
Understanding the Human Machine - A Primer for Bioengineering - Max E. Valentinuzzi
.pdf168 |
Understanding the Human Machine |
Exercise and to think about: With the negative feedback loop in mind, explain the conceptual mechanism of the oral contraceptives in women. Remember that these substances are estrogens and progesterone. Most of the women who were prisoners in concentration camps during the Second World War stopped their menstrual cycles. Why? Indicate in the block diagram the signal pathway. Refer to the basic concept introduced by Hans Selye, also valid for the adrenal cortex. Draw separate block diagrams for the hormonal relationships in woman and man. The menstrual cycle is one of the several biological clocks: refer to the pineal gland and try to find links. Ovulation is another still uncertain question: How does it start?
− Growth
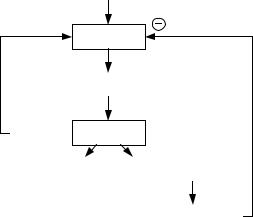
The Growth Endocrine System (GES) does not have a single target organ for its adenohypophyseal hormones — a systemic gland, as the previously described thyroid or adrenal cortex or gonads. In this case, the hypothalamus controls the adenohypophysis — its main target organ — with two secretions, the growth hormone releasing hormone (GRH) and the growth hormone inhibiting hormone (GIH) or somatostatin, with opposing effects as their names clearly identify, for the former stimulates the secretion of growth hormone (GH) and the latter inhibits its secretion from the anterior pituitary (Figure 2.64).
Growth hormone, also known as somatotropin, is a protein of about 190 amino acids that is synthesized and secreted by cells called somatotrophs in the anterior pituitary. It is a major participant in control of several complex physiologic processes, including growth and metabolism. It has direct and indirect effects. The former are the result of growth hormone binding on specific cells, such as fat cells (adipocytes), stimulating them to break down triglyceride and suppressing their ability to take up and accumulate circulating lipids. The latter, instead, are mediated primarily by an insulin-like growth factor (IGF-1), a hormone that is secreted from the liver and other tissues in response to growth hormone. IGF-1 stimulates proliferation of chondrocytes (cartilage cells), resulting in bone growth. It also appears to be the key player in muscle growth stimulating amino acid uptake and protein synthesis.
Growth hormone is one of a battery of hormones that serves to maintain blood glucose within a normal range. It has anti-insulin activity because it suppresses the abilities of insulin to stimulate uptake of glucose in peripheral tissues and enhance glucose synthesis in the liver. Somewhat

Chapter 2. Source: Physiological Systems and Levels |
169 |
paradoxically, administration of growth hormone stimulates insulin secretion, leading to hyperinsulinemia.
This amazing system has demonstrated unexpected and not yet elucidated ramifications (Figure 2.64): Somatostatin or GIH inhibits the secretion of thyroid stimulating hormone (TSH) from the adenohypophysis, insulin and glucagon from the pancreas, gastrin from the stomach and secretin from the small intestine.
FROM HIGHER CENTERS
HT
GIH |
GRH |
AP GH
 TSH
TSH
P I
G
St Gastrin
SI Secretin
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
IGF-l |
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
L |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Figure 2.64. GROWTH ENDOCRINE SYSTEM (GES). The hypothalamus (HT), always influenced from higher nervous system centers which includes external stimulation, produces two releasing hormones with opposite actions on the adenohypophysis or anterior pituitary (AP): the growth hormone-releasing hormone (GRH) and the growth hormone-inhibiting hormone (GIH), also called somatostatin. The figure also depicts the relationships with the pancreas, stomach, small intestine and liver. See text for more details.
170 |
Understanding the Human Machine |
Besides, growth hormone secretion is also part of a negative feedback loop involving IGF-1. High blood levels of IGF-1 lead to decreased secretion of growth hormone not only by directly suppressing the somatotroph, but also by stimulating release of somatostatin from the hypothalamus. GH also feeds back to inhibit GHRH secretion (Figure 2.64).
States of either growth hormone deficiency or excess provide very visible evidence to the role of this hormone in normal physiology. Clinically, deficiency leads to retardation or dwarfism. Conversely, excessive secretion of GH — very dependent on the age of onset — may lead to two distinctive disorders: giantism (very rare, usually resulting from a tumor), the result of excessive growth hormone beginning in childhood or adolescence, and acromegaly, which results from excessive secretion of growth hormone in adults.
