
Оригинал
.pdf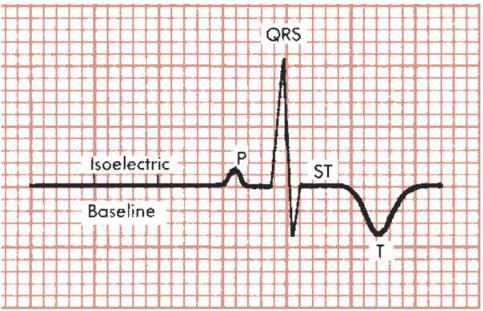
FIGURE 2-6 The P wave is positive (upward), and the T wave is negative (downward). The QRS complex is biphasic (partly positive, partly negative), and the ST segment is isoelectric (neither positive nor negative).
This chapter examines P, QRS, ST, T, and U waves in a general way. The measurements of heart rate, PR interval, QRS width, and QT interval are considered in detail, along with their normal values.
P WAVE
The P wave, which represents atrial depolarization, is a small positive (or negative) deflection before the QRS complex. (The normal values for P wave amplitude and width are described in Chapter 6.)
PR INTERVAL
The PR interval is measured from the beginning of the P wave to the beginning of the QRS complex (Fig. 2-7). The PR interval may vary slightly in different leads, and the shortest PR interval should be noted. The PR interval represents the time it takes for the stimulus to spread through the atria and pass through the AV junction. (This physiologic delay allows the ventricles to fill fully with blood before ventricular depolarization occurs.) In adults the normal PR interval is between 0.12 and 0.2 second (three to five small box sides). When conduction through the AV junction is impaired, the PR interval may become prolonged. Prolongation of the PR interval above 0.2 second is called first-degree heart block (see Chapter 17).
11

FIGURE 2-7 Measurement of the PR interval (see text).
QRS COMPLEX
One of the most confusing aspects of electrocardiography for the beginning student is the nomenclature of the QRS complex. As noted previously, the QRS complex represents the spread of a stimulus through the ventricles. However, not every QRS complex contains a Q wave, an R wave, and an S wave—hence the confusion. The bothersome but unavoidable nomenclature becomes understandable if you remember several basic features of the QRS complex (see Fig. 2-8): When the initial deflection of the QRS complex is negative (below the baseline), it is called a Q wave; the first positive deflection in the QRS complex is called an R wave; a negative deflection following the R wave is called an S wave. Thus the following QRS complex contains a Q wave, an R wave, and an S wave:
FIGURE 2-8 QRS nomenclature (see text).
12

In contrast, the following complex does not contain three waves:
If, as shown, the entire QRS complex is positive, it is simply called an R wave.
If the entire complex is negative, however, it is termed a QS wave (not just a Q wave, as might be expected).
Occasionally, the QRS complex contains more than two or three deflections. In such cases, the extra waves are called R′ (R prime) waves if they are positive and S′
(S prime) waves if they are negative.
Figure 2-8 shows the various possible QRS complexes and the nomenclature of the respective waves. Notice that capital letters (QRS) are used to designate waves of relatively large amplitude and small letters (qrs) label relatively small waves.
The QRS nomenclature is confusing at first, but it allows you to describe any QRS complex over the phone and to evoke in the mind of the trained listener an exact mental picture of the complex named. For example, in describing an ECG you might say that lead V1 showed an rS complex (“small r, capital S”):
You might also describe a QS (“capital Q, capital S”) in lead aVF:
13

QRS WIDTH (INTERVAL)
The QRS width, or interval, represents the time required for a stimulus to spread through the ventricles (ventricular depolarization) and is normally 0.1 second or less (Fig. 2-9). If the spread of a stimulus through the ventricles is slowed, for example, by a block in one of the bundle branches, the QRS width is prolonged. (The full differential diagnosis of a wide QRS complex is discussed in Chapters 12 and 24.)
FIGURE 2-9 Measurement of the QRS width (interval) (see text).
ST SEGMENT
The ST segment is that portion of the ECG cycle from the end of the QRS complex to the beginning of the T wave (Fig. 2-10). It represents the beginning of ventricular repolarization. The normal ST segment is usually isoelectric (i.e., flat on the baseline, neither positive nor negative), but it may be slightly elevated or depressed normally (usually by less than 1 mm). Some pathologic conditions such as myocardial infarction (MI) produce characteristic abnormal deviations of the ST segment. The very beginning of the ST segment (actually the junction between the
14

