
- •ICU Protocols
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1: Airway Management
- •Suggested Reading
- •2: Acute Respiratory Failure
- •Suggested Reading
- •Suggested Reading
- •Website
- •4: Basic Mechanical Ventilation
- •Suggested Reading
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Websites
- •7: Weaning
- •Suggested Reading
- •8: Massive Hemoptysis
- •Suggested Reading
- •9: Pulmonary Thromboembolism
- •Suggested Reading
- •Suggested Reading
- •Websites
- •11: Ventilator-Associated Pneumonia
- •Suggested Readings
- •12: Pleural Diseases
- •Suggested Reading
- •Websites
- •13: Sleep-Disordered Breathing
- •Suggested Reading
- •Websites
- •14: Oxygen Therapy
- •Suggested Reading
- •15: Pulse Oximetry and Capnography
- •Conclusion
- •Suggested Reading
- •Websites
- •16: Hemodynamic Monitoring
- •Suggested Reading
- •Websites
- •17: Echocardiography
- •Suggested Readings
- •Websites
- •Suggested Reading
- •Websites
- •19: Cardiorespiratory Arrest
- •Suggested Reading
- •Websites
- •20: Cardiogenic Shock
- •Suggested Reading
- •21: Acute Heart Failure
- •Suggested Reading
- •22: Cardiac Arrhythmias
- •Suggested Reading
- •Website
- •23: Acute Coronary Syndromes
- •Suggested Reading
- •Website
- •Suggested Reading
- •25: Aortic Dissection
- •Suggested Reading
- •26: Cerebrovascular Accident
- •Suggested Reading
- •Websites
- •27: Subarachnoid Hemorrhage
- •Suggested Reading
- •Websites
- •28: Status Epilepticus
- •Suggested Reading
- •29: Acute Flaccid Paralysis
- •Suggested Readings
- •30: Coma
- •Suggested Reading
- •Suggested Reading
- •Websites
- •32: Acute Febrile Encephalopathy
- •Suggested Reading
- •33: Sedation and Analgesia
- •Suggested Reading
- •Websites
- •34: Brain Death
- •Suggested Reading
- •Websites
- •35: Upper Gastrointestinal Bleeding
- •Suggested Reading
- •36: Lower Gastrointestinal Bleeding
- •Suggested Reading
- •37: Acute Diarrhea
- •Suggested Reading
- •38: Acute Abdominal Distension
- •Suggested Reading
- •39: Intra-abdominal Hypertension
- •Suggested Reading
- •Website
- •40: Acute Pancreatitis
- •Suggested Reading
- •Website
- •41: Acute Liver Failure
- •Suggested Reading
- •Suggested Reading
- •Websites
- •43: Nutrition Support
- •Suggested Reading
- •44: Acute Renal Failure
- •Suggested Reading
- •Websites
- •45: Renal Replacement Therapy
- •Suggested Reading
- •Website
- •46: Managing a Patient on Dialysis
- •Suggested Reading
- •Websites
- •47: Drug Dosing
- •Suggested Reading
- •Websites
- •48: General Measures of Infection Control
- •Suggested Reading
- •Websites
- •49: Antibiotic Stewardship
- •Suggested Reading
- •Website
- •50: Septic Shock
- •Suggested Reading
- •51: Severe Tropical Infections
- •Suggested Reading
- •Websites
- •52: New-Onset Fever
- •Suggested Reading
- •Websites
- •53: Fungal Infections
- •Suggested Reading
- •Suggested Reading
- •Website
- •55: Hyponatremia
- •Suggested Reading
- •56: Hypernatremia
- •Suggested Reading
- •57: Hypokalemia and Hyperkalemia
- •57.1 Hyperkalemia
- •Suggested Reading
- •Website
- •58: Arterial Blood Gases
- •Suggested Reading
- •Websites
- •59: Diabetic Emergencies
- •59.1 Hyperglycemic Emergencies
- •59.2 Hypoglycemia
- •Suggested Reading
- •60: Glycemic Control in the ICU
- •Suggested Reading
- •61: Transfusion Practices and Complications
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Website