Guillemin (1998), in his beautiful account of the development of neuroendocrinology, stated that the nature of the hypothalamic-releasing factor for growth hormone (now called GRH) was not to be established until 1982 and in a totally unexpected way, triggered by studies made on a pancreatic peripheral tumor that was functioning as an ectopic source of the much searched factor. This is one example of the fascinating serendipities of science that only the alert and well-prepared mind can catch. Thus, have always ready the reception antennas.
2.6.2.2. Hypothalamic-Neurohypophyseal System (HNHS)
Figure 2.65 briefly synthesizes the pathways involved in this system. The neurohypophysis originates from neural tissue; it stores and secretes two hormones, oxytocin and vasopressin (antidiuretic hormone or ADH). These hormones are synthesized in the cell bodies of neurons located in the hypothalamus and transported along the axons to the terminals located in the neurohypophysis and are released in response to neural stimulation.
Oxytocin acts on the uterine and vaginal smooth musculature and also on the breasts to help sperm transport during sexual intercourse or during child delivery or milk expulsion during nursing. Mechanical receptors located in these anatomical structures send afferent neural information to the hypothalamus that, in a positive loop, enhance the effects by increasing the secretion of oxytocin. The antidiuretic hormone has a direct effect on the renal distal tubules and collecting ducts permeability to produce water retention and, thus, to regulate the extracellular fluid osmolarity.
Chapter 2. Source: Physiological Systems and Levels |
171 |
FROM HIGHER CENTERS
HT
NEURAL CONNECTIONS
R PP
OXYTOCIN |
VASOPRESSIN |
|
|
OSMOLARITY
Figure 2.65. THE HYPOTHALAMIC-NEUROHYPOPHYSEAL SYSTEM (HNHS). The hypothalamus (HT), via neural connections, stimulates the secretion of oxytocin and vassopressin (or ADH) from the posterior pituitary (PP), also called neurohypophysis. Mechanical receptors R located in the genitalia, uterus, and in the breasts stimulate hypothalamic detectors to elicit contractions in the smooth musculature of these organs to favor sperm transport during sexual intercourse, birth delivery and milk secretion during nursing. ADH, in turn, has an effect on the extracellular fluid osmolarity that is constantly checked by other hypothalamic receptors, thus, establishing a negative feedback loop.
The latter is being checked by the so-called hypothalamic osmoreceptors so creating a regulatory feedback loop.
A typical derangement of this system is diabetes insipidus, which is characterized by low ADH secretion leading to polyuria (increased diuresis) because much less water is being retained. This urine is diluted and not sweet, as the case is with diabetes mellitus, that is, it does not contain glucose. There is also polydipsia (drinking of large amounts of fluid), when the thirst mechanism works correctly, to compensate for the renal water loss. Usually, the cause is a hypothalamic lesion. Alcohol induces diuresis because it inhibits ADH secretion.
Detailed and well-versed information can be found in the excellent edited book by Bayliss and Padfield (1985) or in any of the many INTERNET sites.

172 |
Understanding the Human Machine |
Thinking exercise: You have seen so far the several negative feedback loops that tend to keep in check different hormonal blood levels. Try to improve the block diagrams by searching more information in the literature. Try to devise ways of measuring the feedback gain, as it is done in technological systems. Probably, you will find many practical problems, but think in theoretical terms. An old paper by Sidney Roston (1959) may serve as inspirational source.
2.6.3. The Catecholamine System: Adrenal Medulla
The adrenal medulla, the inner part of the adrenal gland, is not essential to life, but helps a person in coping with physical and emotional stress. It consists of masses of neurons that are part of the sympathetic branch of the autonomic nervous system. Instead of releasing their neurotransmitters at a synapse, these neurons release them into the blood. Thus, although part of the nervous system, the adrenal medulla functions as an endocrine gland. It secretes epinephrine (also called adrenaline) and norepinephrine (also called noradrenaline). Both are derived from the amino acid tyrosine and are collectively called catecholamines, a group that includes other related substances with similar properties. The former hormone increases the heart rate and force of heart contractions, blood is shunted from the skin and viscera to the skeletal muscles, coronary arteries, liver, and brain, causes relaxation of smooth muscles, and helps with conversion of glycogen to glucose in the liver. Other effects include bronchial and pupillary dilatation, hair stands on end (de so-called “gooseflesh” in humans), clotting time of the blood is reduced, increased ACTH secretion from the anterior lobe of the pituitary. The latter (nor-
Figure 2.66. THE ADRENAL MEDULLA SYSTEM. The splanchnic nerves via the celiac ganglion innervate the adrenal medulla. These nerves originate in the spinal cord, at the thoracic levels 5 to 12. Thus, stimulation of them produces secretion of catecholamines. The positive feedback loop would be part of the alarm reaction.

