
Учебники / Revision Sinus Surgery Kountakis 2008
.pdf
178 |
Sarah K. Wise, Richard J. Harvey, and Rodney J. Schlosser |
46.Sillers MJ, Morgan E, El Gammal T (1997) Magnetic resonance cisternography and thin coronal computerized tomography in the evaluation of cerebrospinal fluid rhinorrhea. Am J Rhinol 11:387–392
47.Skedros DG, Cass SP, Hirsch BE, et al. (1993) Sources of error in use of beta-2 transferrin analysis for diagnosing perilymphatic and cerebral spinal fluid leaks. Otolaryngol Head Neck Surg 109:861–864
48.Stone JA, Castillo M, Neelon B, et al. (1999) Evaluation of CSF leaks: high resolution CT compared with contrast-en- hanced CT and radionuclide cisternography. AJNR Am J Neuroradiol 20:706–712
49.Tabaee A, Kassenoff TL, Kacker A, et al. (2005) The efficacy of computer assisted surgery in the endoscopic management of cerebrospinal fluid rhinorrhea. Otolaryngol Head Neck Surg 133:936–943
50.Ugarriza L, Cabedudo J, Lorenzana L, et al. (2001) Delayed pneumocephalus in shunted patients: report of three cases and review of the literature. Br J Neurosurg 15:161–167
51.Villarejo F, Carceller F, Alvarez C, et al. (1998) Pneumocephalus after shunting for hydrocephalus. Childs Nerv Syst 14:333–337
52.Watanabe K, Urade Y, Mader M, (1994) Identification of beta-trace protein as prostaglandin D synthase. Biochem Biophys Res Commun 203:1110–1116
53.Wigand ME (1981) Transnasal ethmoidectomy under endoscopic control. Rhinology 19:7–15
54.Wise SK, Harvey RJ, Neal JG, et al. (2007) Factors contributing to failure in skull base defect repair. Presented at the fall meeting of the American Rhinologic Society, September 5, Washington DC
55.Wolf G, Greistorfer K, Stammberger H (1997) Endoscopic detection of cerebrospinal fluid fistulas with a fluorescence technique: report of experience with over 925 cases. Laryngorhinootologie 76:588–594
56.Zweig JL, Carrau RL, Celin SE, et al. (2000) Endoscopic repair of cerebrospinal fluid leaks to the sinonasal tract: predictors of success. Otolaryngol Head Neck Surg 123:195–201
20
Chapter 21 |
21 |
Delayed Complications |
|
Following Sinus Trauma |
David M. Poetker and Timothy L. Smith
Core Messages
■The most common complication following sinus trauma is sinusitis, usually resulting from edema, blood, retained bone or soft-tissue fragments, or foreign bodies.
■Craniofacial trauma accounts for approximately 28% of mucoceles.
■Mucoceles can present decades after the inciting trauma, so life-long follow up is indicated.
■Foreign bodies of the paranasal sinuses are associated with trauma in 70% of cases, and most commonly involve the maxillary sinus. Thorough and complete debridement in the acute setting is essential to prevent long-term complications.
■Paranasal sinus epidermoids have been reported to occur following traumatic implantation of squamous mucosa.
■Management of paranasal sinus epidermoids involves ventilation of the affected sinuses with longterm endoscopic follow up.
■Traumatic aneurysms of the internal carotid artery can present as an isolated sinus mass.
Contents |
|
|
|
|
|
|
|
Introduction . . . . . . . |
. . |
. . |
. . |
. . |
. |
. |
179 |
Rhinosinusitis . . . . . . . . . . . . . . . . . 179 |
|||||||
Mucoceles . . . . . . . . |
. . |
. . |
. . |
. . |
. |
180 |
|
Foreign Bodies . . . . . . |
. . |
. . |
. . |
. . |
. |
. |
181 |
Silent Sinus Syndrome . . . |
. . |
. . |
. . |
. . |
. |
. |
181 |
Paranasal Sinus Epidermoids |
. . |
. . |
. . |
. . |
. |
. |
182 |
Traumatic Aneurysms . . . |
. . |
. . |
. . |
. . |
. |
. |
182 |
Cerebrospinal Fluid Leak . . |
. . |
. . |
. . |
. . |
. |
|
. 183 |
Conclusion . . . . . . . . |
. . |
. . |
. . |
. . |
. |
|
183 |
attempt to review the common, and some of the not-so- common delayed complications seen following the initial management of sinus trauma.
Rhinosinusitis
Acute complications associated with trauma include:
1.Sinus wall fractures.
2.Bleeding.
3.Sinus foreign bodies.
4.CSF leaks.