- •63: Onco-emergencies
- •63.1 Hypercalcemia
- •63.2 ECG Changes in Hypercalcemia
- •63.3 Superior Vena Cava Syndrome
- •63.4 Malignant Spinal Cord Compression
- •Suggested Reading
- •64: General Management of Trauma
- •Suggested Reading
- •65: Severe Head and Spinal Cord Injury
- •Suggested Reading
- •Websites
- •66: Torso Trauma
- •Suggested Reading
- •Websites
- •67: Burn Management
- •Suggested Reading
- •68: General Poisoning Management
- •Suggested Reading
- •69: Syndromic Approach to Poisoning
- •Suggested Reading
- •Websites
- •70: Drug Abuse
- •Suggested Reading
- •71: Snakebite
- •Suggested Reading
- •72: Heat Stroke and Hypothermia
- •72.1 Heat Stroke
- •72.2 Hypothermia
- •Suggested Reading
- •73: Jaundice in Pregnancy
- •Suggested Reading
- •Suggested Reading
- •75: Severe Preeclampsia
- •Suggested Reading
- •76: General Issues in Perioperative Care
- •Suggested Reading
- •Web Site
- •77.1 Cardiac Surgery
- •77.2 Thoracic Surgery
- •77.3 Neurosurgery
- •Suggested Reading
- •78: Initial Assessment and Resuscitation
- •Suggested Reading
- •79: Comprehensive ICU Care
- •Suggested Reading
- •Website
- •80: Quality Control
- •Suggested Reading
- •Websites
- •81: Ethical Principles in End-of-Life Care
- •Suggested Reading
- •82: ICU Organization and Training
- •Suggested Reading
- •Website
- •83: Transportation of Critically Ill Patients
- •83.1 Intrahospital Transport
- •83.2 Interhospital Transport
- •Suggested Reading
- •84: Scoring Systems
- •Suggested Reading
- •Websites
- •85: Mechanical Ventilation
- •Suggested Reading
- •86: Acute Severe Asthma
- •Suggested Reading
- •87: Status Epilepticus
- •Suggested Reading
- •88: Severe Sepsis and Septic Shock
- •Suggested Reading
- •89: Acute Intracranial Hypertension
- •Suggested Reading
- •90: Multiorgan Failure
- •90.1 Concurrent Management of Hepatic Dysfunction
- •Suggested Readings
- •91: Central Line Placement
- •Suggested Reading
- •92: Arterial Catheterization
- •Suggested Reading
- •93: Pulmonary Artery Catheterization
- •Suggested Reading
- •Website
- •Suggested Reading
- •95: Temporary Pacemaker Insertion
- •Suggested Reading
- •96: Percutaneous Tracheostomy
- •Suggested Reading
- •97: Thoracentesis
- •Suggested Reading
- •98: Chest Tube Placement
- •Suggested Reading
- •99: Pericardiocentesis
- •Suggested Reading
- •100: Lumbar Puncture
- •Suggested Reading
- •Website
- •101: Intra-aortic Balloon Pump
- •Suggested Reading
- •Appendices
- •Appendix A
- •Appendix B
- •Common ICU Formulae
- •Appendix C
- •Appendix D: Syllabus for ICU Training
- •Index

504 |
A. Kulkarni and V. Agarwal |
|
|
•It should be used cautiously in patients with renal impairment. It has many drug interactions and may cause skin hypersensitivity reactions.
•Febuxostat may be used if the patient is hypersensitive to allopurinol.
Step 7: Consider rasburicase (recombinant urate oxidase)
•Urate oxidase—present in most mammals, but not in humans—oxidizes preformed uric acid to allantoin, which is 5 to 10 times more soluble than uric acid in acid urine.
•When exogenous urate oxidase (uricase, rasburicase) is administered, serum and urinary uric acid levels decrease markedly within approximately 4 h.
•This should be used especially if the uric acid level is above 8 mg/dL.
•Uric acid levels should be monitored regularly to adjust dosing.