Chapter 2. Source: Physiological Systems and Levels |
173 |
epi), instead, has little effect on smooth muscle, metabolic processes, and cardiac output, but has strong vasoconstrictive effects, thus increasing blood pressure. Students are encouraged to visit http://users.rcn.com/jkimball.ma.ultranet/BiologyPages .
This gland is innervated, via the celiac ganglion, by the splanchnic nerves, which originate in the spinal cord, at the thoracic levels 5 to 12. Thus, stimulation of them produces secretion of catecholamines. Any external stressful perturbation, such as fear or anger, may easily lead to the so-called alarm reaction perhaps enhanced by a positive feedback loop (Figure 2.66). The cardiovascular effects of catecholamines converge to at least a reversible and temporary increase in blood pressure, so explaining that common mother reproach to her children when she says “don’t bring me a headache with your behavior”. Even getting ready for an action, as before a physical exercise (a race, a given competition, or soldiers in combat) calls for the catecholamine discharge and its physio-
Figure 2.67. SPLANCHNIC STIMULATION in an anesthetized dog. The first increase in arterial blood pressure was due to the direct action of the train of pulses applied to the nerve. However, release of catecholamines was also triggered and their effect was manifested somewhat later, as demonstrated by the second hump of the record about 25 s after the stimulus was disconnected. Records obtained at the Department of Physiology, Baylor College of Medicine, Houston, TX (from the Laboratory Manual by H.E. Hoff and L.A. Geddes, 1965, referred to earlier in the text).
174 |
Understanding the Human Machine |
logical effects. There are also demonstrated neural tracts that descend from higher brain centers able to contribute to the phenomenon. Figure 2.67 illustrates the effects of electrical stimulation of the splanchnic nerve in an experimental animal.
2.6.4. The Thyroid-Parathyroid System for Calcium Regulation
Calcium concentration in plasma is well kept at 10 mg/100 mL (or 5 mEq/L or 2.5 mM/L). It is an ion of paramount importance because it plays a role in several essential physiological functions, such as blood coagulation, cardiac and skeletal muscle mechanics, electrical activity of excitable tissues and also in neuromuscular transmission. The largest calcium store is bone.
Three hormones are responsible for calcium homeostasis:
1)1,25-dihydroxycholecalciferol (DHC), which is a steroid formed in the liver and kidneys from vitamin D;
2)parathyroid hormone or parathormone (PTH), secreted by the parathyroid glands; and
3)calcitonin secreted by the thyroid and with no relationship whatsoever with the hypothalamic-adenohypophyseal system.
Figure 2.68 sumarizes calcium regulation mechanisms. Vitamin D, supplied by the daily diet, is essential for DHC production in the liver and kidneys. In the intestine, an increase of DHC stimulates absortion of calcium (second row inset) and, thus, an increase in its blood level (far right inset, lines b). DHC and PTH cause calcium resorption (release) from bone, thus, the curves relating it to DHC and PTH increase with an increase in calcium liberation (third row, center inset) and that calcium from bone contributes to an increase in blood calcium; that is represented by the input termed c in the figure. In turn, blood calcium (dashed-dotted arrows) acts as input to the thyroid and parathyroid gland, the latter decreasing its PTH production when blood calcium level increase (hence, the inverse relationship shown in the third row, left hand inset) while the former increases calcitonin secretion after the same calcium increase. PTH and calcitonin levels, in a true negative feedback loop, respectively, stimulates and inhibit bone resorption. The second effect is represented by the inverse curve (upper row, center inset). PTH has also stimulating effect in the liver and kidneys to produce DHC.

Chapter 2. Source: Physiological Systems and Levels |
175 |
Thyroid |
Calcitonin |
Blood Ca++ |
D |
Kidneys |
DHC |
|
Vitamin |
|||
& liver |
|||
|
|
Parathyroid |
PTH |
Blood Ca++
- ∆ blood Ca++
+ ∆ blood Ca++
|
resorption |
frombone |
|
|
|
|
|
||||
|
++ |
|
|
|
|
|
Ca |
|
|
|
|
|
|
|
Calcitonin |
||
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
absorption |
intestine |
|||
|
Ca |
from |
|||
|
++ |
|
|
|
|
|
|
|
|
DHC |
|
|
|
|
|
|
|
|
resorption |
frombone |
|
|
|
|
|
||||
|
++ |
|
|
|
|
|
Ca |
|
|
|
|
|
|
|
|
DHC - PTH |
|
|
|
|
|||
|
reabsorption |
fromkidney |
|||
|
++ |
|
|
|
|
|
Ca |
|
|
PTH |
|
|
|
|
|
||
a
b
++ |
a |
b, c, d |
BloodCa |
|
|
c |
|
|
|
|
a, b, c, d |
d
Figure 2.68. CALCIUM REGULATION SYSTEM.