end of the QRS complex and the beginning of the ST segment) is sometimes called the J point. Figure 2-10 shows the J point and the normal shapes of the ST segment. Figure 2-11 compares a normal isoelectric ST segment with abnormal ST segment elevation and depression.
FIGURE 2-10 Characteristics of the normal ST segment and T wave. The junction (J) is the beginning of the ST segment.
FIGURE 2-11 ST segments. A, Normal. B, Abnormal elevation. C, Abnormal depression.
15

T WAVE
The T wave represents part of ventricular repolarization. A normal T wave has an asymmetric shape; that is, its peak is closer to the end of the wave than to the beginning (see Fig. 2-10). When the T wave is positive, it normally rises slowly and then abruptly returns to the baseline.[*] When it is negative, it descends slowly and abruptly rises to the baseline. The asymmetry of the normal T wave contrasts with the symmetry of T waves in certain abnormal conditions such as myocardial infarction (see Chapters 8 and 9) and a high serum potassium level (see Chapter 10).
QT INTERVAL
The QT interval is measured from the beginning of the QRS complex to the end of the T wave (Fig. 2-12). It primarily represents the return of stimulated ventricles to their resting state (ventricular repolarization). The normal values for the QT interval depend on the heart rate. As the heart rate increases (the RR interval shortens),[†] the QT normally shortens; as the heart rate decreases (the RR interval lengthens), the QT interval lengthens.
FIGURE 2-12 Measurement of the QT interval. The RR interval is the interval between two consecutive QRS complexes (see text).
The QT should be measured in the ECG lead (see Chapter 3) that shows the longest intervals. You can measure several intervals in that lead and use the average value. When the QT interval is long, it is often difficult to measure because the end of the T wave may merge imperceptibly with the U wave. As a result, you may be measuring the QU interval rather than the QT interval.
Table 2-1 shows approximate upper normal limits for the QT interval with different heart rates. Unfortunately, there is no simple rule for determining the normal limits of the QT interval. As a result of this problem, another index of the QT was
16

devised. It is the rate-corrected QT or QTc. The rate-corrected QT can be obtained by dividing the actual QT by the square root of the RR interval (both measured in
seconds):
TABLE 2-1 -- QT Interval
Upper Limits of Normal (Estimated)
Measured RR interval (sec) |
Heart rate (per min) |
QT interval upper normal limits (sec) |
|
|
|
1.50 |
40 |
0.50 |
|
|
|
1.20 |
50 |
0.48 |
|
|
|
1.00 |
60 |
0.43 |
|
|
|
0.86 |
70 |
0.40 |
|
|
|
0.80 |
75 |
0.39 |
|
|
|
0.75 |
80 |
0.37 |
|
|
|
0.67 |
90 |
0.35 |
|
|
|
0.60 |
100 |
0.34 |
|
|
|
0.50 |
120 |
0.31 |
|
|
|
0.40 |
150 |
0.27 |
|
|
|
Normally, the QTc is less than or equal to about 0.44 second.
As a general rule: At heart rates of 80/min or less, a measured QT interval of more than half the RR interval is always prolonged. It is also important to note, however, that at heart rates below 80/min, the QT may be less than half the RR and still be significantly prolonged, and at heart rates above 80/min, a QT more than half the RR is not necessarily prolonged (see Table 2-1).
A number of factors can abnormally prolong the QT interval (Fig. 2-13). For example, this interval can be prolonged by certain drugs used to treat cardiac arrhythmias (e.g., amiodarone, disopyramide, dofetilide, ibutilide, procainamide, quinidine, and sotalol), as well as a large number of other types of agents (tricyclic antidepressants, phenothiazines, pentamidine, and so forth). Specific electrolyte disturbances (low potassium, magnesium, or calcium levels) are important causes of
17