•Rasburicase degrades uric acid within the blood samples at room temperature, thus interfering with accurate measurement.
•Therefore, samples should immediately be placed on ice until the completion of assay.
Step 8: Treat associated electrolyte disorders
•Hyperkalemia—hemodialysis may be needed if renal insufficiency or volume overload is present.
•Hypocalcemia—if asymptomatic, no therapy is required.
•Hyperphosphatemia—restrict phosphate intake and increase loss with phosphate binders such as aluminum hydroxide or calcium carbonate, sevelamer hydroxide, and lanthanum carbonate.
Step 9: Consider hemodialysis
•This modality should be considered in specific situation such as:
–Volume overload
–Uric acid of more than 10 mg/dL despite rasburicase
–Uncontrolled hyperkalemia and hyperphosphatemia
–Renal failure (Table 63.2)
63.3Superior Vena Cava Syndrome
A 19-year-old patient with lymphoma presented with dyspnea, swelling of the head and the neck, and upper limbs, and distended veins on the neck and the upper chest.
Step 1: Resuscitate
•Compression of the tracheobronchial tree causing airway compromise is an airway emergency, needing intubation (with a small endotracheal tube) and ventilation till definitive treatment (refer to Chap. 78)
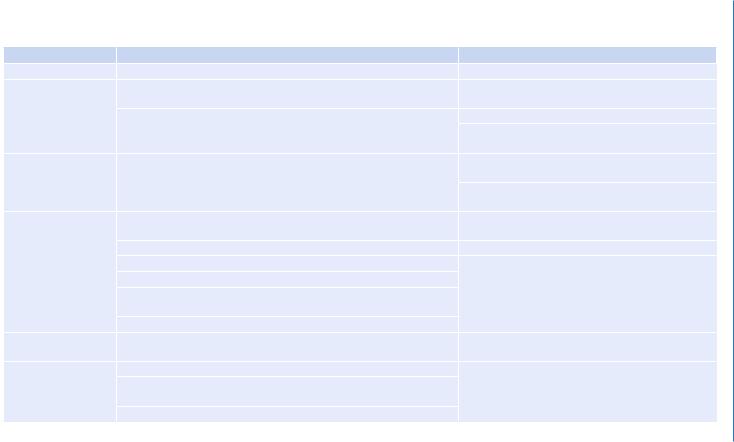
Table 63.2 Treatment for tumor lysis syndrome |
|
|
Intervention |
Dosage |
Comment |
Fluids |
3 L/m2/day (200 mL/kg/day if £10 kg) |
Exercise caution if congestive heart failure |
Allopurinol |
Oral dose: 50–100 mg/m2 every 8 h orally (maximum 300 mg/m2/day) or |
6-Mercaptopurine, azathioprine, cyclophosphamide, |
|
10 mg/kg/day divided every 8 h (maximum 800 mg/day) |
and methotrexate require dose reduction |
|
IV: 200–400 mg/m2/day in 1–3 divided doses (maximum 600 mg/day) |
Renal impairment—50% dose reduction |
|
|
Drug interaction with thiazide diuretics, ampicillin/ |
|
|
amoxicillin |
Rasburicase |
IV infusion 0.1–0.2 mg/kg/day in 50 mL normal saline over 30 min, for |
Contraindicated in glucose-6-phosphate dehydrogenase |
|
5 days |
deficiency |
|
|
Adverse reactions—anaphylaxis, rash, hemolysis, and |
|
|
methemoglobinemia |
Hyperkalemia |
Calcium gluconate: 10 ml of 10% solution or calcium chloride (5–10 ml |
ECG monitoring |
|
of 10% solution) by slow IV infusion for life-threatening arrhythmias |
|
|
Albuterol nebulizer |
Avoid PR route in neutropenics |
|
Regular insulin: 0.1 U/kg IV + 25% D (2 mL/kg) IV |
Sodium bicarbonate and calcium not to be administered |
|
Sodium bicarbonate: 1–2 mEq/kg IV, push only if pH <7.2 |
through the same line |
|
Sodium polystyrene sulfonate: 1 gm/kg/day in 1–4 doses with 50% |
|
|
sorbitol PO/PR |
|
|
Dialysis: if severe |
|
Hypocalcemia |
Calcium gluconate: 10 ml of 10% solution IV administered slowly or |
ECG monitoring |
|
calcium chloride |
|
Hyperphosphatemia |
Hydration |
Limit aluminum hydroxide use to 1–2 days to avoid |
|
Aluminum hydroxide: 50–150 mg/kg/day in divided doses PO or |
cumulative aluminum toxicity |
|
nasogastrically every 6 h |
|
|
Dialysis: if severe |
|
emergencies-Onco 63
505

506 |
A. Kulkarni and V. Agarwal |
|
|
Step 2: Do imaging
•Computed tomography (CT) scan of chest with or without venography is diagnostic
•These patients may not be able to lie supine for CT chest
•They have to be intubated prior to CT or empirical therapy needs to be started
•Upper extremity venogram or duplex ultrasound for patients with a central venous catheter in upper extremity to exclude venous thrombus.