Summarizing: PTH, a polypeptide hormone produced in the parathyroid gland, along with Vitamin D, is the principal regulator of calcium and also phosphorus homeostasis. The most important actions are: (1) rapid mobilization of calcium and phosphate from bone and long-term acceleration of bone resorption; (2) increase of renal tubular reabsorption of calcium; (3) increase of intestinal absorption of calcium (mediated by an action on the metabolism of vitamin D); and (4) decrease of renal tubular reabsorption of phosphate. These actions account for most of the important clinical manifestations of PTH excess or deficiency. Calcitonin, in turn, acts directly on osteoclasts (via specific receptors). Bone biopsies from patients treated with the drug show no effects on mineralization. It has a short half-life. Given as a subcutaneous injection showed significant improvements in bone density but there was a high incidence of side effects, including pain at the injection site, flushing and nausea, which
176 |
Understanding the Human Machine |
limited the use of the drug. Calcitonin now is available as a nasal spray, which has made it much more tolerable for patients. Calcitonin is a safe alternative to estrogen in women who cannot take estrogen.
Knowledge of this system is relatively recent (Bronner, Sammon, Stacey et al., 1967; Schweitzer, Thompson, Harness et al., 1979). Mathematical models have also been proposed (Powell and Valentinuzzi, 1974). One important surgical consequence is that in a thyroidectomy, the parathyroids must be preserved, otherwise derangemenst in the calcium system are to be expected. Another interesting concept is that of the liver as an internal secretion organ.
2.6.5. The Insulin-Glucagon System: Pancreas
In a previous section dealing with the Gastrointestinal System, the pancreas was described as an exocrine gland collaborating in the digestive process. The pancreas, however, is also an endocrine gland secreting four hormones that originate from specific cells located in well-differentiated structures called the islets of Langerhans:
a)insulin, produced by the beta or B cells (make up 60-75% of islets);
b)glucagon, secreted by the alfa or A cells (make up 20% of islets);
c)somatostatin (SS or GIH), secreted by the delta or D cells (10% of islets) ;and
d)pancreatic polypeptide, secreted by the F cells (just a few percent of islets).
The two first, insulin and glucagon, are essential in the normal regulation of blood glucose, which is maintained at a level of 80 mg/100 mL (or 80 V%). The third one could have an influence in the case of diseased pancreatic cells, such as tumors leading to hyperglycemia. The fourth — sometimes called the “hunger hormone” because it might stimulate the hunger center in the hypothalamus — suppresses SS secretions from gut and pancreas and pancreatic enzyme output, too. However, its function is not known yet. All four are dumped into the portal blood and pass through the liver before getting into the general circulation.
The curves shown in the central part of Figure 2.69 represent blood glucose (vertical axis) with insulin and glucagon concentrations, respectively, also in blood (horizontal axis). An increase in blood insulin produces a decrease in the concentration of blood glucose (curve In) while the opposite occurs when blood glucagon goes up (straight line Gl). The

Chapter 2. Source: Physiological Systems and Levels |
177 |
Figure 2.69. GLUCOSE REGULATION. Curves shown in the central part of the figure represent blood glucose in the vertical axis and insulin and glucagon concentrations, respectively, also in blood, in the horizontal axis. The operating point is Q. Inputs act on the horizontal axes and outputs come off the vertical axes. See text for details.
crossing point, Q, of both curves is the operating point. The horizontal dashed line intercepts the vertical axis at the normal blood glucose level. The beta or B-cells from the pancreas supply insulin to blood and increase their output as the glucose blood concentration goes up (left upper curve). By a similar token, the lower left relationship represents glucagon release from the alfa or A-cells as a function of blood glucose level: when the latter increases glucagon liberation goes down. The latter subsystem also feeds into blood. Glucose enters the system in the daily diet via the gastrointestinal tract and the liver constantly checks the blood glucose level; if needed, because of temporary hypoglycemia, it gives off an amount of glucose to compensate for the fall. Excretion of this sugar takes place through the kidneys when its blood concentration exceeds the threshold of about 180mg/100 mL. Finally, the tissues in general are the users of glucose for their metabolic processes. Thus, blood acts as a dynamic reservoir.
The most important derangement of pancreatic function leads to diabetes mellitus, highly frequent, largely genetic, caused by deficiency or lack of
