
- •Foreword
- •Preface
- •Contents
- •About the Editors
- •Contributors
- •1: Tracheobronchial Anatomy
- •Trachea
- •Introduction
- •External Morphology
- •Internal Morphology
- •Mucous Layer
- •Blood Supply
- •Anatomo-Clinical Relationships
- •Bronchi
- •Main Bronchi
- •Bronchial Division
- •Left Main Bronchus (LMB)
- •Right Main Bronchus (RMB)
- •Blood Supply
- •References
- •2: Flexible Bronchoscopy
- •Introduction
- •History
- •Description
- •Indications and Contraindications
- •Absolute Contraindications
- •Procedure Preparation
- •Technique of FB Procedure
- •Complications of FB Procedure
- •Basic Diagnostic Procedures
- •Bronchoalveolar Lavage (BAL)
- •Transbronchial Lung Biopsy (TBLB)
- •Transbronchial Needle Aspiration (TBNA)
- •Bronchial Brushings
- •Advanced Diagnostic Bronchoscopy
- •EBUS-TBNA
- •Ultrathin Bronchoscopy
- •Transbronchial Lung Cryobiobsy (TBLC)
- •Therapeutic Procedures Via FB
- •LASER Bronchoscopy
- •Electrocautery
- •Argon Plasma Coagulation (APC)
- •Cryotherapy
- •Photodynamic Therapy
- •Airway Stent Placement
- •Endobronchial Valve Placement
- •Conclusion
- •References
- •History and Historical Perspective
- •Indications and Contraindications
- •Procedure Description
- •Procedure Planning
- •Target Approximation
- •Sampling
- •Complications
- •Future Directions
- •Summary and Recommendations
- •References
- •4: Rigid Broncoscopy
- •Innovations
- •Ancillary Equipment
- •Rigid Bronchoscopy Applications
- •Laser Bronchoscopy
- •Tracheobronchial Prosthesis
- •Transbronchial Needle Aspiration (TBNA)
- •Rigid Bronchoscope in Other Treatments for Bronchial Obstruction
- •Mechanical Debridement
- •Pediatric Rigid Bronchoscopy
- •Tracheobronchial Dilatation
- •Foreign Bodies Removal
- •Other Indications
- •Complications
- •The Procedure
- •Some Conclusions
- •References
- •History and Historical Perspective
- •Indications and Contraindications
- •Preprocedural Evaluation and Preparation
- •Physical Examination
- •Procedure-Related Indications
- •Application of the Technique
- •Topical Anesthesia
- •Anesthesia of the Nasal Mucosa and Nasopharynx
- •Anesthesia of the Mouth and Oropharynx
- •Superior Laryngeal Nerve Block
- •Recurrent Laryngeal Nerve Block (RLN)
- •Conscious Sedation
- •Monitored Anesthesia Care (MAC)
- •General Anesthesia
- •Monitoring the Depth of Anesthesia
- •Interventional Bronchoscopy Suites
- •Airway Devices
- •Laryngeal Mask Airway (LMA)
- •Endotracheal Tube (ETT)
- •Rigid Bronchoscope
- •Modes of Ventilation
- •Spontaneous Ventilation
- •Assisted Ventilation
- •Noninvasive Positive Pressure Ventilation (NIV)
- •Positive Pressure Controlled Mechanical Ventilation
- •Jet Ventilation
- •Electronic Mechanical Jet Ventilation
- •Postprocedure Care
- •Special Consideration
- •Anesthesia for Peripheral Diagnostic and Therapeutic Bronchoscopy
- •Anesthesia for Interventional Bronchoscopic Procedures During the COVID-19 Pandemic
- •Summary and Recommendations
- •Conclusion
- •References
- •Background
- •Curricular Structure and Delivery
- •What Is a Bronchoscopy Curriculum?
