
- •Preface
- •Contents
- •1 Elements of the Nervous System
- •2 Somatosensory System
- •3 Motor System
- •4 Brainstem
- •5 Cerebellum
- •6 Diencephalon and Autonomic Nervous System
- •7 Limbic System
- •8 Basal Ganglia
- •9 Cerebrum
- •10 Coverings of the Brain and Spinal Cord; Cerebrospinal Fluid and Ventricular System
- •Further Reading
- •Index
- •Abbreviations
- •1 Elements of the Nervous System
- •Elements of the Nervous System
- •Information Flow in the Nervous System
- •Synapses
- •Neurotransmitters and Receptors
- •Functional Groups of Neurons
- •Glial Cells
- •Development of the Nervous System
- •2 Somatosensory System
- •Peripheral Nerve, Dorsal Root Ganglion, Posterior Root
- •Peripheral Regulatory Circuits
- •Central Components of the Somatosensory System
- •Posterior and Anterior Spinocerebellar Tracts
- •Posterior Columns
- •Anterior Spinothalamic Tract
- •Lateral Spinothalamic Tract
- •Other Afferent Tracts of the Spinal Cord
- •Central Processing of Somatosensory Information
- •Somatosensory Deficits due to Lesions at Specific Sites along the Somatosensory Pathways
- •3 Motor System
- •Central Components of the Motor System and Clinical Syndromes of Lesions Affecting Them
- •Motor Cortical Areas
- •Corticospinal Tract (Pyramidal Tract)
- •Corticonuclear (Corticobulbar) Tract
- •Other Central Components of the Motor System
- •Lesions of Central Motor Pathways
- •Peripheral Components of the Motor System and Clinical Syndromes of Lesions Affecting Them
- •Clinical Syndromes of Motor Unit Lesions
- •Complex Clinical Syndromes due to Lesions of Specific Components of the Nervous System
- •Spinal Cord Syndromes
- •Vascular Spinal Cord Syndromes
- •Nerve Root Syndromes (Radicular Syndromes)
- •Plexus Syndromes
- •Peripheral Nerve Syndromes
- •Syndromes of the Neuromuscular Junction and Muscle
- •4 Brainstem
- •Surface Anatomy of the Brainstem
- •Medulla
- •Pons
- •Midbrain
- •Olfactory System (CN I)
- •Visual System (CN II)
- •Eye Movements (CN III, IV, and VI)
- •Trigeminal Nerve (CN V)
- •Facial Nerve (CN VII) and Nervus Intermedius
- •Vagal System (CN IX, X, and the Cranial Portion of XI)
- •Hypoglossal Nerve (CN XII)
- •Topographical Anatomy of the Brainstem
- •Internal Structure of the Brainstem
- •5 Cerebellum
- •Surface Anatomy
- •Internal Structure
- •Cerebellar Cortex
- •Cerebellar Nuclei
- •Connections of the Cerebellum with Other Parts of the Nervous System
- •Cerebellar Function and Cerebellar Syndromes
- •Vestibulocerebellum
- •Spinocerebellum
- •Cerebrocerebellum
- •Cerebellar Tumors
- •6 Diencephalon and Autonomic Nervous System
- •Location and Components of the Diencephalon
- •Functions of the Thalamus
- •Syndromes of Thalamic Lesions
- •Thalamic Vascular Syndromes
- •Epithalamus
- •Subthalamus
- •Hypothalamic Nuclei
- •Afferent and Efferent Projections of the Hypothalamus
- •Functions of the Hypothalamus
- •Sympathetic Nervous System
- •Parasympathetic Nervous System
- •Visceral and Referred Pain
- •7 Limbic System
- •Anatomical Overview
- •Internal and External Connections
- •Microanatomy of the Hippocampal Formation
- •Amygdala
- •Functions of the Limbic System
- •Types of Memory
- •8 Basal Ganglia
- •Preliminary Remarks on Terminology
- •The Role of the Basal Ganglia in the Motor System: Phylogenetic Aspects
- •Connections of the Basal Ganglia
- •Function and Dysfunction of the Basal Ganglia
- •Clinical Syndromes of Basal Ganglia Lesions
- •9 Cerebrum
- •Development
- •Gross Anatomy and Subdivision of the Cerebrum
- •Gyri and Sulci
- •Histological Organization of the Cerebral Cortex
- •Laminar Architecture
- •Cerebral White Matter
- •Projection Fibers
- •Association Fibers
- •Commissural Fibers
- •Functional Localization in the Cerebral Cortex