Introduction
Maxillofacial trauma is a common occurrence and has been well studied in the literature. Given the anatomical relationships, the paranasal sinuses are often involved in this trauma. Interestingly, relatively little has been written in the literature addressing the various complications of sinus trauma, and their respective management. Of the reports on sinus trauma, more attention has been paid to management of the acute complications rather than long-term or delayed complications. Management of such things as reduction of the bony fractures, removal of foreign bodies, and management of cerebrospinal fluid (CSF) leaks have all been described. In this chapter, we
Each of these should be managed in the acute setting. However, if they are not appropriately managed, they can lead to delayed complications. The most common complication following sinus trauma is rhinosinusitis. Rhinosinusitis can result from edema and blood, retained bone or soft-tissue fragments, or foreign bodies. These can obstruct the outflow tract of the sinus and/or disrupt the mucociliary function of the mucous membrane. Either can lead to mucous retention in the sinus and ultimately chronic rhinosinusitis. This has been well described in the case of frontal sinus fractures that obstruct the outflow tract [11, 14]. Often, at the time of the acute injury, the blood and edema associated with the fracture make it
180
very difficult to identify which frontal sinus fractures will result in obstruction of the outflow tract. Occasionally, a computed tomography (CT) scan obtained in a sagittal plane will help identify damage to the outflow tract. Smith and colleagues have discussed the option of medical treatment and observation of frontal sinus disease following the reduction of fractures of the anterior table of the frontal sinus, and any naso-orbitoethmoid fractures [14]. If this fails to resolve the sinus disease, a repeat of the medical management is recommended.
■Only if the second round of medical management fails do Smith et al. recommend endoscopic sinus surgery addressing the frontal sinus outflow tract [14].
This can be done through a Draf II procedure (extended endoscopic frontal sinusotomy), or a Draf III procedure (an endoscopic modified Lothrop procedure) [14]. These endonasal approaches can be augmented with a frontal sinus trephination. This allows for an additional access point for instrumentation and visualization. An osteoplastic flap may be considered in the case of a failed endonasal approach or a particularly recalcitrant case of frontal rhinossinusitis.
Post-traumatic rhinosinusitis involving the paranasal sinuses must be managed using the same principles as non-trauma-related rhinosinusitis. Initial medical management using broad-spectrum antibiotics with good sinus penetration, along with a corticosteroid to decrease outflow tract edema is recommended. Surgically, the sinus ostia must be opened, facilitating proper mucociliary function and sinus drainage. In a study reporting on maxillary sinus evaluation following trauma, the authors report that 9 of the 15 patients (60%) with maxillary sinus fractures report delayed complaints related to rhinosinusitis [16]. Six of the 9 patients required medications for the sinusitis. Follow-up CT scans of the sinuses performed between 9 and 47 months post-trauma (mean 19.8 months) showed diminished maxillary sinus volume in the traumatized sinus, mucosal thickening, and
21 bone defects; 3 patients had their maxillary sinuses filled with soft tissue [16]. Since the focus of the article was not management, no mention was made of how these patients were treated, or the outcomes following treatment.
Mucoceles
A mucocele is an expanded, mucous-filled paranasal sinus that is most commonly found in the frontal sinus [5, 10]. Chronic rhinosinusitis and allergic sinonasal disease are the most common causes of paranasal sinus mucoceles [10]. Craniofacial trauma is the reported cause in approximately 28% of mucoceles [9]. Maxillary sinus
David M. Poetker and Timothy L. Smith
mucoceles are said to account for up to 10% of all mucoceles, and are less commonly associated with trauma when compared to frontal mucoceles [2, 10]. Primary, or true mucoceles, occur when the outflow tract of the sinus is blocked, either due to trauma or inflammation. Secondary mucoceles occur when fractures result in mucosal entrapment and subsequent retention cyst formation [3, 15].
Patients present with a variety of signs and symptoms when suffering from a mucocele. These can range from severe headache to facial/sinus pressure, facial/sinus pain, vision complaints such as diplopia, and even obvious facial deformities. It is not uncommon to see bony erosion and remodeling of the sinus walls in the case of a mucocele. In the frontal sinus, this remodeling can extend anteriorly or posteriorly through the anterior and posterior tables, respectively. It can also extend inferiorly into the orbit leading to increased pressure on the globe, proptosis, and diplopia. This bony remodeling and erosion has been associated with the production of bone-resorbing factors produced by the lining of the mucoceles [15]. It is also believed that the intramucocele pressure is transmitted to the surrounding sinus bones, thus causing them to remodel. This remodeling often leads to gross changes in the shape of the sinus wall, and thinning of that wall. In the maxillary sinus, bone remodeling and erosion can lead to lateral nasal wall displacement, bulging of the hard palate, and even displacement of the maxillary alveolar dentition [2].
As mentioned, mucoceles can present years, and even decades from trauma.
■The average time between trauma and surgical confirmation of a mucocele has been reported at 7.5 years [15].