- •Tradition, Teaching Styles, and Beliefs
- •Using Assessment Tools to Guide the Educational Process
- •The Ethics of Teaching
- •When Learners Teach: The Journey from Novice to Mastery and Back Again
- •The Future Is Now
- •References
- •Interventional Procedure
- •Assessment of Flow–Volume Curve
- •Dyspnea
- •Analysis of Pressure–Pressure Curve
- •Conclusions
- •References
- •Introduction
- •Adaptations of the IP Department
- •Environmental Control
- •Personal Protective Equipment
- •Procedure Performance
- •Bronchoscopy in Intubated Patients
- •Other Procedures in IP Unit
- •References
- •Introduction
- •Safety
- •Patient Safety
- •Provider Safety
- •Patient Selection and Screening
- •Lung Cancer Diagnosis and Staging
- •Inpatients
- •COVID-19 Clearance
- •COVID Clearance: A Role for Bronchoscopy
- •Long COVID: A Role for Bronchoscopy
- •Preparing for the Next Pandemic
- •References
- •Historical Perspective
- •Indications and Contraindications
- •Evidence-Based Review
- •Summary and Recommendations
- •References
- •Introduction
- •Clinical Presentation
- •Diagnosis
- •Treatment
- •History and Historical Perspectives
- •Indications and Contraindications
- •Benign and Malignant Tumors
- •Tumors with Uncertain Prognosis
- •Application of the Technique
- •Evidence Based Review
- •Summary and Recommendations
- •References
- •12: Cryotherapy and Cryospray
- •Introduction
- •Historical Perspective
- •Equipment
- •Cryoadhesion
- •Indications
- •Cryorecanalization
- •Cryoadhesion and Foreign Body Removal
- •Cryoadhesion and Mucus Plugs/Blood Clot Retrieval
- •Endobronchial Cryobiopsy
- •Transbronchial Cryobiopsy for Lung Cancer
- •Safety Concerns and Contraindications
- •Cryoablation
- •Indications
- •Evidence
- •Safety Concerns and Contraindications
- •Cryospray
- •Indications
- •Evidence
- •Safety Concerns and Contraindications
- •Advantages of Cryotherapy
- •Limitations
- •Future Research Directions
- •References
- •13: Brachytherapy
- •History and Historical Perspective
- •Indications and Contraindications
- •Application of the Technique
- •Evidence-Based Review
- •Adjuvant Treatment
- •Palliative Treatment
- •Complications
- •Summary and Recommendations
- •References
- •14: Photodynamic Therapy
- •Introduction
- •Photosensitizers
- •First-Generation Photosensitizers
- •M-Tetrahidroxofenil Cloro (mTHPC) (Foscan®)
- •PDT Reaction
- •Tumor Damage Process
- •Procedure
- •Indications
- •Curative PDT Indications
- •Palliative PDT Indications
- •Contraindications
- •Rationale for Use in Early-Stage Lung Cancer
- •Rationale
- •PDT in Combination with Other Techniques for Advanced-Stage Non-small Cell Lung Cancer
- •Commentary
- •Complementary Endoscopic Methods for PDT Applications
- •New Perspectives
- •Other PDT Applications
- •Conclusions
- •References
- •15: Benign Airways Stenosis
- •Etiology
- •Congenital Tracheal Stenosis
- •Iatrogenic
- •Infectious
- •Idiopathic Tracheal Stenosis
- •Distal Bronchial Stenosis
- •Diagnosis Methods
- •Patient History
- •Imaging Techniques
- •Bronchoscopy
- •Pulmonary Function Test
- •Treatment
- •Endoscopic Treatment
- •Dilatation
- •Laser Therapy
- •Stents
- •How to Proceed
- •Stent Placement
- •Placing a Montgomery T Tube
- •The Rule of Twos for Benign Tracheal Stenosis (Fig. 15.23)
- •Surgery
- •Summary and Recommendations
