
Gale Encyclopedia of Genetic Disorder / Gale Encyclopedia of Genetic Disorders, Two Volume Set - Volume 1 - A-L - I
.pdf
Bardet-Biedl syndrome
KEY TERMS
Brachydactyly—Abnormal shortness of the fingers and toes.
Electroretinogram (ERG)—A measurement of electrical activity of the retina.
Intravenous pyelogram—An x ray assessment of kidney function.
Linkage analysis—A method of finding mutations based on their proximity to previously identified genetic landmarks.
Polydactyly—The presence of extra fingers or toes.
Retinitis pigmentosa—Degeneration of the retina marked by progressive narrowing of the field of vision.
Syndactyly—Webbing or fusion between the fingers or toes.
tion begin in early childhood. Learning disabilities, if present, are identified in school-aged children, if not earlier. Failure to menstruate leads to diagnosis of some adolescent girls. Infertility brings some young adults to medical attention. Kidney disease is progressive and may not become obvious until adulthood.
Due to progressive degeneration of the retina, vision damage occurs in all patients. Specific vision defects include poor night vision during childhood, severe myopia (nearsightedness), glaucoma, and cataracts. A few patients suffer from retinitis pigmentosa, a condition in which the field of vision progressively narrows. Most individuals affected with BBS are blind by age 30.
Many infants with BBS are born with a kidney defect affecting kidney structure, function, or both. The specific abnormality varies from patient to patient and may be aggravated by lifelong obesity, another common problem for BBS patients. The complications of obesity, such as high blood pressure (hypertension) and insulin-resistant diabetes mellitus, contribute to kidney disease.
BBS patients may have extra fingers or toes (polydactyly), short fingers (brachydactyly), or broad, short feet. Some patients have a combination of all three of these features. Alternately, polydactyly may be limited to one limb, hands only, or feet only. Syndactyly, the fusion of two or more fingers or toes, may also occur. In some BBS families, all affected members display at least some of these limb abnormalities.
Many individuals with BBS have genital abnormalities. Most boys with BBS have a very small penis and
some also have undescended testes. Men with BBS are usually unable to have children. In women with BBS, the genitalia, ovaries, fallopian tubes, and uterus may or may not be underdeveloped. The vagina may not be completely formed. Though some women with BBS do not menstruate, others menstruate irregularly, and some women are able to have children. In both sexes, there may be birth defects in the urinary or gastrointestinal tract.
Some research indicates that people with BBS have characteristic facial features, including a prominent forehead, deep-set eyes, flat nasal bridge, and thin upper lip. Teeth are small and crowded, and a high, arched palate is common.
Occasionally, individuals with BBS have liver disease or heart abnormalities.
In addition to the physical effects of the condition, intelligence is sometimes affected. While some BBS patients show normal intelligence, others have mild to moderate learning disabilities. These patients are often developmentally delayed—they are slower than most children to walk, speak, or reach other developmental milestones. Difficulty with language and comprehension may continue into adulthood. In a few people with BBS, more severe mental retardation occurs. In some patients, vision handicap and developmental delay appear to be related.
Some parents report that their children with BBS have behavioral problems that continue into adulthood. These include lack of inhibition and social skills, emotional outbursts, and obsessive-compulsive behavior. Most people with BBS prefer fixed routines and are easily upset by a change in plans.
Diagnosis
Diagnosis of BBS is a challenge for medical professionals. Not only do the symptoms of BBS vary greatly from patient to patient, but some of these symptoms occur in other conditions, many of which are more common than BBS.
Though available on a research basis, genetic testing for BBS is not yet offered through clinical laboratories. Instead, it is the association of many BBS symptoms in one patient that generally leads to a clinical diagnosis. Therefore, patients must have a thorough genetic evaluation. This provides a chance to rule out other disorders with similar symptoms. Because symptoms emerge throughout childhood, patients diagnosed as infants require regular exams to confirm proper diagnosis. Some disorders historically confused with BBS include Lawrence-Moon syndrome, Kearns-Sayre syndrome, and
McKusick-Kaufman syndrome. This last syndrome is also caused by mutation in the MKKS gene; in fact, the
138 |
GALE ENCYCLOPEDIA OF GENETIC DISORDERS |

gene took its name from McKusick-Kaufman syndrome. While people with this syndrome show some of the same symptoms as BBS patients, the specific MKKS mutation differs between the conditions. This explains how one gene can be responsible for two distinct yet similar disorders.
Six major criteria form the basis of BBS diagnosis. These are retinal degeneration, polydactyly, obesity, learning disabilities, kidney abnormalities, and genital defects (in males). To confirm diagnosis, the patient should receive three particular diagnostic tests. An eye exam called an electroretinogram is used to test the electric currents of the retina. An ultrasound is used to examine the kidneys, as is an intravenous pyelogram (IVP). An IVP is an x-ray assessment of kidney function.