Koudstaal and his colleagues reported a series of three mucoceles following maxillofacial trauma. The longest delay in presentation in their series was 35 years [9]. For this, they advocate lifelong follow up for patients who have suffered sinus trauma. Although these are rare, they must be kept in the differential for patients presenting with a history of trauma.
Infection of the mucocele leads to formation of a mucopyocele. This infection can lead to rapid enlargement of the mucocele with increased risks of extrasinus complications.
■Pathogens associated with mucopyoceles are often common sinus pathogens associated with acute and chronic rhinosinusitis [15].
These rapid expansions of the mucocele increase the risk of intracranial complications [5]. Cultrera and colleagues report a patient who developed meningitis from a frontal

Delayed Complications Following Sinus Trauma
sinus mucocele that had eroded through the posterior table of the frontal sinus, and through the dura. The patient was 9 years out from craniofacial trauma [5].
■Management of mucoceles and mucopyoceles due to maxillofacial trauma observes the same tenets of those due to inflammatory mucosal disease.
The mucocele must be opened, and the cavity drained. Although some authors still recommend complete evacuation of the cystic cavity with complete removal of the respiratory mucosa, most otolaryngologists would argue against that [15]. By opening the mucocele and allowing for drainage, mucociliary clearance may be re-estab- lished. Often times, the bony remodeling will return to a near-normal state, responding to the external pressures on the sinus once the intramucocele pressure has been relieved.
Foreign Bodies
As discussed, sinus foreign bodies can be identified in many acute trauma settings. Foreign bodies such as glass, bone fragments, gravel, and even teeth have been reported [1, 17].
■Sinus foreign bodies reportedly occur more than half of the time in the maxillary sinus, and are associated with trauma in 70% [17].
With the use of CT as the gold standard in the diagnostic imaging of maxillofacial trauma, it seems unlikely that foreign bodies are not discovered upon the initial radiographic evaluation. However, there are reports of facial fractures being treated many years ago, before the routine use of these imaging modalities, so retained foreign body should remain on the differential. In addition, it is quite possible to misinterpret the CT findings with the usual compliment of blood and edema in the sinuses in the acute setting.
Alessandro and colleagues at the University of Rome reported a case of a 26-year-old male who presented with a 14-month history of recurrent headaches and swelling of the left upper lid region. His history was significant for a severe motor vehicle collision (MVC) 2 years prior to evaluation. During that collision, he had suffered a left fronto-orbital fracture with a laceration over the left eyelid [1]. A CT scan demonstrated a foreign body lodged subcutaneously that extended into the anterior table of the frontal sinus. The sinus demonstrated mucosal thickening in the area of the foreign body. Upon surgical debridement, it was found to be a fragment of an ink pen [1]. Long-term follow up reportedly demonstrated resolution of the patient’s symptoms.
181
Another report described a woman who suffered extensive facial fractures following an MVC [8]. These included Le Fort I, II, and III fractures, a midline palatal fracture, and a mandible fracture. A mold of her palate was made using a synthetic material made up of polyacrylic acid and polyethylmethacrylate. She underwent an open reduction of her fractures, and the palate and mandible fractures were addressed with a gunning splint. The woman recovered well from her injuries; however, she began having ipsilateral maxillary sinus complaints as soon as 1 year following the repair. She underwent several courses of antibiotics, and even a sinus washout. Although these helped, they did not solve the problem. Imaging demonstrated a right maxillary sinus opacification. Twenty-nine years after her trauma, she underwent resection of a mass from that maxillary sinus. Pathology reports described chronic inflammation with dense fibrosis, spicules of bone, and foreign material. The authors hypothesized that a small amount of the palate mold was introduced into the maxillary sinus, and the chronic sinus issues she suffered was from the sinus foreign body [8].