- •References
- •16: Endobronchial Prostheses
- •Introduction
- •Indications
- •Extrinsic Compression
- •Intraluminal Obstruction
- •Stump Fistulas
- •Esophago-respiratory Fistulas (ERF)
- •Expiratory Central Airway Collapse
- •Physiologic Rationale for Airway Stent Insertion
- •Stent Selection Criteria
- •Stent-Related Complications
- •Granulation Tissue
- •Stent Fracture
- •Migration
- •Contraindications
- •Follow-Up and Patient Education
- •References
- •Introduction
- •Overdiagnosis
- •False Positives
- •Radiation
- •Risk of Complications
- •Lung Cancer Screening Around the World
- •Incidental Lung Nodules
- •Management of Lung Nodules
- •References
- •Introduction
- •Minimally Invasive Procedures
- •Mediastinoscopy
- •CT-Guided Transthoracic Biopsy
- •Fluoroscopy-Guided Transthoracic Biopsies
- •US-Guided Transthoracic Biopsy
- •Thoracentesis and Pleural Biopsy
- •Thoracentesis
- •Pleural Biopsy
- •Surgical or Medical Thoracoscopy
- •Image-Guided Pleural Biopsy
- •Closed Pleural Biopsy
- •Image-Guided Biopsies for Extrathoracic Metastases
- •Tissue Acquisition, Handling and Processing
- •Implications of Tissue Acquisition
- •Guideline Recommendations for Tissue Acquisition in Mediastinal Staging
- •Methods to Overcome Challenges in Tissue Acquisition and Genotyping
- •Rapid on-Site Evaluation (ROSE)
- •Sensitive Genotyping Assays
- •Liquid Biopsy
- •Summary, Recommendations and Highlights
- •References
- •History
- •Data Source and Methodology
- •Tumor Size
- •Involvement of the Main Bronchus
- •Atelectasis/Pneumonitis
- •Nodal Staging
- •Proposal for the Revision of Stage Groupings
- •Small Cell Lung Cancer (SCLC)
- •Discussion
- •Methodology
- •T Descriptors
- •N Descriptors
- •M Descriptors
- •Summary
- •References
- •Introduction
- •Historical Perspective
- •Fluoroscopy
- •Radial EBUS Mini Probe (rEBUS)
- •Ultrasound Bronchoscope (EBUS)
- •Virtual Bronchoscopy
- •Trans-Parenchymal Access
- •Cone Beam CT (CBCT)
- •Lung Vision
- •Sampling Instruments
- •Conclusions
- •References
- •History and Historical Perspective
- •Narrow Band Imaging (NBI)
- •Dual Red Imaging (DRI)
- •Endobronchial Ultrasound (EBUS)
- •Optical Coherence Tomography (OCT)
- •Indications and Contraindications
- •Confocal Laser Endomicroscopy and Endocytoscopy
- •Raman Spectrophotometry
- •Application of the Technique
- •Supplemental Technology for Diagnostic Bronchoscopy
- •Evidence-Based Review
- •Summary and Recommendations, Highlight of the Developments During the Last Three Years (2013 on)
- •References
- •Introduction
- •History and Historical Perspective
- •Endoscopic AF-OCT System
- •Preclinical Studies
- •Clinical Studies
- •Lung Cancer
- •Asthma
- •Airway and Lumen Calibration
- •Obstructive Sleep Apnea
- •Future Applications
- •Summary
- •References
- •23: Endobronchial Ultrasound
- •History and Historical Perspective
- •Equipment
- •Technique
- •Indication, Application, and Evidence
- •Convex Probe Ultrasound
- •Equipment
- •Technique
- •Indication, Application, and Evidence
- •CP-EBUS for Malignant Mediastinal or Hilar Adenopathy
- •CP-EBUS for the Staging of Non-small Cell Lung Cancer
- •CP-EBUS for Restaging NSCLC After Neoadjuvant Chemotherapy
- •Complications
- •Summary
- •References
- •Introduction
- •What Is Electromagnetic Navigation?