- •Primary Cortical Fields
- •Association Areas
- •Frontal Lobe
- •Coverings of the Brain and Spinal Cord
- •Dura Mater
- •Arachnoid
- •Pia Mater
- •Cerebrospinal Fluid Circulation and Resorption
- •Arteries of the Anterior and Middle Cranial Fossae
- •Arteries of the Posterior Fossa
- •Collateral Circulation in the Brain
- •Dural Sinuses
- •Venous Drainage
- •Cerebral Ischemia
- •Arterial Hypoperfusion
- •Particular Cerebrovascular Syndromes
- •Impaired Venous Drainage from the Brain
- •Intracranial Hemorrhage
- •Intracerebral Hemorrhage (Nontraumatic)
- •Subarachnoid Hemorrhage
- •Subdural and Epidural Hematoma
- •Impaired Venous Drainage
- •Spinal Cord Hemorrhage and Hematoma
- •Further Reading
- •Index

4128 · 4 Brainstem
Olfactory System (CN I)
The olfactory pathway (Figs. 4.7 and 4.8) is composed of the olfactory epithelium of the nose, the fila olfactoria (olfactory nerve = CN I), the olfactory bulb and tract, and a cortical area (the paleocortex) extending from the uncus of the temporal lobe across the anterior perforated substance to the medial surface of the frontal lobe under the genu of the corpus callosum.
The olfactory epithelium occupies an area of about 2 cm2 in the roof of each nasal cavity, overlying portions of the superior nasal concha and of the nasal septum. It contains receptor cells, supportive cells, and glands (Bowman’s glands) that secrete a serous fluid, the so-called olfactory mucus, in which aromatic substances are probably dissolved. The sensory cells (olfactory cells) are bipolar cells whose peripheral processes terminate in the olfactory hairs of the olfactory epithelium.
Fila olfactoria and olfactory bulb. The central processes (neurites) of the olfactory cells coalesce into bundles containing hundreds of unmyelinated fibers surrounded by a Schwann-cell sheath. These fila olfactoria, about 20 on either side, are, in fact, the olfactory nerves (CN I is thus composed of peripheral nerve fibers, but is not a single peripheral nerve in the usual sense). They pass through small holes in the cribriform (“sievelike”) plate and enter the olfactory bulb, where they form the first synapse of the olfactory pathway. Although it is not physically located in the cerebral cortex, the olfactory bulb is actually a piece of the telencephalon. Within it, complex synapses are made onto the dendrites of mitral cells, tufted cells, and granule cells.
Olfactory pathway. The first neuron of the olfactory pathway is the bipolar olfactory cell; the second neurons are the mitral and tufted cells of the olfactory bulb. The neurites of these cells form the olfactory tract (2nd neuron), which lies adjacent to and just below the frontobasal (orbitofrontal) cortex. The olfactory tract divides into the lateral and medial olfactory striae in front of the anterior perforated substance; another portion of it terminates in the olfactory trigone, which also lies in front of the anterior perforated substance. The fibers of the lateral stria travel by way of the limen insulae to the amygdala, semilunar gyrus, and ambient gyrus (prepyriform area). This is the site of the 3rd neuron, which projects to the anterior portion of the parahippocampal gyrus (Brodmann area 28, containing the cortical projection fields and association area of the olfactory system). The fibers of the medial stria terminate on nuclei of the septal area below the genu of the corpus callosum (subcallosal area) and in front of the anterior commissure. Fibers emerging from these nuclei project, in turn, to the opposite hemisphere and to the limbic system. The olfactory path-
Baehr, Duus' Topical Diagnosis in Neurology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.