Treatment and management
Unless they have severe birth defects involving the heart, kidneys, or liver, patients with BBS can have a normal life span. However, obesity and kidney disease are major threats. If unchecked, obesity can lead to high blood pressure, diabetes mellitus, and heart disease. Untreated kidney disease can lead to renal failure, a frequent cause of early death in patients with BBS. Some patients require dialysis and kidney transplant. Therefore, it is very important to monitor and manage patients with BBS, and to promptly treat any complications. Affected individuals should eat a well-balanced, low-calorie diet and exercise regularly.
Because BBS carriers also appear prone to kidney disease, parents and siblings of patients with BBS should take extra precautions. These include baseline screening for kidney defects or cancer, as well as preventive health care on a regular basis.
In order to conserve vision to the extent possible, retinal degeneration should be carefully monitored. Therapy, education, and counseling help prepare the patient for progressive loss of vision. The Foundation Fighting Blindness, a support and referral group, offers help to BBS patients and their families.
Though not life-threatening, learning disabilities and reproductive dysfunction need attention in order to maximize the quality of life for patients with BBS. Affected people benefit greatly from special or vocational education, speech therapy, social skills training, and community support services. Some adult patients may never be able to live independently and may remain with their families. In these cases, families should plan future living arrangements in case the patients outlive their caregivers.
Genital abnormalities may require hormonal treatment or surgical attention. Sometimes removal of undescended testes is necessary to prevent cancer. Patients with genital and reproductive dysfunction may need
counseling to help them deal with the personal, familial, social, and cultural impact of the condition. Genetic counseling is available to help fertile BBS patients address their reproductive choices.
Prognosis
The outlook for people with BBS depends largely on the extent of the birth abnormalities, prompt diagnosis, and follow-up care. At this time there is no treatment for the extensive retinal damage caused by BBS. However, good health care beginning in childhood can help many people with BBS avoid other serious effects of this disorder. Researchers are actively exploring genetic causes, treatment, and management of BBS.
Resources
BOOKS
“Bardet-Biedl Syndrome.” In Smith’s Recognizable Patterns of Human Malformation. 5th ed. Philadelphia: W. B. Saunders, 1997, pp. 590-591.
PERIODICALS
Beales, P. L., et al. “New Criteria for Improved Diagnosis of Bardet-Biedl Syndrome: Results of a Population Survey.”
Journal of Medical Genetics 36 (1999): 437-446.
Foltin, Lynn. “Researchers Identify Inherited Obesity, Retinal Dystrophy Gene.” Texas Medical Center News 22 (2000): 17.
Hrynchak, P. K. “Bardet-Biedl Syndrome.” Optometry and Vision Science 77 (May 2000): 236-243.
ORGANIZATIONS
Foundation Fighting Blindness. Executive Plaza 1, Suite 800, 11350 McCormick Rd., Hunt Valley, MD 21031. (888) 394-3937. http://www.blindness.org .
Genetic Alliance. 4301 Connecticut Ave. NW, #404, Washington, DC 20008. (800) 336-GENE (Helpline) or (202) 9665557. Fax: (888) 394-3937. info@geneticalliance.http://www.geneticalliance.org .
WEBSITES
“Bardet Biedl Syndrome.” NORD—National Organization for Rare Disorders. http://www.raredisorders.org .
Avis L. Gibons
I Batten disease
Definition
Batten disease is a disorder of the nervous system that begins in childhood. Symptoms of the disorder include mental impairment, seizures, and loss of sight and motor skills.
disease Batten
GALE ENCYCLOPEDIA OF GENETIC DISORDERS |
139 |
Batten disease
KEY TERMS
Lipopigments—Substances made up of fats and proteins found in the body’s tissues.
Lysosome—Membrane-enclosed compartment in cells, containing many hydrolytic enzymes; where large molecules and cellular components are broken down.
Neuronal ceroid lipofuscinoses—A family of four progressive neurological disorders.
Description
Batten disease is characterized by an abnormal buildup of lipopigments—substances made up of fats and proteins—in bubble-like compartments within cells. The compartments, called lysosomes, normally take in and break down waste products and complex molecules for the cell. In Batten disease, this process is disrupted, and the lipopigments accumulate. This breakdown is genetic. It is marked by vision failure and the loss of intellect and neurological functions, which begin in early childhood.
Batten disease is a form of a family of progressive neurological disorders known as neuronal ceroid lipofuscinoses (or NCLs). It is also known as Spielmeyer-Vogt- Sjögren-Batten disease, or juvenile NCL. There are three other disorders in the NCL family: Jansky-Bielchowsky disease, late infantile neuronal ceroid lipofuscinosis, and Kufs disease (a rare adult form of NCL). Although these disorders are often collectively referred to as Batten disease, Batten disease is a single disorder.
Genetic profile
Batten disease was named after the British pediatrician who first described it in 1903. It is an autosomal recessive disorder. This means that it occurs when a child receives one copy of the abnormal gene from each parent. Batten disease results from abnormalities in gene CLN3. This specific gene was identified by researchers in 1995.