- •SuperDimension Navigation System (EMN-SD)
- •Computerized Tomography
- •Computer Interphase
- •The Edge Catheter: Extended Working Channel (EWC)
- •Procedural Steps
- •Planning
- •Detecting Anatomical Landmarks
- •Pathway Planning
- •Saving the Plan and Exiting
- •Registration
- •Real-Time Navigation
- •SPiN System Veran Medical Technologies (EMN-VM)
- •Procedure
- •Planning
- •Navigation
- •Biopsy
- •Complications
- •Limitations
- •Summary
- •References
- •Introduction
- •Image Acquisition
- •Hardware
- •Practical Considerations
- •Radiation Dose
- •Mobile CT Studies
- •Future Directions
- •Conclusion
- •References
- •26: Robotic Assisted Bronchoscopy
- •Historical Perspective
- •Evidence-Based Review
- •Diagnostic Yield
- •Monarch RAB
- •Ion Endoluminal Robotic System
- •Summary
- •References
- •History and Historical Perspective
- •Indications and Contraindications
- •General
- •Application of the Technique
- •Preoperative Care
- •Patient’s Position and Operative Field
- •Incision and Initial Dissection
- •Palpation
- •Biopsy
- •Control of Haemostasis and Closure
- •Postoperative Care
- •Complications
- •Technical Variants
- •Extended Cervical Mediastinoscopy
- •Mediastinoscopic Biopsy of Scalene Lymph Nodes
- •Inferior Mediastinoscopy
- •Mediastino-Thoracoscopy
- •Video-Assisted Mediastinoscopic Lymphadenectomy
- •Transcervical Extended Mediastinal Lymphadenectomy
- •Evidence-Based Review
- •Summary and Recommendations
- •References
- •Introduction
- •Case 1
- •Adrenal and Hepatic Metastases
- •Brain
- •Bone
- •Case 1 Continued
- •Biomarkers
- •Case 1 Concluded
- •Case 2
- •Chest X-Ray
- •Computerized Tomography
- •Positive Emission Tomography
- •Magnetic Resonance Imaging
- •Endobronchial Ultrasound with Transbronchial Needle Aspiration
- •Transthoracic Needle Aspiration
- •Transbronchial Needle Aspiration
- •Endoscopic Ultrasound with Needle Aspiration
- •Combined EUS-FNA and EBUS-TBNA
- •Case 2 Concluded
- •Case 3
- •Standard Cervical Mediastinoscopy
- •Extended Cervical Mediastinoscopy
- •Anterior Mediastinoscopy
- •Video-Assisted Thoracic Surgery
- •Case 3 Concluded
- •Case 4
- •Summary
- •References
- •29: Pleural Anatomy
- •Pleural Embryonic Development
- •Pleural Histology
- •Cytological Characteristics
- •Mesothelial Cells Functions
- •Pleural Space Defense Mechanism
- •Pleura Macroscopic Anatomy
- •Visceral Pleura (Pleura Visceralis or Pulmonalis)
- •Parietal Pleura (Pleura Parietalis)
- •Costal Parietal Pleura (Costalis)
- •Pleural Cavity (Cavitas Thoracis)
- •Pleural Apex or Superior Pleural Sinus [12–15]
- •Anterior Costal-Phrenic Sinus or Cardio-Phrenic Sinus
- •Posterior Costal-Phrenic Sinus
- •Cost-Diaphragmatic Sinus or Lateral Cost-Phrenic Sinus
- •Fissures18
- •Pleural Vascularization
- •Parietal Pleura Lymphatic Drainage
- •Visceral Pleura Lymphatic Drainage
- •Pleural Innervation
- •References
- •30: Chest Ultrasound
- •Introduction
- •The Technique
- •The Normal Thorax
- •Chest Wall Pathology
- •Pleural Pathology
- •Pleural Thickening
- •Pneumothorax
- •Pulmonary Pathology
- •Extrathoracic Lymph Nodes
- •COVID and Chest Ultrasound
- •Conclusions
- •References
- •Introduction
- •History of Chest Tubes
- •Overview of Chest Tubes
- •Contraindications for Chest Tube Placement