Silent Sinus Syndrome
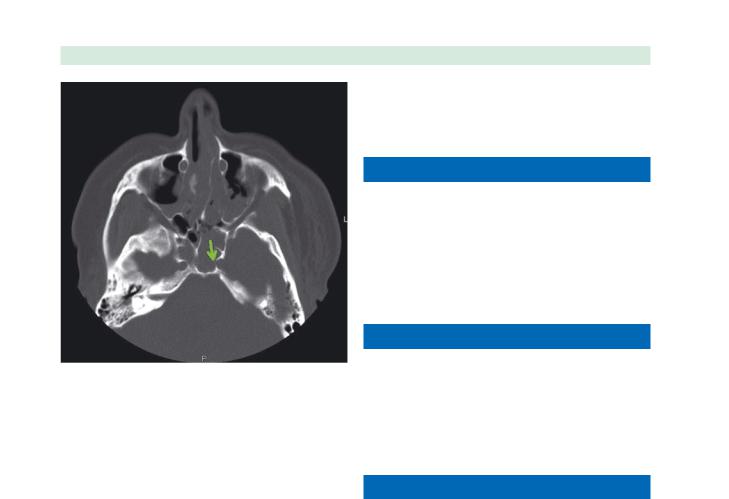
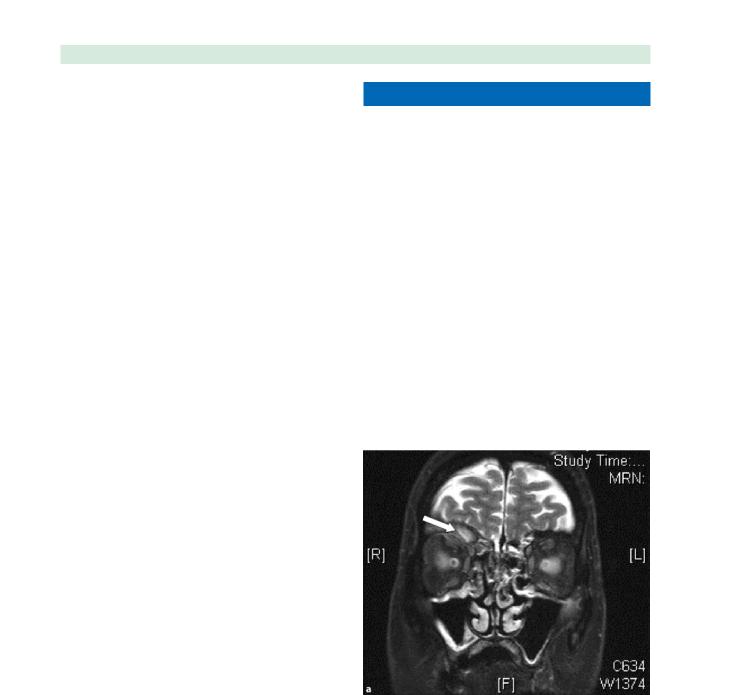
There have been two reports to date of orbital floor fractures causing a silent sinus syndrome with delayed enophthalmos and hypoglobus (Fig. 21.1) [6,13]. In the first case, a 50-year-old male was struck in the face with a tree branch, suffering a minimally displaced orbital floor fracture. His ocular motility was normal, as was his vision,
Fig. 21.1 A coronal computed tomography (CT) of the paranasal sinuses demonstrating an opacified right maxillary sinus. This patient sustained a right orbital blow out fracture 20 years prior to evaluation. She was initially referred to an ophthalmologist for contralateral proptosis. Note the right orbital floor prosthesis and the inferior displacement of the right orbital floor. Also note the lateralization of the ipsilateral uncinate process

182 |
David M. Poetker and Timothy L. Smith |
so the fracture was managed conservatively. At 2 months post-trauma, he returned to the clinic for a 2-week progressive enophthalmos with diplopia. A CT of the orbits and sinuses revealed a completely opacified ipsilateral maxillary sinus with a severely depressed orbital floor. He was taken to surgery for maxillary antrostomy and orbital floor reconstruction. He was found to have obstruction of the natural maxillary ostium from herniated orbital contents. His symptoms resolved postoperatively [6]. The second case was of a 27-year-old man who was assaulted [13]. A CT scan demonstrated a minimally displaced left zygomaticomaxillary fracture and a moderately displaced orbital floor fracture, with an air-fluid level in the ipsilateral maxillary sinus. The patient was managed conservatively because he had no functional deficit. Six months after his trauma, he re-presented with vertical diplopia, limited vertical gaze, enophthalmos, and hypoglobus. A repeat CT scan revealed left inferior orbital expansion and a left maxillary sinus contracture with complete opacification. The patient underwent maxillary antrostomy with orbital floor reconstruction. At the time of surgery, thick, opaque mucous was cleared from the sinus, with bony fragments found obstructing the maxillary ostium. The patient had resolution of his diplopia. He was observed for an additional 4 months with no recurrence of his visual disturbances [13]. The two groups hypothesized that the mechanism of action was similar to that believed to cause silent sinus syndrome, where bone or herniated orbital contents led to obstruction of the ostium. This obstruction led to hypoventilation of the sinus, which in turn led to mucosal absorption of the oxygen and a negative pressure within the sinus. This negative pressure collapsed the sinus, pulling the orbital floor inferiorly. The authors advocate management directed at reestablishing the aeration of the sinus in these cases [13].
Patients often experience chronic pain, pressure, chronic infection, and disfigurement due to expansion and erosion caused from the epidermoid [3]. In addition, it is felt that these can degenerate into a carcinoma if not adequately addressed [7].
■Treatment of epidermoid lesions includes marsupialization and exteriorization of the cyst, as well as complete excision of the cyst lining [3].