Individuals with only one abnormal gene are known as carriers; they do not develop the disease but can pass the gene on to their own children. When both parents carry one abnormal gene, their children have a one in four chance of developing Batten disease.
Demographics
Batten disease is relatively rare, occurring in two to four of every 100,000 births in the United States. NCLs
appear to be more common in children living in Northern Europe and Newfoundland, Canada.
Signs and symptoms
Early symptoms of Batten disease include vision difficulties and seizures. There may also be personality and behavioral changes, slow learning, clumsiness, or stumbling. These signs typically appear between ages five and eight. Over time, the children experience mental impairment, worsening seizures, and the complete loss of vision and motor skills.
Batten disease, like other childhood forms of NCL, may first be suspected during an eye exam that displays a loss of certain cells. Because such cell loss can occur in other eye diseases, however, the disorder cannot be diagnosed by this sign alone. An eye specialist who suspects Batten disease may refer the child to a neurologist, who will analyze the medical history and information from various laboratory tests.
Diagnosis
Diagnostic tests used for Batten disease and other NCLs include:
•Blood or urine tests that detect abnormalities that may indicate Batten disease
•Skin or tissue sampling, which can detect the buildup of lipopigments in cells
•Electroencephalogram, which displays electrical activity within the brain that suggests a person has seizures
•Electrical studies of the eyes that further detect various eye problems common in childhood NCLs
•Brain scans, which spot changes in the brain’s appearance
Treatment and management
There is no known treatment to prevent or reverse the symptoms of Batten disease or other NCLs. Anticonvulsant drugs are often prescribed to reduce or control seizures. Other medicines may be prescribed to manage other symptoms associated with the disorder. Physical and occupation therapy may also help people retain function for a longer period of time. Scientists’ recent discovery of the genes responsible for NCLs may help lead to effective treatments.
There have been reports of the slowing of the disease among children who were given vitamins C and E and diets low in vitamin A. However, the fatal outcome of the disease remained the same.
140 |
GALE ENCYCLOPEDIA OF GENETIC DISORDERS |
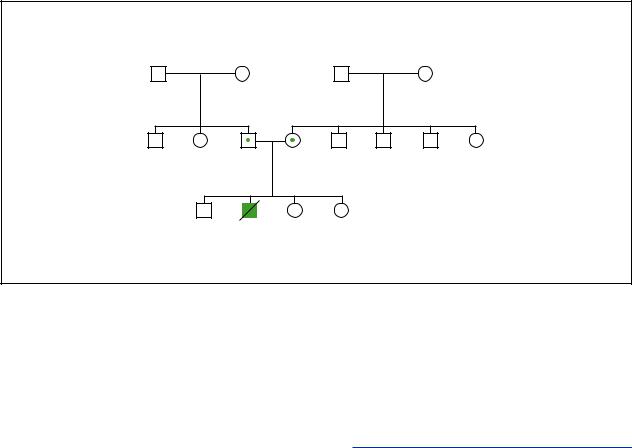
Batten Disease
("Classic" form)
d.9y Seizures Mental delays Loss of sight
(Gale Group)
Prognosis |
BBB syndrome see Opitz syndrome |
People with Batten disease may become blind, confined to bed, and unable to communicate. Batten disease is typically fatal by the late teens or 20s. Some people with the disorder, however, live into their 30s.
Resources
ORGANIZATIONS
Battens Disease Support and Research Association. 2600 Parsons Ave., Columbus, OH 43207. (800) 448-4570.http://www.bdsra.org. .
Children’s Brain Disease Foundation. 350 Parnassus Ave., Suite 900, San Francisco, CA 94117. (415) 566-5402.
Children’s Craniofacial Association. PO Box 280297, Dallas, TX 75243-4522. (972) 994-9902 or (800) 535-3643. contactcca@ccakids.com. http://www.ccakids.com .
JNCL Research Fund. PO Box 766, Mundelein, IL 60060.http://www.jnclresearch.org .
National Organization for Rare Disorders (NORD). PO Box 8923, New Fairfield, CT 06812-8923. (203) 746-6518 or (800) 999-6673. Fax: (203) 746-6481. http://www
.rarediseases.org .
WEBSITES
“Batten Disease Fact Sheet.” (June 2000). National Institute of Neurological Disorders and Stroke. http://www.ninds
.nih.gov/health_and_medical/pubs/batten_disease.htm . “Gene for Last Major Form of Batten Disease Discovered.”
(September 18, 1997). National Institute of Diabetes and Digestive and Kidney Disorders. http://www.niddk.nih
.gov/welcome/releases/9_18_97.htm
Michelle Lee Brandt
I Beals syndrome
Definition
Beals syndrome, also known as Beals contractural arachnodactyly (BCA), congenital contractural arachnodactyly, or Beals-Hecht syndrome, is a rare genetic disorder that involves the connective tissue of the skeleton.