- •Chest Tube Procedural Technique
- •Special Considerations
- •Pneumothorax
- •Empyema
- •Hemothorax
- •Chest Tube Size Considerations
- •Pleural Drainage Systems
- •History of and Introduction to Indwelling Pleural Catheters
- •Indications and Contraindications for IPC Placement
- •Special Considerations
- •Non-expandable Lung
- •Chylothorax
- •Pleurodesis
- •Follow-Up and IPC Removal
- •IPC-Related Complications and Management
- •Competency and Training
- •Summary
- •References
- •32: Empyema Thoracis
- •Historical Perspectives
- •Incidence
- •Epidemiology
- •Pathogenesis
- •Clinical Presentation
- •Radiologic Evaluation
- •Biochemical Analysis
- •Microbiology
- •Non-operative Management
- •Prognostication
- •Surgical Management
- •Survivorship
- •Summary and Recommendations
- •References
- •Evaluation
- •Initial Intervention
- •Pleural Interventions for Recurrent Symptomatic MPE
- •Especial Circumstances
- •References
- •34: Medical Thoracoscopy
- •Introduction
- •Diagnostic Indications for Medical Thoracoscopy
- •Lung Cancer
- •Mesothelioma
- •Other Tumors
- •Tuberculosis
- •Therapeutic Indications
- •Pleurodesis of Pneumothorax
- •Thoracoscopic Drainage
- •Drug Delivery
- •Procedural Safety and Contraindications
- •Equipment
- •Procedure
- •Pre-procedural Preparations and Considerations
- •Procedural Technique [32]
- •Medical Thoracoscopy Versus VATS
- •Conclusion
- •References
- •Historical Perspective
- •Indications and Contraindications
- •Evidence-Based Review
- •Endobronchial Valves
- •Airway Bypass Tracts
- •Coils
- •Other Methods of ELVR
- •Summary and Recommendations
- •References
- •36: Bronchial Thermoplasty
- •Introduction
- •Mechanism of Action
- •Trials
- •Long Term: Ten-Year Study
- •Patient Selection
- •Bronchial Thermoplasty Procedure
- •Equipment
- •Pre-procedure
- •Bronchoscopy
- •Post-procedure
- •Conclusion
- •References
- •Introduction
- •Bronchoalveolar Lavage (BAL)
- •Technical Aspects of BAL Procedure
- •ILD Cell Patterns and Diagnosis from BAL
- •Technical Advises for Conventional TLB and TLB-C in ILD
- •Future Directions
- •References
- •Introduction
- •The Pediatric Airway
- •Advanced Diagnostic Procedures
- •Endobronchial Ultrasound
- •Virtual Navigational Bronchoscopy
- •Cryobiopsy
- •Therapeutic Procedures
- •Dilation Procedures
- •Thermal Techniques
- •Mechanical Debridement
- •Endobronchial Airway Stents
- •Metallic Stents
- •Silastic Stents
- •Novel Stents
- •Endobronchial Valves
- •Bronchial Thermoplasty
- •Discussion
- •References
- •Introduction
- •Etiology
- •Congenital ADF
- •Malignant ADF
- •Cancer Treatment-Related ADF
- •Benign ADF
- •Iatrogenic ADF
- •Diagnosis
- •Treatment Options
- •Endoscopic Techniques
- •Stents
- •Clinical Results
- •Stent Complications
- •Other Available Stents
- •Other Endoscopic Methods
- •References
- •Introduction
- •Anatomy and Physiology of Swallowing
- •Functional Physiology of Swallowing
- •Epidemiology and Risk Factors
- •Types of Foreign Bodies
- •Organic
- •Inorganic
- •Mineral
- •Miscellaneous
- •Clinical Presentation
- •Acute FB
- •Retained FB
- •Radiologic Findings
- •Bronchoscopy
- •Airway Management
- •Rigid Vs. Flexible Bronchoscopy
- •Retrieval Procedure
- •Instruments
- •Grasping Forceps
- •Baskets
- •Balloons
- •Suction Instruments