Chandra and Palmer recently reported a series of three patients with paranasal sinus epidermoids. One patient had extension of a petrous apex epidermoid; however, the remaining two patients both had histories of craniofacial trauma, supporting the theory of traumatic implantation of the squamous mucosa. One woman had an epidermoid of the pterygopalatine space that expanded anteriorly, causing the posterior wall of the maxillary sinus to bulge anteriorly. The epidermoid was widely marsupialized through the posterior wall, using a maxillary antrostomy. She remained free of disease for 30 months at last followup [3].
The second patient was a young woman who developed an expanding mass of the left supraorbital ethmoid. Initially it was felt to be a mucocele; however, upon entering into the sinus, keratinaceous debris was encountered. She too underwent a wide marsupialization into the frontal sinus. As of 14 months postdebridement, she was without evidence of disease [3]. The authors acknowledge that more aggressive management such as an osteoplastic flap for frontal or ethmoid lesions is possible. They point out that the goal of their surgery was to ventilate the sinuses with functional mucociliary clearance. They also point out that wide marsupialization without complete excision of the cyst lining requires long-term endoscopic follow up with regular debridements [3].
Paranasal Sinus Epidermoids
There are approximately two dozen reports of paranasal 21 sinus epidermoids, or cholesteatomas, in the literature
over the past 100 years [3,7].
■The most common locations of paranasal sinus epidermoids is the frontal sinus, but have also been reported in the ethmoid and maxillary sinuses [3].
Etiologic causes of epidermoid sinus tumors:
1.Congenital – they can theoretically be due to:
a.Migration of squamous epithelium.
b.Traumatic implantation.
c.Metaplasia of the native respiratory mucosa.
2.Acquired – usually felt to be due to:
a.Traumatic implantation.
b.Metaplasia [3].
Traumatic Aneurysms
Approximately one half of all intracranial traumatic aneurysms involve the internal carotid artery [12]. Of those, 60% occur in the cavernous portion of the internal carotid artery. They result from injury to all three layers of the artery, and often times are detected in the setting of fractures of the walls of the sphenoid sinus [12,18]. Interestingly, the initial angiograms performed will commonly show no aneurysm (Fig. 21.2); however, the patients may present with delayed epistaxis or an isolated sphenoid or ethmoid mass [12]. A clinical triad of craniofacial trauma, monocular blindness, and epistaxis should result in a high index of suspicion for a traumatic aneurysm. This severe epistaxis can occur anywhere from a few days to more than 6 months out from the trauma [12]. It has been recommended that an angiogram be performed in
Delayed Complications Following Sinus Trauma |
183 |
Fig. 21.2 An axial CT of the head demonstrating a fracture of the left lateral wall of the sphenoid sinus in a patient following a motor vehicle crash (arrow). An initial angiogram was negative for an aneurysm; however she remains at risk for development of a traumatic aneurysm
ernous portion of the right internal carotid artery. This was successfully embolized, and ultimately the patient did well [12].
Cerebrospinal Fluid Leak
Cerebrospinal fluid leaks can occur in both the acute and delayed settings following craniofacial and sinus trauma. The delayed CSF leaks have been reported to occur months after the initial trauma [4]. Management of these delayed leaks is similar to that for a leak following an acute injury, or of a spontaneous CSF leak. This is outlined more extensively elsewhere in this text.
Conclusion
As discussed, there is a paucity of information in the literature about long-term or delayed complications from sinus trauma. Even with a remote trauma history, complicating factors may arise. One must be aware of these potential pitfalls in order to prepare adequately for their diagnosis and management.
patients who have CT evidence of a sphenoid sinus or carotid canal fractures [18].
■Immediate angiograms should be performed in the fracture patients who have massive epistaxis.
Those without epistaxis should have an angiogram performed 2–3 weeks after the trauma. In patients without CT evidence of sphenoid sinus fractures, an angiogram should be performed if they demonstrate a delayed subarachnoid hemorrhage, unexplained neurological deterioration, or cranial nerve palsy. A repeat angiogram should be performed for patients with repeated epistaxis even if the initial angiogram was negative [18].