Description
Individuals diagnosed with Beals syndrome usually have long, thin, fingers and toes that cannot be straightened out because of contractures, meaning a limited range of motion in the joints of their fingers, hips, elbows, knees, and ankles. They also have unusual external ears that appear crumpled. Contractures of the elbows, knees, and hips at birth are very common. Some babies also have clubfoot, causing one or both feet to be turned in towards each other at the ankles. In most individuals, the contractures improve with time and the clubfoot responds well to physiotherapy.
The condition occurs when fibrillin, an important component of the body’s connective tissue (the glue and scaffolding of the body; for example bones, cartilages,
syndrome Beals
GALE ENCYCLOPEDIA OF GENETIC DISORDERS |
141 |

Beals syndrome
KEY TERMS
Amniocentesis—A procedure performed at 16-18 weeks of pregnancy in which a needle is inserted through a woman’s abdomen into her uterus to draw out a small sample of the amniotic fluid from around the baby. Either the fluid itself or cells from the fluid can be used for a variety of tests to obtain information about genetic disorders and other medical conditions in the fetus.
Chromosome—A microscopic thread-like structure found within each cell of the body and consists of a complex of proteins and DNA. Humans have 46 chromosomes arranged into 23 pairs. Changes in either the total number of chromosomes or their shape and size (structure) may lead to physical or mental abnormalities.
Connective tissue—A group of tissues responsible for support throughout the body; includes cartilage, bone, fat, tissue underlying skin, and tissues that support organs, blood vessels, and nerves throughout the body.
Contracture—A tightening of muscles that prevents normal movement of the associated limb or other body part.
Fibrillin-2—A protein that forms part of the body’s connective tissue. The precise function of fibrillin- 2 is not known.
Kyphosis—An abnormal outward curvature of the spine, with a hump at the upper back.
Mitral valve prolapse—A heart defect in which one of the valves of the heart (which normally controls blood flow) becomes floppy. Mitral valve prolapse may be detected as a heart murmur but there are usually no symptoms.
Mutation—A permanent change in the genetic material that may alter a trait or characteristic of an individual, or manifest as disease, and can be transmitted to offspring.
Protein—Important building blocks of the body, composed of amino acids, involved in the formation of body structures and controlling the basic functions of the human body.
Scoliosis—An abnormal, side-to-side curvature of the spine.
tendons, and fibers) is not made properly by the body. The gene responsible for making fibrillin is called FBN2 and it is located on chromosome 5. Any mutation (change) occurring in the FBN2 gene results in Beals syndrome.
Genetic profile
Beals syndrome is caused by a mutation occurring in a gene. Genes are units of hereditary material passed from a parent to a child through the egg and sperm. The information contained in genes is responsible for the development of all the cells and tissues of the body. Most genes occur in pairs: one copy of each pair is inherited from the egg cell produced by the mother and the other copy of each pair comes from the sperm cell of the father. One of these genes (called FBN2) tells the body how to make fibrillin-2, a specific type of protein. Proteins are substances made in the body that consist of chemicals called amino acids. Fibrillin-2 is an important part of connective tissue. Connective tissue provides structural support and elasticity to the body. It is made up of various components, including elastic-like fibers, and fib- rillin-2 is thought to play a role in ensuring that the elastic fibers of the connective tissue are assembled properly early in development; however, the precise function of fibrillin-2 remains unknown. People with Beals syndrome have a mutation in one copy of their FBN2 gene. As a result, the fibrillin-2 they make is unable to work properly and this causes the BCA symptoms.
Beals syndrome is inherited as a dominant condition. In dominant conditions, a person needs to have only one altered gene copy to develop the condition. The mutation in the FBN2 gene that causes Beals syndrome can be inherited from a parent who is also affected with BCA. Individuals with Beals syndrome have a 50% chance in each pregnancy to have a child with Beals syndrome.
Sometimes Beals syndrome cannot be traced back to a parent with the condition. In these cases, the genetic change is said to be a spontaneous mutation. This means that some unknown event has caused the FBN2 gene (which functions normally in the parent) to mutate in either the sperm of the father or the egg of the mother. If fertilization occurs, the resulting individual will have Beals syndrome. A person who has Beals syndrome due to a spontaneous mutation can then pass on this altered FBN2 gene to his or her future children.
Demographics
Beals syndrome affects males and females of all ethnic groups. It is a rare condition and accurate estimates of the number of affected people are not available.
Signs and symptoms
Besides the general appearance displayed by persons with Beals syndrome (tall and thin, contractures, with typical crumpled ear), symptoms of the disorder vary from one affected individual to the next. Sometimes,
142 |
GALE ENCYCLOPEDIA OF GENETIC DISORDERS |
arms are disproportionately long for the height of the person. Other less common features may include a small chin, protruding forehead, and a high arch in the roof of the mouth (palate).
An abnormal bending or twisting of the spine (kyphosis/scoliosis) is seen in about half of individuals diagnosed with Beals syndrome and can occur in early infancy. This bending and twisting of the spine tends to worsen over time. Some individuals may also have an abnormal indentation or protrusion of their chest wall. Decreased muscle bulk, especially in the lower legs, is also a common sign of Beals syndrome.