- •Ablative Therapies
- •Cryotherapy
- •Laser Therapy
- •Electrocautery and APC
- •Surgical Management
- •Complications
- •Bleeding and Hemoptysis
- •Distal Airway Impaction
- •Iron Pill Aspiration
- •Follow-Up and Sequelae
- •Conclusion
- •References
- •Vascular Origin of Hemoptysis
- •History and Historical Perspective
- •Diagnostic Bronchoscopy
- •Therapeutic Bronchoscopy
- •General Measures
- •Therapeutic Bronchoscopy
- •Evidence-Based Review
- •Summary
- •Recommendations
- •References
- •History
- •“The Glottiscope” (1807)
- •“The Esophagoscope” (1895)
- •The Rigid Bronchoscope (1897–)
- •The Flexible Bronchoscope (1968–)
- •Transbronchial Lung Biopsy (1972) (Fig. 42.7)
- •Laser Therapy (1981–)
- •Endobronchial Stents (1990–)
- •Electromagnetic Navigation (2003–)
- •Bronchial Thermoplasty (2006–)
- •Endobronchial Microwave Therapy (2004–)
- •American Association for Bronchology and Interventional Pulmonology (AABIP) and Journal of Bronchology and Interventional Pulmonology (JOBIP) (1992–)
- •References
- •Index

42 |
M. Díez Ferrer and A. Rosell |
|
|
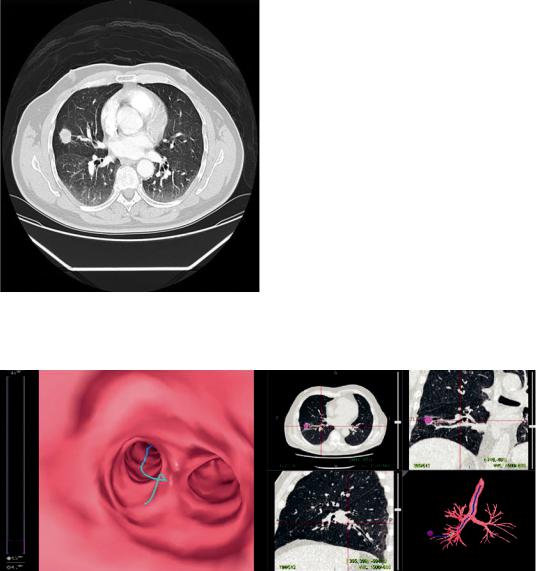
Fig. 3.4 Two bronchoscopists and one trained nurse performing ultrathin bronchoscopy with virtual bronchoscopic navigation (LungPoint®) in the endoscopy suite. Note that fuoroscopy is also used
Optional equipment:
•\ Cone-beam CT to corroborate the position of the ultrathin bronchoscope and the sampling instrument relative to the lesion.
•\ Virtual bronchoscopy, virtual bronchoscopic navigation, or electromagnetic navigation to assist procedure planning and guiding of the ultrathin bronchoscope to the peripheral pulmonary lesion.
In Fig. 3.4, ultrathin bronchoscopy with virtual bronchoscopic navigation is performed under general anesthesia in the endoscopy suite.
choscope and to assist sampling, although CT or cone-beam CT can also be used to corroborate the position of the ultrathin bronchoscope and the sampling instrument relative to the lesion. Sampling is performed with instruments of limited size that can be passed through the working channel of the ultrathin bronchoscope.
To develop all the aforementioned aspects and to provide an integrated understanding of the technologies that can be coupled with ultrathin bronchoscopy, we have structured ultrathin bronchoscopy in the following steps: procedure planning, target approximation, position veri cation, and sampling.
Procedure Description |
Procedure Planning |
In general terms, the procedure starts by conducting an accurate planning of the bronchial route leading to the peripheral lesion, either through ne reading of a high-resolution chest CT or supported by a planning software. During the procedure of ultrathin bronchoscopy, target approximation can be accomplished after memorization of the planned bronchial route or assisted by navigation software. Fluoroscopy is usually used to track the position of the ultrathin bron-
First thing to consider when planning the procedure on a CT image is the presence of a bronchus or artery afferent or, within the peripheral lesion, the so called bronchus sign and artery sign. When present, the diagnostic yield of the procedure is signi cantly higher [10–12]. Examples of bronchus and artery signs are shown in Fig. 3.5.