Cranial Nerves · 129 4
Longitudinal striae
Striae medullares of the thalamus
Medial olfactory stria
Subcallosal area |
|
|
Habenulo- |
|
|
|
|
||
|
|
|
interpedun- |
|
|
|
|
cular tract |
|
|
|
|
Habenular |
|
|
|
|
nucleus |
|
Olfactory bulb |
|
|
Inter- |
|
|
|
|
peduncular |
|
|
|
|
nucleus |
|
|
|
|
Medial |
|
|
|
|
forebrain |
|
|
|
|
bundle |
|
|
|
|
Tegmental |
|
|
|
|
nuclei |
|
|
|
|
Dorsal |
|
Olfactory epithelium |
Lateral |
Area 28 |
longitudinal |
|
bipolar olfactory cells |
fasciculus |
|||
olfactory |
(entorhinal |
|||
|
|
|||
|
stria |
area) |
|
Uncus with |
Prepiriform |
Reticular |
amygdaloid body |
area |
formation |
Fig. 4.7 The olfactory nerve and tract and the olfactory pathway |
|
|
Olfactory bulb |
Olfactory tract |
|
Medial olfactory |
|
Temporal pole |
stria |
|
|
Lateral olfactory |
|
|
stria |
|
|
Limen insulae |
|
Prepiriform |
|
|
|
Anterior |
|
area |
|
|
|
perforated substance |
Amygdaloid |
|
Ambient gyrus |
body |
|
|
|
|
Semilunar
Diagonal
gyrus
band of Broca
Uncus
Fig. 4.8 The olfactory nerve and tract as seen from below
Baehr, Duus' Topical Diagnosis in Neurology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.

4130 · 4 Brainstem
way is the only sensory pathway that reaches the cerebral cortex without going through a relay in the thalamus. Its central connections are complex and still incompletely known.
Connections of the olfactory system with other brain areas. An appetizing aroma excites the appetite and induces reflex salivation, while a foul smell induces nausea and the urge to vomit, or even actual vomiting. These processes also involve the emotions: some odors are pleasant, others unpleasant. Such emotions probably come about through connections of the olfactory system with the hypothalamus, thalamus, and limbic system. Among its other connections, the septal area sends association fibers to the cingulate gyrus.
The main connections of the olfactory system with autonomic areas are the medial forebrain bundle and the striae medullares thalami (Fig. 6.9, p. 277). The medial forebrain bundle runs laterally through the hypothalamus and gives off branches to hypothalamic nuclei. Some of its fibers continue into the brainstem to terminate in autonomic centers in the reticular formation, the salivatory nuclei, and the dorsal nucleus of the vagus nerve. The striae medullares thalami terminate in the habenular nucleus; this pathway then continues to the interpeduncular nucleus and the brainstem reticular formation (Fig. 6.9, p. 277).
Disturbances of smell can be classified as either quantitative or qualitative. Quantitative disturbances of smell include hyposmia (diminished smell) and anosmia(absence of smell). They are always due either to peripheral damage of the olfactory nerve, that is, of the fila olfactoria (e. g., because of rhinitis, trauma with disruption of the fila in the cribriform plate, or side effects of medication), or to central damage of the second neuron in the olfactory bulb and/or tract (olfactory groove meningioma is a classic cause). Qualitative disturbances of smell, also known as parosmias, may consist of an unpleasant cacosmia (e. g., fecal odor) or of hyperosmia (abnormally intense smell). They are usually due to central dysfunction, as in temporal lobe epilepsy.
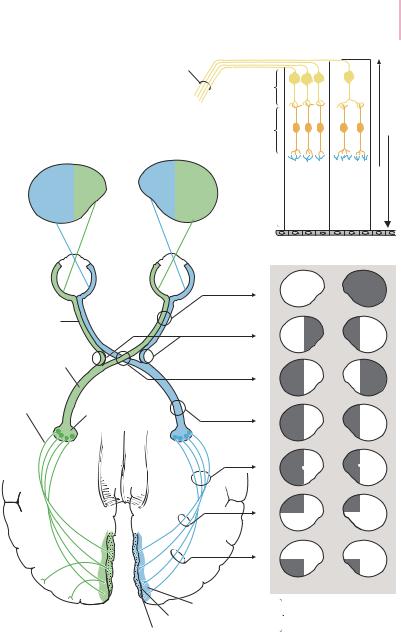
Visual System (CN II)
Visual pathway
The retina (Fig. 4.9a) is the receptor surface for visual information. Like the optic nerve, it is a portion of the brain, despite its physical location at the periphery of the central nervous system. Its most important components are the sensory receptor cells, or photoreceptors, and several types of neurons of the visual pathway. The deepest cellular layer of the retina contains the photoreceptors (rods and cones); the two more superficial layers contain the bipolar neurons and the ganglion cells.