Less common symptoms of Beals syndrome include heart and eye problems. The most frequent heart problem involves one of the heart valves (mitral valve prolapse) and may necessitate medication prior to dental or other surgeries so as to prevent infection. More serious heart problems may occur but are rare. The aorta, the major blood vessel carrying blood away from the heart, may occasionally enlarge. This condition usually requires medication to prevent further enlargement or rarely, surgery. A small number of individuals with Beals syndrome may also be nearsighted and require eye glasses.
Diagnosis
The diagnosis of Beals syndrome is based on the presence of specific conditions. The diagnosis is suspected in anyone with the typical features of Beals syndrome such as tall, slender stature, contractures of many joints including the elbows, knees, hips, and fingers, abnormal curvature of the spine, decreased muscle bulk, and crumpled ears. As of 2001, a genetic test to confirm a BCA diagnosis has yet to become routinely available. Genetic testing for this syndrome remains limited to a few research laboratories around the world.
Testing during pregnancy (prenatal diagnosis) to determine whether the unborn child of at-risk parents may be affected by BCA is not routinely available. Also, because of the rather mild nature of the condition in most individuals, prenatal diagnosis is usually not requested. There has been at least one documented prenatal diagnosis for Beals syndrome. Using a procedure called amniocentesis, fluid surrounding the developing baby was removed and cells from that fluid were submitted to genetic testing in a research laboratory. The procedure allowed confirmation that the unborn child was affected with Beals syndrome.
Treatment and management
There is no cure for Beals syndrome. Management of the disorder usually involves physiotherapy in early
childhood to increase joint mobility and to lessen the effects of low muscle bulk. The contractures have been known to spontaneously improve, with surgery sometimes required to release them.
The abnormal curvature of the spine tends to worsen with time. A bone specialist should be consulted for advice on the appropriate treatment. Some individuals may require a back brace and/or surgery to correct the curvature.
A heart specialist should be consulted because some individuals with Beals syndrome have been known to have heart defects. Usually, an ultrasound of the heart is taken to assess whether there are any abnormalities. Medications may be used to treat some types of heart problems, if any. An eye specialist should also be consulted because of the possibility of eye problems such as myopia (nearsightedness). Prescription eye glasses may be necessary.
Individuals with Beals syndrome and their families may benefit from genetic counseling for information on the condition and recurrence risks for future pregnancies.
Prognosis
There tends to be gradual improvement in the joint contractures with time. The abnormal spinal curvature tends to get worse over time and may require bracing or surgery. The life span of individuals with Beals syndrome is not altered.
Resources
PERIODICALS
Robinson, Peter N., M. Godfrey. “The molecular genetics of Marfan syndrome and related microfibrillinopathies.”
Journal of Medical Genetics 37(2000): 9-25.
ORGANIZATIONS
AVENUES National Support Group for Arthrogryposis Multiplex Congenita. PO Box 5192, Sonora, CA 95370. (209) 928-3688. avenues@sonnet.com. http://www
.sonnet.com/avenues .
National Marfan Foundation. 382 Main St., Port Washington, NY 11050-3121. (800) 862-7326. http://www.marfan
.org .
National Organization for Rare Disorders (NORD). PO Box 8923, New Fairfield, CT 06812-8923. (203) 746-6518 or (800) 999-6673. Fax: (203) 746-6481. http://www
.rarediseases.org .
OTHER WEBSITES
Godfrey, Maurice. “Congenital Contractural Arachnodactyly.” GeneClinics. Univeristy of Washington, Seattle.http://www.geneclinics.org . (March 6, 2001)
Nada Quercia, Msc, CCGC CGC
syndrome Beals
GALE ENCYCLOPEDIA OF GENETIC DISORDERS |
143 |

Beare-Stevenson cutis gyrata syndrome
Beals-Hecht syndrome see Beals syndrome
Bean syndrome see Blue rubber bleb nevus syndrome
I Beare-Stevenson cutis gyrata syndrome
Definition
Beare-Stevenson Cutis gyrata syndrome is a serious, extremely rare inherited disorder affecting the skin, skull, genitals, navel, and anus. This condition often results in early death.
Description
Beare-Stevenson cutis gyrata syndrome is also known as Beare-Stevenson syndrome and cutis gyrata syndrome of Beare and Stevenson. This very rare inherited disease causes serious physical problems affecting many body parts. Cutis gyrata is characterized by an unusual ridging pattern in the skin resembling corrugation in cardboard. This skin corrugation is present from birth and commonly occurs on the head and arms.
All people with Beare-Stevenson cutis gyrata syndrome are mentally retarded or developmentally delayed. The brain, skull, face, respiratory system, and genitals are often malformed. Death at an early age is common.