If the slice thickness of the CT is suf cient to allow identi cation of small bronchi and if a bronchus leading to the lesions is present, then it
Данная книга находится в списке для перевода на русский язык сайта https://meduniver.com/
3 Ultrathin Bronchoscopy: Indications and Technique |
43 |
|
|
will be feasible to reconstruct a three-dimensional bronchial route to the peripheral nodule. With this information alone, highly trained bronchoscopists have the ability to reconstruct the bronchial route from the CT and mentally reproduce the route during the procedure. Fortunately, complementary technologies have been developed to assist procedure planning. The mainstay technology for procedure planning is virtual bronchoscopy. Dedicated software is used for multiplanar
Fig. 3.5 Chest CT showing both a bronchus and artery leading to a PPL (bronchus and artery signs, respectively)
reconstruction of CT images and segmentation of the airways. After manual identi cation of the nodule in the CT, the bronchial route to the nodule can be followed through the inner lumen of the segmented airways. This route can be memorized by the bronchoscopist to be reproduced in the bronchoscopy suite. Otherwise, a virtual bronchoscopic navigation platform can be used to perform virtual bronchoscopy in the endoscopy suite and match virtual and endoscopic images during the procedure to facilitate orientation. A screenshot of a virtual bronchoscopy is shown in Fig. 3.6.
Target Approximation
In order to guarantee patient stillness during the procedure, the authors of the present text prefer performing ultrathin bronchoscopy under general anesthesia and laryngeal mask or endotracheal intubation. This facilitates bronchoscope manipulation in the smaller subsegmental bronchi, allows application of short controlled apneas to gain greater operator control during sampling, and may also avoid accidental damaging of theber bronchoscope due to abrupt patient movements. It has to be pointed out that, in some cases, cutting some centimeters of the proximal end of the orotracheal tube may be necessary to warrant full insertion of the 600 mm working length of the ultrathin bronchoscope and avoid falling
Fig. 3.6 Procedure plani cation with a virtual bronchoscopy navigation system (LungPoint®). This system allows matching the virtual bronchoscopy seen in the Figure with the endoscopic images during the procedure
44 |
M. Díez Ferrer and A. Rosell |
|
|
short to the lung periphery, especially in relatively tall patients. However, general anesthesia is not mandatory and moderate sedation is preferred in many centers.
As previously mentioned, target approximation can be accomplished after memorization of the planned bronchial route or assisted by virtual bronchoscopic navigation software. This software allows matching virtual and endoscopic images during the procedure to guide the ultrathin bronchoscope through every bifurcation leading to the afferent bronchus. In either case, fuoroscopy is usually used to track the real-time position of the ultrathin bronchoscope.
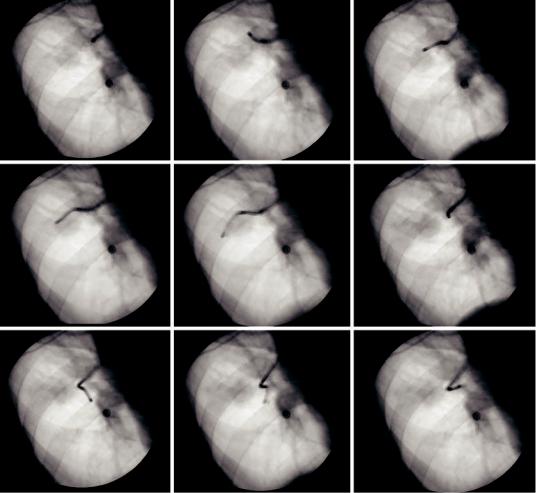
Fluoroscopy was the rst imaging technique used for guiding the ultrathin bronchoscope to the nodule [1]. Biplanar fuoroscopy is desirable but, when not accessible, the C-arm must be rotated adequately. Although it is not a guidance tool per se, it can be useful to con rm the position and direction of the bronchoscope throughout the procedure and relative to the peripheral lesion, as long as the lesion is fuoroscopically visible (see Fig. 3.7). Unfortunately, peripheral pulmonary nodules are not always visible with fuoroscopy. In one study, the authors reported that from a population of 1369 individuals at high risk for lung cancer, 15 small peripheral lung
a |
b |
c |
d |
e |
f |
g |
h |
i |
Fig. 3.7 Fluoroscopy Fluoroscopy can be used to track down the path leading to the peripheral pulmonary lesion. To assure that the right direction is followed, fuoroscopy
is performed in every bifurcation (a–i). Whenever misdirected, the bronchoscope is pulled backward to the previous bifurcation and another bronchus followed
Данная книга находится в списке для перевода на русский язык сайта https://meduniver.com/
3 Ultrathin Bronchoscopy: Indications and Technique |
45 |
|
|
cancers were detected with low-dose CT. Of these, 73% had negative chest radiography [13]. Because CT allows for nodule detection independent of size, localization, and characteristics of the PPL, it has also been used for verifying the position of the instrument when exploring the peripheral airways [14].