QT prolongation. Hypothermia also prolongs the QT interval by slowing the repolarization of myocardial cells. The QT interval may be prolonged with myocardial ischemia and infarction (especially during the evolving phase) and with subarachnoid hemorrhage. QT prolongation may predispose patients to potentially lethal ventricular arrhythmias. (See the discussion of torsades de pointes in Chapter 16.) The differential diagnosis of a long QT is summarized in Chapter 24.
FIGURE 2-13 Abnormal QT interval prolongation in a patient taking quinidine. The QT interval (0.6 sec) is markedly prolonged for the heart rate (65 beats/min) (see Table 2-1). The rate-corrected QT interval (normally 0.44 sec or less) is also prolonged (0.63 sec).[*] Prolonged ventricular repolarization may predispose patients to develop torsades de pointes, a life-threatening ventricular arrhythmia (see Chapter 16).
The QT interval may be shortened by digitalis in therapeutic doses or by hypercalcemia, for example. Because the lower limits of normal for the QT interval have not been well defined, only the upper limits are given in Table 2-1.
U WAVE
The U wave is a small, rounded deflection sometimes seen after the T wave (see Fig. 2-2). As noted previously, its exact significance is not known. Functionally, U waves represent the last phase of ventricular repolarization. Prominent U waves are
characteristic of hypokalemia (see Chapter 10). Very prominent U waves may also be 18

seen in other settings, for example, in patients taking drugs such as sotalol or one of the phenothiazines or sometimes after patients have had a cerebrovascular accident. The appearance of very prominent U waves in such settings, with or without actual QT prolongation, may also predispose patients to ventricular arrhythmias (see Chapter 16).
Normally, the direction of the U wave is the same as that of the T wave. Negative U waves sometimes appear with positive T waves. This abnormal finding has been noted in left ventricular hypertrophy and myocardial ischemia.
CALCULATION OF HEART RATE
Two simple methods can be used to measure the heart rate (number of heartbeats per minute) from the ECG: box counting method and QRS counting method.
BOX COUNTING METHOD
The easier way, when the heart rate is regular, is to count the number of large (0.2-sec) boxes between two successive QRS complexes and divide a constant (300) by this. (The number of large time boxes is divided into 300 because 300 × 0.2 = 60 and the heart rate is calculated in beats per minute or 60 seconds.)
For example, in Figure 2-14, the heart rate is 75 beats/min, since four large time boxes are counted between successive R waves (300 ÷ 4 = 75). Similarly, if two large time boxes are counted between successive R waves, the heart rate is 150 beats/min. With five intervening large time boxes, the heart rate is 60 beats/min.
FIGURE 2-14 Heart rate (beats per minute) can be measured by counting the number of large (0.2-sec) time boxes between two successive QRS complexes and
19

dividing 300 by this number. In this example, the heart rate is calculated as 300 ÷ 4
= 75 beats/min.
When the heart rate is fast or must be measured very accurately from the ECG, you can modify the approach as follows: Count the number of small (0.04-sec) boxes between successive R waves and divide a constant (1500) by this number. In Figure 2-14, 20 small time boxes are counted between QRS complexes. Therefore the heart rate is 1500 ÷ 20 = 75 beats/min. (The constant 1500 is used because 1500 × 0.04 =
60 and the heart rate is being calculated in beats per 60 seconds.) QRS COUNTING METHOD
If the heart rate is irregular, the first method will not be accurate because the intervals between QRS complexes vary from beat to beat. In such cases you can determine an average rate simply by counting the number of QRS complexes in some convenient time interval (e.g., every 6 seconds or every 10 seconds) and multiplying this number by the appropriate factor to obtain the rate in beats per 60 seconds.
Counting the number of QRS complexes in 6-second intervals (and then multiplying this number by 10; Fig. 2-15) can be easily done in most acute settings because the top of the ECG paper used in bedside cardiac monitors and telemetry units is generally scored with vertical marks every 3 seconds[*] (see Fig. 2-14).
For conventional, full 12-lead ECG recordings, the rhythm strip at the bottom of the chart generally displays 10 consecutive seconds of data, so the number of QRS complexes in this entire interval can be multiplied by 10 to obtain the heart rate.
20