Genetic profile
Beare-Stevenson cutis gyrata syndrome is an autosomal dominant disorder, meaning that a person needs a change, or mutation, in only one of two copies of the gene involved to manifest the disorder. As of 2001, all reported cases have been sporadic, or random, occurrences, happening in families with no family history of the disease. This syndrome is associated with mutations in FGFR2, a fibroblast growth factor receptor gene. The fibroblast growth factor receptor genes serve as blueprints for proteins important to inhibition of cell growth during and after embryonic development. FGFR2 is located on human chromosome 10 in an area designated as 10q26.
Demographics
As of 2001, less than 10 cases of Beare-Stevenson cutis gyrata syndrome have been reported. Both males
KEY TERMS
Acanthosis nigricans—A skin condition characterized by darkly pigmented areas of velvety wartlike growths. Acanthosis nigricans usually affects the skin of the armpits, neck, and groin.
Amniocentesis—A procedure performed at 16-18 weeks of pregnancy in which a needle is inserted through a woman’s abdomen into her uterus to draw out a small sample of the amniotic fluid from around the baby. Either the fluid itself or cells from the fluid can be used for a variety of tests to obtain information about genetic disorders and other medical conditions in the fetus.
Autosomal—Relating to any chromosome besides the X and Y sex chromosomes. Human cells contain 22 pairs of autosomes and one pair of sex chromosomes.
Chorionic villus sampling (CVS)—A procedure used for prenatal diagnosis at 10-12 weeks gestation. Under ultrasound guidance a needle is inserted either through the mother’s vagina or abdominal wall and a sample of cells is collected from around the fetus. These cells are then tested for chromosome abnormalities or other genetic diseases.
Sporadic—Isolated or appearing occasionally with no apparent pattern.
and females are affected. The few cases documented in the medical literature suggest that some cases of this disease might be associated with advanced paternal age, or older fathers.
Signs and symptoms
All people with Beare-Stevenson cutis gyrata syndrome are developmentally delayed or mentally retarded. There may be excess fluid on the brain (hydrocephalus), and the nerve connection between the two halves of the brain (the corpus callosum) may be absent or underdeveloped.
A cloverleaf-shaped skull is a very unusual birth abnormality that is common in infants with BeareStevenson cutis gyrata syndrome. Abnormalities in skull shape happen when the sutures (open seams between the bony plates that form the skull) fuse before they typically would. Premature closure of the skull sutures is known as craniosynostosis. Growth of the brain pushes outward
144 |
GALE ENCYCLOPEDIA OF GENETIC DISORDERS |
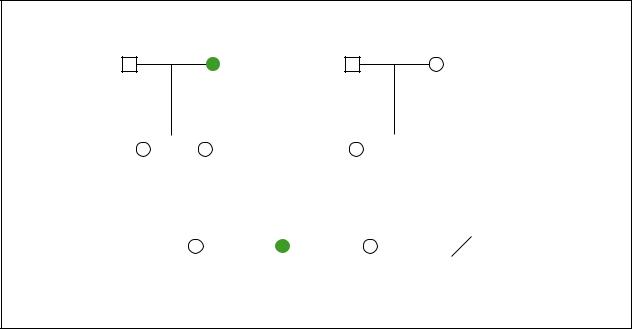
Beare-Stevenson Cutis Gyrata
Cutis gyrata
Craniosynostosis
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
42y |
35y |
||||||||||||
|
|
|
|
|
Craniosynostosis |
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
Wide-set eyes |
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
Developmental delays |
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
Craniosynostosis |
|
|
|
|
|
d.2y |
|||||||
|
|
|
|
|
Protruding eyes |
|
Craniosynostosis, cloverleaf-shaped skull |
|||||||||||
|
|
|
|
|
Cutis gyrata |
|
|
|
Low-set ears |
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
Developmental delays |
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Cutis gyrata |
||||
(Gale Group)
on skull plates that have not yet fused, causing characteristic bulges in those areas.
The characteristic face of someone with BeareStevenson cutis gyrata syndrome has prominent, bulging eyes that slant downward with droopy eyelids. The middle third of the face is underdeveloped and may appear somewhat flattened. The ears are positioned lower and rotated backward from where they would typically be. Skin ridges may be found in front of the ear. Infants with this condition may be born with teeth.
The most recognizable physical symptom of this syndrome is the unusual ridging, or corrugation, of the skin. This cutis gyrata affects the skin on the scalp, face, ears, lips, and limbs and is usually evident at birth. Patches of skin on the armpits, neck, and groin may also display acanthosis nigricans, unusually dark, thickened patches of skin with multiple delicate growths. Skin tags may be present on the surface of the skin and on the tissues lining the mouth. Affected children usually have a prominent navel and may have extra nipples.
People with this disorder may not be able to fully straighten their arms at the elbow. The skin of the palms of the hands and the soles of the feet often show deep ridging. Affected individuals may have small, underdeveloped fingernails.
Children with Beare-Stevenson cutis gyrata syndrome may have breathing problems and narrowing of the roof of the mouth (cleft palate). The anus may be
positioned more forward than normal. The genitals are often malformed and surrounded by corrugated skin. An abnormal stomach valve may cause feeding problems.