Ramos and colleagues present a patient who was evaluated for episodic dizziness and progressive visual complaints over an 8-year period. His past medical history was significant for severe craniofacial trauma 12 years prior to presentation. Imaging studies showed a mass in the sphenoid sinus, with the carotid arteries producing a normal signal in the region of the cavernous sinus bilaterally. The CT scan demonstrated erosion of the superior wall of the sphenoid. Initial biopsy attempts were nondiagnostic, so an endoscopic examination was performed. A well-encapsulated mass was identified, and profuse bleeding occurred when the mass was pierced. An angiogram demonstrated a very large aneurysm from the cav-
References
1.Alessandro A, Sassano P, Mustazza MC, et al. (2006) Com- plex-type penetrating injuries of craniomaxillofacial region. J Craniofac Surg 17:442–446
2.Billing KJ, Davis G, Selva D, et al. (2004) Post-traumatic maxillary sinus mucocele. Ophthalmic Surg Lasers Imaging 35:152–155
3.Chandra RK, Palmer JN (2006) Epidermoids of the paranasal sinuses and beyond: endoscopic management. Am J Rhinol 20:441–444
4.Chen K, Chen C, Mardini S, et al. (2006) Frontal sinus fractures: a treatment algorithm and assessment of outcomes based on 78 clinical cases. Plast Reconstr Surg 118:457–468
5.Cultrera F, Giuffrida M, Mancuso P (2006) Delayed posttraumatic frontal sinus mucopyocoele presenting with meningitis. J Craniomaxillofac Surg 34:502–504
6.Gagnon MR, Yeatts RP, Williams Z, et al. (2004) Delayed enophthalmos following a minimally displaced orbital floor fracture. Ophthal Plast Reconstr Surg 20:241–243
7.Hartman JM, Stankiewicz JA (1991) Cholesteatoma of the paranasal sinuses: case report review of the literature. Ear Nose Throat J 70:719–725
8.Kirkpatrick WNA, Cook C, Joshi N, et al. (2003) Complications of the orbital floor and maxillary sinus 30 years after Coe-Pak misplacement in the management of pan-facial fractures. Orbit 22:55–61

184 |
David M. Poetker and Timothy L. Smith |
9.Koudstaal MJ, Van der Wal KGH, Bijvoet HWC, et al. 14. Smith TL, Jan JK, Loehrl TA, et al. (2002) Endoscopic man-
(2004) Post-trauma mucocele formation in the frontal sinus; a rationale for follow up. Int J Oral Maxillofac Surg 33:751–754
10.Marks SC, Latoni JD, Mathog RH (1997) Mucoceles of the maxillary sinus. Otolaryngol Head Neck Surg 117:18–21
11.Poetker DM, Smith TL (2006) Endoscopic treatment of the frontal sinus outflow tract in frontal sinus trauma. Oper Tech Otolaryngol Head Neck Surg 17:66–72
12.Ramos A, Tobio R, Ley E, et al. (1996) Traumatic aneurysm of the internal carotid artery: a late finding presenting as a mass in the sphenoid sinus. Am J Neuroradiol 17:222–225
13.Ross JJ, Kersten RC (2005) Late enophthalmos mimicking silent sinus syndrome secondary to orbital trauma. J Craniofac Surg 16:840–843
agement of the frontal recess in frontal sinus fractures: a shift in the paradigm? Laryngoscope 112:784–790
15.Smoot EC III, Bowen DG, Lappert P, et al. (1995) Delayed development of an ectopic frontal sinus mucocele after pediatric cranial trauma. J Craniofac Surg 6:327–331
16.Top H, Aygit C, Sarikaya A, et al. (2004) Evaluation of maxillary sinus after treatment of midfacial fractures. J Oral Maxillofac Surg 62:1229–1236
17.Tung T, Chen Y, Santamaria E, et al. (1998) Dislocation of anatomic structures into the maxillary sinus after craniofacial trauma. Plast Reconstr Surg 101:1904–1908
18.Uzan M, Cantasdemir M, Seckin MS, et al. (1998) Traumatic intracranial carotid tree aneurysms. Neurosurgery 43:1314–1320
21
Chapter 22
Recurrent Mucoceles |
22 |
Benjamin Bleier, James N. Palmer, and Bradford A. Woodworth |
Core Messages
■Management of recurrent mucoceles has shifted from open surgical resection toward more conservative, endoscopic marsupialization techniques.
■Recurrent mucocele formation may result from incomplete marsupialization of the primary lesion or unfavorable scarring of a sinus ostium or free mucosal edge.
■Mucoceles that violate the boundaries of the sinonasal cavity are at higher risk for recurrence due to the increased complexity of complete marsupialization by strictly endoscopic techniques.
■Infected mucoceles (mucopyoceles) can rapidly expand and increase the incidence of local complications.
■Computed tomography is absolutely required for evaluation and preoperative management, and magnetic resonance imaging is highly recommended if the primary lesion demonstrates skull-base erosion or frank intracranial extension.
■The overall goal of revision mucocele surgery includes complete adjacent sinusotomy followed by wide-field marsupialization of the cyst wall to minimize the risk of scarring and entrapment of residual secretory mucosa.
■Extended frontal sinus procedures, such as the Draf III (endoscopic modified Lothrop) procedure, are often necessary for recurrent frontal sinus mucoceles to increase the chances of success.
■Partial (modified) endoscopic medial maxillectomy is recommended for recurrent maxillary sinus mucoceles.
■Sphenoid mucoceles are addressed via a transnasal/ transseptal or transethmoid approach.
