Pain
3.2.2.1 Arthralgia
3.2.2.2 Myofascial pain
3.2.3 Limitation of mandibular movement
3.3 Specific processes
3.3.1 Disc displacement
3.3.2 Degenerative joint disease
3.4 Theories of underlying causes
3.4.1 Psychosocial factors
3.4.2 Bruxism and other para-functional activities
3.4.3 Trauma
3.4.4 Occlusal factors
3.4.5 Genetic factors
3.4.6 Possible associations
4 Diagnosis
Diagnostic criteria
Psychosocial and behavioral interventions
Occlusal splints
Medication
Physiotherapy, biofeedback and similar non-invasive measures
Occlusal adjustment/reorganization
5 Surgery
-
Arthrocentesis
-
Arthroscopy
-
Intra-articular injections
6 Prognosis
7 References
Classification of disfunction
Muscular:
-
Hyperactivity, spasm, and trismus
-
Inflammation (myositis)
-
Trauma
-
Myofascial pain and fibromyalgia
-
Atrophy or hypertrophy
Arthrogenic:
-
Disc displacement (internal derangement)
-
Hypomobility of the disc (adhesions or scars)
-
Dislocation and subluxation
-
Arthritis
-
Infections
-
Metabolic disease (gout, chondrocalcinosis)
-
Capsulitis, synovitis
-
Ankylosis (fibrous or bony)
-
Fracture
-
Condylar hyperplasia, hypoplasia or aplasia
-
Neoplasia
Group I: muscle disorders
Ia. Myofascial pain:
-
Report of pain or ache in the jaw, temples, face, preauricular area, or inside the ear at rest or during function;
-
Pain reported by the subject in response to palpation of 3 of the following muscle sites (right side and left side count as a separate sites for each muscle): posterior temporalis, middle temporalis, anterior temporalis, origin of masseter, insertion of masseter, posterior mandibular region, submandibular region, lateral pterygoid area, and tendon of the temporalis;
-
At least one of the painful sites must be on the same side as the complaint of pain.
Ib. Myofascial pain with limited opening:
-
Myofascial pain as defined in Ia;
-
Pain-free unassisted mandibular opening 40 mm;
-
Maximum assisted opening (passive stretch) 5 mm greater than pain-free unassisted opening.
Group II: disc displacements
IIa. Disc displacement with reduction:
-
Reciprocal clicking in TMJ (click on both vertical opening and closing that occurs at point 5 mm greater interincisal distance on opening than closing and is eliminated on protrusive opening), reproducible on 2 out of 3 consecutive trials; or
-
Clicking in TMJ on both vertical range of motion (either opening or closing), reproducible on 2 out of 3 consecutive trials, and click during lateral excursion or protrusion, reproducible on 2 out of 3 consecutive trials.
IIb. Disc displacement without reduction with limited opening:
-
History of significant limitation in opening;
-
Maximum unassisted opening 35 mm;
-
Passive stretch increases opening by 4 mm over maximum unassisted opening;
-
Contralateral excursion 7 mm and/or uncorrected deviation to ipsilateral side on opening;
-
Absence of joint sound or presence of joint sounds not meeting criteria for disc displacement with reduction.
IIc. Disc displacement without reduction, without limited opening:
-
History of significant limitation of mandibular opening;
-
Maximum unassisted opening 35 mm;
-
Passive stretch increases opening by 5 mm over maximum unassisted opening;
-
Contralateral excursion 7 mm;
-
Presence of joint sounds not meeting criteria for disc displacement with reduction;
-
In those studies allowing images, imaging conducted by either arthrography or magnetic resonance reveals disc displacement without reduction.
Group III: arthralgia, osteoarthritis, osteoarthrosis
IIIa. Arthralgia:
-
Pain in one or both joint sites (lateral pole and/or posterior attachment) during palpation;
-
One or more of the following self-reports of pain: pain in the region of the joint, pain in the joint during maximum unassisted opening, pain in the joint during assisted opening, and pain in the joint during lateral excursion;
-
For a diagnoses of simple arthralgia, coarse crepitus must be absent.
IIIb. Osteoarthritis of the TMJ:
-
Arthralgia as defined in IIIa;
-
Either coarse crepitus in the joint or radiologic signs of arthrosis.
IIIc. Osteoarthrosis of the TMJ:
-
Absence of all signs of arthralgia;
-
Either coarse crepitus in the joint or radiologic signs of arthrosis.
What is TMJ Disorder?
The temporomandibular joint (TMJ) is the joint that joins your jaw to your skull. This joint is in front of the ears; you can easily locate it by opening and closing your mouth and feeling the joint with your fingers. When there is a problem with the joint, the muscles or the ligaments around this joint, the condition is called TMJ or TMJ disorder.
TMJ disorders-Definition -Temporomandibular joint and muscle disorders (TMJ disorders) are problems or symptoms of the chewing muscles and joints that connect your lower jaw to your skull.
Alternative Names -TMD; Temporomandibular joint disorders; Temporomandibular muscle disorders.
Causes. There are two matching temporomandibular joints -- one on each side of your head, located just in front of your ears. The abbreviation "TMJ" literally refers to the joint but is often used to mean any disorders or symptoms of this region.
Many TMJ-related symptoms are caused by the effects of physical stress on the structures around the joint. These structures include:
-
Cartilage disk at the joint
-
Muscles of the jaw, face, and neck
-
Nearby ligaments, blood vessels, and nerves
-
Teeth
For many people with temporomandibular joint disorders, the cause is unknown. Some causes given for this condition are not well proven. These included:
-
A bad bite or orthodontic braces
-
Stress and tooth grinding. Many people with TMJ problems do not grind their teeth, and many who have been grinding their teeth for a long time do not have problems with their TMJ joint. For some people, the stress associated with this disorder may be caused by the pain as opposed to being the cause of the problem.
Poor posture can also be an important factor in TMJ symptoms. For example, holding the head forward while looking at a computer all day strains the muscles of the face and neck.
Other factors that might make TMJ symptoms worse are stress, poor diet, and lack of sleep.
Many people end up having "trigger points" - contracted muscles in your jaw, head, and neck. Trigger points can refer pain to other areas, causing a headache, earache, or toothache.
Other possible causes of TMJ-related symptoms include arthritis, fractures, dislocations, and structural problems present since birth.
Symptoms. People who have TMJ disorder may have some of the following symptoms:
-
facial pain
-
jaw pain or tenderness of the jaw
-
pain while chewing
-
popping or clicking of the jaw
-
grating sound when opening or closing the mouth
-
dull, aching pain in the face
-
headaches
-
earaches, tinnitus
-
difficulty opening and closing the mouth
-
biting or chewing difficulty or discomfort
-
locked jaw
-
reduced ability to open or close the mouth
-
generalized pain and tenderness around the joint
-
a history of poor sleep or a diagnosed sleep disorder