Diagnosis
Diagnosis of Beare-Stevenson cutis gyrata syndrome is based on visible hallmark characteristics of the disease. As of 2001, all reported cases have shown hallmark characteristics from birth. DNA testing is available for BeareStevenson cutis gyrata syndrome. This testing is performed on a blood sample to confirm a diagnosis made on physical features. Prenatal genetic testing is also available. Beare-Stevenson cutis gyrata may be suspected in an unborn fetus if a hallmark characteristic, like a cloverleaf skull, is visible on prenatal ultrasound.
Treatment and management
There is no cure for Beare-Stevenson cutis gyrata syndrome. Of less than 10 reported cases in the literature, many died early in life. So few people have been diagnosed with this disease that there is no published information regarding its treatment and management.
Prognosis
Early death is common in people with BeareStevenson cutis gyrata syndrome, especially among those with a cloverleaf skull.
syndrome gyrata cutis Stevenson-Beare
GALE ENCYCLOPEDIA OF GENETIC DISORDERS |
145 |

Beckwith-Wiedemann syndrome
Resources
PERIODICALS
Hall, B. D., et al. “Beare-Stevenson Cutis Gyrata Syndrome.”
American Journal of Medical Genetics 44 (1992): 8289. Krepelova, Anna, et al. “FGFR2 Gene Mutation (Tyr375Cys) in a New Case of Beare-Stevenson Syndrome.” American
Journal of Medical Genetics 76 (1998): 362-64.
ORGANIZATIONS
Children’s Craniofacial Association. PO Box 280297, Dallas, TX 75243-4522. (972) 994-9902 or (800) 535-3643. contactcca@ccakids.com. http://www.ccakids.com .
FACES. The National Craniofacial Assocation. PO Box 11082, Chattanooga, TN 37401. (423) 266-1632 or (800) 3322373. faces@faces-cranio.org. http://www.faces-cranio
.org/ .
WEBSITES
“Cutis Gyrata Syndrome of Beare and Stevenson.” OMIM— Online Mendelian Inheritance in Man. http://www.ncbi
.nlm.nih.gov/entrez/dispomim.cgi?id=123790 .
Judy C. Hawkins, MS
Becker muscular dystrophy see Duchenne muscular dystrophy
I Beckwith-Wiedemann
syndrome
Definition
Beckwith-Wiedemann syndrome (BWS) refers to a disorder of overgrowth. This condition is usually characterized by large body size (macrosomia), large tongue (macroglossia), enlarged internal organs (visceromegaly), the presence of an abdominal wall defect (umbilical hernia or omphalocele), and low blood sugar in the newborn period (neonatal hypoglycemia).
Description
Beckwith and Wiedemann initially described Beckwith-Wiedemann syndrome in the 1960s. It is also known as Wiedemann-Beckwith syndrome and exomphalos macroglossia gigantism syndrome (EMG syndrome).
BWS syndrome will frequently present prenatally with fetal macrosomia, enlarged placentas, and often more than usual amniotic fluid (polyhydramnios) that may lead to premature delivery (a baby being born more than three weeks before its due date). In the first half of pregnancy, the majority of amniotic fluid is made by the
movement of sodium, chloride, and water crossing the amniotic membrane and fetal skin to surround the fetus. During the second half of pregnancy, the majority of amniotic fluid is fetal urine that is produced by the fetal kidneys. Another major source of amniotic fluid is secretion from the fetal respiratory tract. This sterile fluid is not stagnant. It is swallowed and urinated by the fetus constantly and is completely turned over at least once a day. If the fetus has an enlarged tongue (macroglossia), and cannot swallow as usual, this can lead to build-up of excess amniotic fluid. Aside from swallowing difficulties in the newborn, macroglossia can also lead to difficulties with feeding and breathing.
Approximately 75% of infants who have BWS will have an omphalocele. An omphalocele occurs when the absence of abdominal muscles allows the abdominal contents to protrude through the opening in the abdomen. This is covered by a membrane into which the umbilical cord inserts. Omphaloceles are thought to be caused by a disruption of the process of normal body infolding at three to four weeks of fetal development. Although 25% of infants with BWS do not have omphaloceles, they may have other abdominal wall defects such as an umbilical hernia or even a less severe separation of the abdominal muscles, called diastasis recti.
Fifty to sixty percent of newborns with BWS present have low blood sugar levels within the first few days of life. This is called neonatal hypoglycemia and is caused by having more than the usual number of islet cells in the pancreas (pancreatic islet cell hyperplasia). The islet cells of the pancreas produce insulin. This cluster of cells is called the islets of Langerhans and make up about 1% of the pancreas. These cells are the most important sugar (glucose) sensing cells in the body. When an individual eats a meal high in glucose or carbohydrates, this leads to a rise in blood sugar, which is then a signal for the increased insulin secretion by the islet cells of the pancreas. If too much insulin is produced, then the blood glucose levels drop too low. This is called hypoglycemia. Since glucose is the primary fuel for brain function, if hypoglycemia lasts too long, it can lead to brain damage. For this reason, detection and treatment of the hypoglycemia is extremely important. Any child born with features of this syndrome should be carefully monitored for hypoglycemia, especially during the first week of life. Occasionally, onset of hypoglycemia is delayed until the first month after birth. For this reason, the parents of a child with BWS should be taught to watch for the symptoms of hypoglycemia so that they can seek care as soon as possible.