Baehr, Duus' Topical Diagnosis in Neurology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.
Optic n.
3rd neuron: Ganglion cells
2nd neuron
Bipolar cells
Cranial Nerves · 131 4
Light
1st neuron
Rods and cones
Pigment epithelium
a







 Impulses
Impulses
Fovea Periphery
Visual cortex
Optic n. |
|
|
Optic tract |
|
|
4th neuron |
Lateral |
|
Optic radiation |
||
geniculate |
||
|
||
|
body |
Areas |
|
19 |
and |
|
18 |
b
c
Superior striate area Calcarine sulcus
Inferior striate area
Area 17
Fig. 4.9 The optic nerve and the visual pathway. a Composition of the retina (schematic drawing). b The visual pathway, with sites of possible lesions. c The corresponding visual field deficits.
Baehr, Duus' Topical Diagnosis in Neurology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.

4132 · 4 Brainstem
Rods and cones. When light falls on the retina, it induces a photochemical reaction in the rods and cones, which leads to the generation of impulses that are ultimately propagated to the visual cortex. The rods were long thought to be responsible for the perception of brightness and for vision in dim light, while the cones were thought to subserve color perception and vision in bright light. More recent research, however, has cast doubt on these hypotheses. The underlying mechanisms of these processes are probably much more complex but cannot be discussed here in any further detail.
The fovea is the site of sharpest vision in the retina and contains only cones, which project onto the bipolar cells of the next neuronal layer in a one-to-one relationship. The remainder of the retina contains a mixture of rods and cones.
The retinal image of a visually perceived object is upside-down and with left and right inverted, just like the image on the film in a camera.
Optic nerve, chiasm, and tract. The retinal bipolar cells receive input onto their dendrites from the rods and cones and transmit impulses further centrally to the ganglion cell layer. The long axons of the ganglion cells pass through the optic papilla (disk) and leave the eye as the optic nerve, which contains about 1 million fibers. Half of these fibers decussate in the optic chiasm: the fibers from the temporal half of each retina remain uncrossed, while those from the nasal half of each retina cross to the opposite side (Fig. 4.9a).
Thus, at positions distal (posterior) to the optic chiasm, fibers from the temporal half of the ipsilateral retina and the nasal half of the contralateral retina are united in the optic tract.
A small contingent of optic nerve fibers branches off the optic tracts and travels to the superior colliculi and to nuclei in the pretectal area (see Fig. 4.26). These fibers constitute the afferent arm of various visual reflexes, and, in particular, of the important pupillary light reflex, which will be discussed further below (p. 155).
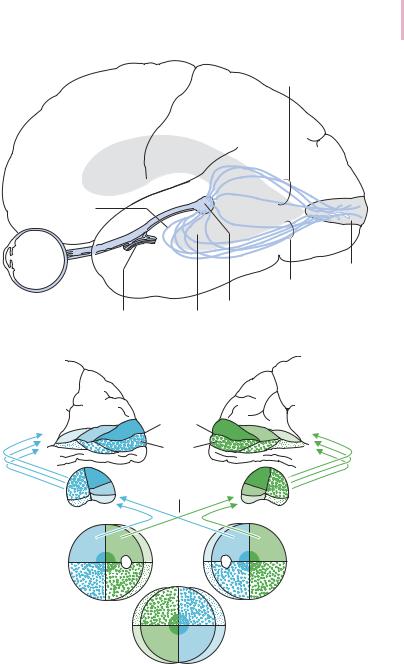
Lateral geniculate body, optic radiation, and visual cortex. The optic tract terminates in the lateral geniculate body, which contains six cellular layers. Most of the optic tract fibers end here, forming synapses with lateral geniculate neurons. These, in turn, emit fibers that run in the hindmost portion of the internal capsule (Fig. 3.2, p. 58) and then form a broad band that courses around the temporal and occipital horns of the lateral ventricle, the so-called optic radiation (of Gratiolet; see Fig. 4.10). The fibers of the optic radiation terminate in the visual cortex, which is located on the medial surface of the occipital lobe, within, above, and below the calcarine fissure (Brodmann area 17). Fibers derived from the macula occupy the largest area of the visual cortex (Fig. 4.11). Area 17 is also known as the striate cortex because it contains the stripe of Gen-
Baehr, Duus' Topical Diagnosis in Neurology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.