Virtual bronchoscopic navigation can also be used to assist in lesion approximation. When using virtual bronchoscopic navigation systems, a trained bronchoscopist is needed to perform the virtual bronchoscopy through the previously selected path. The assistant bronchoscopist will guide the operator through the airways and will indicate the right direction in each encountered bifurcation. To date, there is only one large randomized trial comparing ultrathin bronchoscopy with and without use of virtual bronchoscopic navigation. This study by Asano et al. showed no signi cant differences in diagnostic yield on both groups (67.1% vs. 59.9%; p = 0.173) in 350 patients with peripheral nodules ≤3 cm. However, subgroup analysis of these data showed that the navigation system could be helpful for achieving nodules located in the peripheral third of the lung, those invisible in the postero-ante- rior radiographs and when located in the upper right lobe. Fluoroscopy was used in both groups to ensure location of the ultrathin bronchoscope and sampling of the desired location [15]. In a later study, we compared ultrathin bronchoscopy with and without virtual bronchoscopic navigation and evaluated the infuence of segmentation on diagnostic yield [16]. We compared 55 cases of virtual bronchoscopic navigationguided ultrathin bronchoscopy to 110 unguided controls. Although the diagnostic yield did not differ between both arms (47% and 40%, respectively; p = 0.354), an 85% diagnostic yield was observed when segmentation was optimal and the peripheral nodule was endobronchial, compared to a 30% diagnostic yield when the segmentation was suboptimal and a 20% diagnostic yield when segmentation was optimal but the lesion extrabronchial. In fact, the position of the lesion relative to the bronchus, that is, if the lesion is endoor extrabronchial, will determine the diagnostic yield of the procedure. This point is fur-
ther commented in the next section on position veri cation.
During target approximation with an ultrathin bronchoscope, several considerations should be made. First of all is the limited suction capability of the ultrathin bronchoscope due to the small working channel. Therefore, if abundant or thick secretions are present, it might be recommended that bronchial hygiene with a conventional bronchoscope is performed either prior to starting or during the procedure. Also, angulation of the tip of the ultrathin bronchoscope can be challenging in the upper lobes. Sometimes it might be simply impossible to overcome some anatomical angulations with the ultrathin bronchoscope. Leaving the biopsy forceps inside the working channel may provide greater stiffness to the bronchoscope in some cases. Finally, another disadvantage of ultrathin compared to conventional bronchoscopes is the quality of the endoscopic vision, not only in regard to technical manufacturing details but also to bronchial anatomy in the lung periphery. Particularly, a greater collapsibility is found in the periphery due to progressive loss of stiffness in the intrapulmonary airways. To overcome bronchial collapsibility and improve endoscopic vision in the peripheral airways, it is recommended that secretions are not aspirated and saline is continuously instilled instead. In our institution, a 50 mL syringe with room-temperature saline is connected to the working channel of the ultrathin bronchoscope. The assistant instills saline as requested, thus facilitating bypassing of secretions and bronchial lumen widening. A view of ultrathin bronchoscopy in peripheral airways under saline infusion is shown in Fig. 3.8.
Position Verifcation
Once the peripheral pulmonary lesion is approximated and no endobronchial abnormality is visualized, then two issues might have occurred: either approximation to the lesion has not been accurate enough, or the lesion is extrabronchial. At this point, fuoroscopy, CT, or cone-beam CT can be used to verify the position of the ultrathin bronchoscope relative to the lesion. Also, a radial

46 |
M. Díez Ferrer and A. Rosell |
|
|
a
b
Fig. 3.8 Ultrathin bronchoscopy in peripheral airways: (a) 50 mL aliquot with saline connected to the working channel. (b) Views before and after saline infusion
Данная книга находится в списке для перевода на русский язык сайта https://meduniver.com/