Children with BWS have an increased risk of mortality associated with tumor development. These tumors begin development during fetal life (embryonal tumors).
146 |
GALE ENCYCLOPEDIA OF GENETIC DISORDERS |

These malignant tumors develop in approximately 8% of children who have BWS. The most frequently seen tumors in individuals who have BWS include Wilms tumor (nephroblastoma) and hepatoblastomas. Wilms tumor is a tumor that arises in the kidney and consists of several embryonic tissues. Wilms tumor accounts for 80% of all kidney tumors in children. The peak incidence occurs between two and three years of age, but can be present from infancy to adulthood.
Hepatoblasomas are tumors that arise in the liver during fetal development and is the most common primary liver tumor in infancy and childhood. A wide variety of other tumors, both malignant and benign, are also seen in individuals who have BWS and include, but are not limited to, nervous system tumors (neuroblastomas), adrenal gland tumors, and tumors that commonly occur in the head and neck (rhabdomyosarcoma). The increased risk for tumors appears to be concentrated in the first eight years of life, consistent with the embryonic nature of these tumors. In patients who have BWS, tumor development is not common after age eight.
Hemihyperplasia of a lower extremity or of the whole half of the body can be present. For example, one leg may be longer than the other leg. If hemihyperplasia is present, it may be recognized at birth and may become more or less obvious as a child grows. The risk of tumor development increases significantly when hemihyperplasia is present. While only 13% of affected individuals have hemihyperplasia, 40% of those with neoplasms have hyperplasia. Most patients with BWS remain at or above the 95th percentile for length through adolescence. Advanced bone age can be identified on x ray examination. Growth rate usually slows down at around age seven or eight. After nine years of age, the average weight remains between the 75th and 95th percentile. Although height, weight, skeletal, and dental maturity may be above average for years, growth rate gradually slows down and eventually children reach average height and normal proportions. Puberty occurs at a usual time.
Another feature includes unusual linear grooves within the ear lobes and/or a groove or pit on the top of the outer ear. Facial characteristics may include prominent eyes (exophthalmos), “stork bite” birth marks (telangiectatic nevi) of the upper half of the face, and “port wine stain” birth marks (facial nevus flammeus) on the face.
Genetic profile
The genetics of BWS is complex. Approximately 85% of individuals who have BWS have no family history of BWS and have a normal karyotype. Of these patients, approximately 20% have paternal uniparental
KEY TERMS
Amniocentesis—A procedure performed at 16-18 weeks of pregnancy in which a needle is inserted through a woman’s abdomen into her uterus to draw out a small sample of the amniotic fluid from around the baby. Either the fluid itself or cells from the fluid can be used for a variety of tests to obtain information about genetic disorders and other medical conditions in the fetus.
Chorionic villus sampling (CVS)—A procedure used for prenatal diagnosis at 10-12 weeks gestation. Under ultrasound guidance a needle is inserted either through the mother’s vagina or abdominal wall and a sample of cells is collected from around the fetus. These cells are then tested for chromosome abnormalities or other genetic diseases.
Hemihyperplasia—A condition in which overdevelopment or excessive growth of one half of a specific organ or body part on only one side of the body occurs.
Neonatal—Neonatal refers to the first 28 days after birth.
Nevus flammeus—A flat blood vessel tumor present at birth, also known as a “port wine stain.”
disomy for chromosome 11p15. Uniparental disomy occurs when an individual receives two copies of a chromosome, part of a chromosome, or a gene from one parent, as opposed to receiving one copy from each parent. In this situation, the amount of gene expression can be changed and cause a disease or disorder. Approximately 5-10% of patients who have no family history and a normal karyotype have a gene change identified near 11p15, called p57(KIP2). This gene region, p57(KIP2), is a tumor supressor region, meaning that its presence suppresses tumor development, but that the loss of a normally functioning region could lead to tumor development and potentially lead to BWS. The IGF-2 (insulin-like growth factor-2) gene is also in this region. Both uniparental disomy and a gene mutation result in dosage changes of the normal functioning genes, resulting in overexpression and subsequently increased growth and tumor risk. When a gene change in the p57(KIP2) region is found in either of the parents of the affected child, the chance for a future child to have BWS could be as high as 50% with each future pregnancy. The remaining 70% of individuals who have BWS, no family history, and a normal karyotype have no identifiable cause
syndrome Wiedemann-Beckwith
GALE ENCYCLOPEDIA OF GENETIC DISORDERS |
147 |