Cranial Nerves · 133 4
Optic radiation for lower half of the visual field
Meyer’s loop
Calcarine area
Optic radiation for upper half of the visual field
|
|
Lateral |
Chiasm |
Lateral ventricle |
geniculate |
|
(inferior horn) |
body |
Fig. 4.10 The optic radiation (of Gratriolet)
Right |
|
|
Left Projection onto |
Cuneus |
Calcarine |
|
the left visual cortex |
|
|
|
|
|
sulcus |
|
|
|
Lingual |
|
|
|
gyrus |
|
|
|
Optic |
|
|
|
chiasm |
|
Projection onto |
|
|
|
|
Right |
|
Left |
the left lateral |
|
geniculate body |
||
|
|
|
|
|
|
|
Projection onto the retina |
Right |
|
|
Left |
|
|
Overlapping |
|
|
|
visual fields |
|
Fig. 4.11 Projection of the visual fields onto the retina, lateral geniculate body, and visual cortex
Baehr, Duus' Topical Diagnosis in Neurology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.
4 134 · 4 Brainstem
Optic
tract Optic 

 chiasm
chiasm
Temporal Nasal
Macular
bundle
Retina
Optic n.
Macula
Optic disk
Macular |
bundle |
Fig. 4.12 Position of the macular bundle in the retina, optic nerve, and optic chiasm
nari, a white band composed of horizontally running fibers, which can be seen with the naked eye in sectioned anatomical specimens.
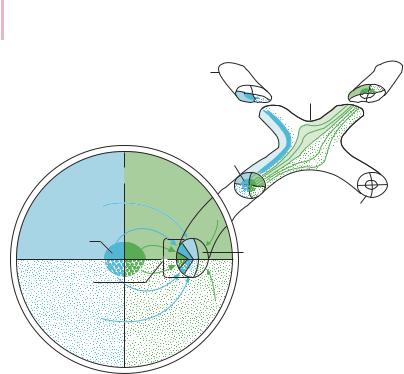
Somatotopic organization of the visual pathway. Although the fibers of the visual pathway partially decussate in the optic chiasm, a strict point-to-point somatotopic organization of the individual nerve fibers is preserved all the way from the retina to the visual cortex.
Visualinformationistransmittedcentrallyasfollows.Anobjectlocatedinthe left visual field gives rise to images on the nasal half of the left retina and the temporalhalfoftherightretina.Opticnervefibersderivedfromthenasalhalfof the left retina cross to the left side in the optic chiasm to join the fibers from the temporalhalfoftherightretinaintherightoptictract.Thesefibersthenpasstoa relay station in the right lateral geniculate body, and then by way of the right optic radiation into the right visual cortex. The right visual cortex is thus responsible for the perception of objects in the left visual field; in analogous fashion, all visual impulses relating to the right visual field are transmitted through the left optic tract and radiation into the left visual cortex (Fig. 4.9b).
Baehr, Duus' Topical Diagnosis in Neurology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.

Cranial Nerves · 135 4
Visual fibers derived from the macula are found in the temporal portion of the optic disk and in the central portion of the optic nerve (Fig. 4.12). Damage to these fibers can be seen by ophthalmoscopy as atrophy of the temporal portion of the disk (temporal pallor).
Lesions along the Visual Pathway
Optic nerve lesions. The optic nerve can be damaged at the papilla, in its anterior segment, or in its retrobulbar segment (i.e., behind the eye). Lesions of the papilla (e. g., papilledema, caused by intracranial hypertension and by a variety of metabolic disorders) can be seen by ophthalmoscopy. Lesions of the anterior segment of the optic nerve are often due to vasculitis (e. g., temporal arteritis). Retrobulbar lesions are a cardinal finding in multiple sclerosis (retrobulbar neuritis). Lesions at any of these sites can cause long-term impairment or loss of vision in the affected eye. Brief episodes of visual impairment in a single eye, lasting from a few seconds to several minutes (“transient monocular blindness”), are designated amaurosis fugax and are generally caused by microembolism into the retina. In such cases, the internal carotid artery is often the source of emboli and should be investigated for a possible stenosis.