■Endoscopic drainage appears to be an effective technique with little morbidity in the proper hands. However, open approaches are still necessary in select cases.
Contents |
|
|
|
|
Introduction . . . . . . . . . . . . . |
. . |
. |
. |
185 |
Epidemiology . . . . . . . . . . . . |
. . . |
. |
|
. 185 |
Pathophysiology . . . . . . . . . . . . . . . . 186 |
||||
Presentation . . . . . . . . . . . . . |
. . |
. |
. |
186 |
Preoperative Workup . . . . . . . . . . . . . . 186 |
||||
Surgical Technique . . . . . . . . . . |
. . . |
. |
|
. 187 |
Frontal Sinus Mucoceles . . . . . . . |
. . |
. |
. |
189 |
Maxillary Sinus Mucoceles . . . . . . |
. . |
. |
. |
190 |
Ethmoid and Sphenoid Sinus Mucoceles |
. . |
. |
. |
190 |
Postoperative Care . . . . . . . . . . |
. . . |
. |
|
. 191 |
Outcomes . . . . . . . . . . . . . . |
. . |
. |
192 |
|
Conclusion . . . . . . . . . . . . . |
. . . |
. |
|
192 |
Introduction
Sinonasal mucoceles are indolent, expansile cysts that contain mucus and are lined with functional respiratory epithelium. These benign lesions may be locally destructive due to chronic expansion with reactive bone remodeling and may become secondarily infected, resulting in a mucopyocele. Classically, recurrent lesions were felt to require complete surgical resection, often with obliteration of the involved sinus cavities. With the advent of endoscopic surgical techniques and newer imaging modalities over the past 30 years, management of recurrent mucoceles has shifted toward more conservative marsupialization techniques.
Epidemiology
Mucoceles most commonly present between the ages of 40 and 60 years and have no discernable sex predilection [1]. Those presenting in children are usually idiopathic, although some authors advocate cystic fibrosis screening
186 |
Benjamin Bleier, James N. Palmer, and Bradford A. Woodworth |
in any child found to have a mucocele [5, 7]. Paranasal sinus mucoceles occur most frequently in the frontal sinus [11]. Several large case series have reported incidences of 60–90% in the frontal sinus and 8–30% within the ethmoid sinus. Mucoceles of the maxillary and sphenoid sinus are rare, although some authors report an incidence of up to 5% and 10%, respectively [1, 9, 13].
Pathophysiology
The current paradigm for management of mucoceles and their recurrences derives from a more complete understanding of the pathophysiology of this disease. Studies by Lund et al. [14] demonstrated that the mucocele lining is composed of functional respiratory mucosa, namely ciliated pseudostratified columnar epithelium.
■Primary and recurrent mucocele development can be extrapolated to an event resulting in retained mucus with a concomitant loss of a normal outflow tract.
One proposed mechanism of primary mucocele formation implicates the cystic degeneration of a seromucinous gland with formation of a retention cyst [2]. Sinus outflow obstruction resulting from intranasal neoplasm or iatrogenic causes may also contribute to mucocele formation. One series reported a 9.3% incidence of frontal sinus mucocele following osteoplastic flap [8]. Recurrent mucocele formation may result from incomplete marsupialization of the primary lesion or unfavorable scarring of a sinus ostium or free mucosal edge. Other etiologic factors include a history of chronic sinusitis, allergic rhinitis, and previous maxillofacial trauma.
■Once formed, mucoceles may affect bony remodeling via an inflammatory cascade focused at the bone–mu- cocele interface.
Inflammatory mediators including interleukin (IL)-1 and IL-2 as well as fibroblast-derived prostaglandin E2 and collagenase act to promote bone resorption, which in
22 conjunction with the mass effect of the lesion itself, can result in local bony destruction and displacement of adjacent soft tissue structures [14–16].
Local complications arise from chronic cyst wall expansion that may result in intraorbital extension with globe displacement or skull-base erosion. The incidence of intracranial extension has been reported as high as 55%, half of which had a larger intracranial than sinus component [9]. Lesions that violate the boundaries of the sinonasal cavity tend to be at higher risk for recurrence secondary to the increased complexity of complete marsupialization by strictly endoscopic techniques [18].
Bacterial invasion of the cyst can also occur, resulting in a mucopyocele. This may lead to rapid expansion of the lesion with a resultant increased incidence of local complications. Common culture isolates from these lesions include Staphylococcus aureus, alpha-hemolytic
Streptococci, Haemophilus influenzae, Pseudomonas aeruginosa, and anaerobes including Propionibacterium acnes, Prevotella, and Fusobacterium [3, 5].
■Common etiologies of paranasal sinus mucoceles include:
1.Chronic rhinosinusitis.
2.Prior sinus surgery (external or endoscopic).
3.Maxillofacial trauma.
4.Allergy.
5.Neoplasm.
6.Idiopathic.
Presentation
Presenting symptoms of a recurrent mucocele are often referable to its location and include congestion, headache, rhinorrhea, and pressure. Diplopia, eye pain, decreased visual acuity, epiphora, and proptosis may be present with significant intraorbital involvement. In some cases of recurrent disease, prior loss of bony orbital architecture may result in profound exophthalmos, leading to exposure keratopathy and central retinal block [6]. Frontal mucoceles may also present with a forehead mass secondary to erosion of the anterior table. Conversely, patients with full-thickness posterior table erosion may present with a cerebrospinal fluid leak or meningitis.
Preoperative Workup
The evaluation of a patient with a suspected recurrent mucocele relies primarily on history and physical exam coupled with radiographic evaluation. If the prior marsupialization included sinusotomy with skull-base clearance, a portion of the cyst wall may be readily apparent on nasal endoscopy. While plain films have been utilized in the past to assess paranasal sinus disease, computed tomography (CT) has become the modality of choice to evaluate these lesions. Mucoceles appear as well-circum- scribed cysts with homogenous mucoid contents whose attenuation increases with chronicity of the lesion secondary to increasing protein content (10–40 Hounsfield Units). High-resolution images in both axial and coronal planes provide valuable information regarding the integrity of surrounding bony structural elements and help to plan surgical intervention.
Recurrent Mucoceles
Magnetic resonance imaging (MRI) is also useful when attempting to differentiate between mucocele and other sinonasal soft tissue lesions, and is highly recommended if the primary lesion demonstrates skull-base erosion or frank intracranial extension. Mucoceles will be low intensity on T1-weighted and gadolinium-enhanced images, while appearing high intensity on T2-weighted imaging [13].
■Imaging the characteristics of mucoceles:
1.Computed Tomography.
a.Non-contrast enhanced.
b.Well circumscribed with homogenous mucoid content.
i.New lesions 10–18 Hounsfield Units.
ii.Chronic Lesions 20–40 Hounsfield Units.
c.Contrast enhanced.
d.Rim enhancement.
2.Magnetic resonance imaging.
a.T1-weighted sequence – dark.
b.T2-weighted sequence – bright.
c.Gadolinium enhanced – does not enhance.
Several systems have been devised that classify mucoceles according to the site and degree of local invasion. Intracranial extent is a critical element in most systems as it predicts surgical complexity and potential need for skullbase repair or sinus obliteration at the time of surgery.
■Classification of paranasal sinus mucoceles [4]:
1.Type 1 – anterior without intracranial extension.
2.Type 2 – anterior with intracranial extension.
3.Type 3 – posterior midline without intracranial extension.
4.Type 4 – posterior with intracranial extension.
■As part of the preoperative evaluation the surgeon should do the following:
1.Perform a complete history and physical examination including nasal endoscopy.
2.Obtain a high-resolution CT with axial and coronal cuts. The use of image guidance for recurrent lesions is advocated.
187
Surgical Technique
Traditionally, open surgical resection, rather than marsupialization, was the gold standard treatment for primary or recurrent sinonasal mucoceles. Techniques such as the Lynch-Howarth frontoethmoidectomy or osteoplastic flap with subsequent sinus obliteration were associated with significant morbidity and cosmetic deformity as well as a relatively high recurrence rate [17]. As early as 1921 it was recognized that marsupialization was a rational alternative to these more radical approaches. This concept has been supported by subsequent studies demonstrating essentially normal mucociliary transport mechanisms within previously marsupialized cavities [10]. With the introduction of nasal endoscopes, microsurgical instruments, and image-guided surgical navigation, endoscopic transnasal marsupialization has become the treatment of choice and obviated the need for external incisions in the vast majority of cases.
Surgical management of recurrent lesions is largely dictated by the location, amount of residual bony partitions, and degree of local extension noted on preoperative CT.
Fig. 22.1 Supraorbital ethmoid sinus mucocele. A patient with
3.Carefully review CT with specific attention to site a history of right frontal mucocele drained at an outside institu- of involvement, the presence of bony erosion, and tion presented with proptosis and eye pain. T2-weighted coro-
the degree of intraorbital and/or intracranial extension.
nal magnetic resonance imaging scan reveals a right supraorbital ethmoid mucocele (white arrow) that probably developed
4.Obtain an MRI with any significant intracranial in- secondary to inadequate drainage and iatrogenic scarring of the volvement in primary or recurrent lesions or con- supraorbital outflow tract. a Intraoperative triplanar imaging
cern over sinonasal neoplasm. |
and endoscopic view following drilling with a 70 diamond burr. |
|
b Intraoperative computed tomography (CT) scan and real-time |
|
updating of image-guidance was performed to confirm that the |
|
mucocele was completely marsupialized (c) b–c see next page |