Lesions of the optic chiasm, such as those produced by a pituitary tumor, craniopharyngioma, or meningioma of the tuberculum sellae, generally affect the decussating fibers in the central portion of the chiasm. The result is partial blindness for objects in the temporal half of the visual field of either eye, i.e., bitemporal hemianopsia (the “blinker phenomenon,” where the reference is to a horse’s blinkers). Fibers in the lower portion of the chiasm, derived from the lower portion of the chiasm, are commonly affected first by such processes; thus, bitemporal upper quadrantanopsia is a common early finding. Only color vision may be impaired at first.
Less commonly, however, a lesion of the chiasm can cause binasal hemianopsia, e. g., when a tumor has grown around the chiasm and compresses it from both sides (thus mainly affecting the laterally located, uncrossed fibers derived from the temporal halves of the two retinas, which are responsible for perception in the nasal hemifield of each eye). Aneurysms of the internal carotid artery and basilar meningitis are further possible causes, but the binasal hemianopsia in such cases is rarely pure.
Bitemporal and binasal hemianopsia are both termed heteronymous, because they affect opposite halves of the visual fields of the two eyes: the former affects the right hemifield of the right eye and the left hemifield of the left eye, while the latter affects the left hemifield of the right eye and the right hemifield of the left eye.
Baehr, Duus' Topical Diagnosis in Neurology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.
4136 · 4 Brainstem
Optic tract lesions, on the other hand, cause homonymous hemianopsia, in which the hemifield of the same side is affected in each eye. When the fibers of the right optic tract are interrupted, for example, no visual impulses derived fromtherightsideofeitherretinacanreachthevisualcortex.Theresultisblindnessinthelefthalfofthevisualfieldofeacheye(Figs.4.9b andc).Optictractlesions are usually caused by a tumor or basilar meningitis, less often by trauma.
Because an interruption of the optic tract also affects the optic nerve fibers traveling to the superior colliculi and to the pretectal area (cf. p. 155), it impairs the pupillary light reflex in response to light falling on the side of the retina
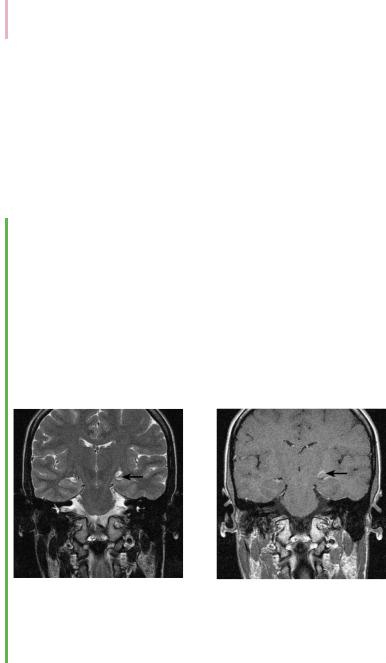
Case Presentation 1: Lesion of the Optic Tract in a Patient with Multiple Sclerosis
This 19-year-old female high-school senior, previously in excellent health, noted a visual disturbance in which she had blurry vision whenever she looked in certain directions. Within 24 hours, this blurriness spread over the entire right hemifield. She consulted her family doctor, who referred her to the hospital.
The admitting neurologist’s visual field examination revealed right homonymous hemianopsia sparing the uppermost portion of the right hemifield. The remainder of the neurological exami-
nation was normal, as were the general physical examination and all routine laboratory tests. Further tests were performed, including an MRI scan of the head, a cerebrospinal fluid examination, and recording of the visual evoked potentials (VEP). All of these tests confirmed the clinical suspicion of an inflammatory disease affecting the CNS (multiple sclerosis) producing a lesion along the course of the left optic tract. The patient was given cortisone-bolus therapy and her symptoms resolved within three days.
a |
b |
Fig. 4.13 Inflammatory lesion of the left optic tract in a patient with multiple sclerosis, as revealed by MRI. a The T2-weighted coronal image shows a hyperintense lesion along the course of the left optic radiation above the choroidal fissure, sparing only the basal portion of the optic tract (arrow). b The T1-weighted coronal image after intravenous administration of contrast material reveals enhancement at this site, indicating a focus of acute inflammation.
Baehr, Duus' Topical Diagnosis in Neurology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.