Step 3: Confirm diagnosis
•Obtain biopsies before instituting therapy if diagnosis is uncertain
Proper hemostatic measures should be taken while performing invasive
procedures
Step 4: Chemotherapy and corticosteroids
• These can be used, especially in tumors that are chemosensitive
Step 5: Radiotherapy
•This is a standard treatment modality for sensitive tumors but may take a few weeks to show effect
Step 6: Stenting of the superior vena cava
•It has been shown to be effective and feasible in relieving the symptoms of superior vena cava syndrome
63.4Malignant Spinal Cord Compression
A 68-year-old patient with carcinoma of prostrate developed worsening back pain progressively with radiating pain down the right leg associated with weakness and difficulty in walking and loss of bladder and bowel function.
Step 1: Resuscitate (see Chap. 78)
(a)Pain relief with adequate analgesics is a priority in these patients.
(b)Urgent neurosurgical, radiotherapy, oncology consultation for limb salvage is necessary.
(c)Special precaution needs to be taken while transporting these patients.
Step 2: Do imaging
•In patient with high index of suspicion and symptoms suggestive of metastatic bone disease, magnetic resonance imaging is gold standard for diagnosis.
•Alternative is CT scan of spine.
•It is important to image the entire spine as more than one area of compression may be present.

63 Onco-emergencies |
507 |
|
|
Step 3: Start glucocorticoids
(a)Dexamethasone is indicated in patients with motor deficits or radiologic evidence of neural compression.
(b)It is given as an initial intravenous dose of 10–16 mg followed by 4 mg every 4 h.
(c)This is later administered orally and tapered over 10–12 days.
(d)Use proton pump inhibitors or H2 blockers along with high dose of corticosteroids.
Step 4: Consider radiation therapy
•This has been the mainstay of the treatment in patients with and without motor deficit.
•This is usually combined with surgery for spine stabilization.
Step 5: Consider surgery
•It is indicated in most cases, especially in patients with a good performance status. Indications are the following:
–Gross instability of the spine
–Rapidly progressive symptoms
–Progressive symptoms during radiation therapy
–When tissue for diagnosis is needed
–Radioresistant tumors
Step 6: Consider chemohormonal therapy
•Hormonal chemotherapy and zoledronic acid should be considered in sensitive tumors such as prostate cancer, testicular tumor, or lymphoma.
Suggested Reading
1.Coiffier B, Altman A, Pui CH, Younes A, Cairo MS. Guidelines for the management of pediatric and adult tumor lysis syndrome: an evidence-based review. J Clin Oncol. 2008;26:2767–78.
2.Halfdanarson TR, Hogan WJ, Moynihan TJ. Oncologic emergencies: diagnosis and treatment. Mayo Clin Proc. 2006;81(6):835–48. www.mayoclinicproceedings.com.
This review covers the complete spectrum of oncologic emergencies with their etiopathogenesis and initial therapy, a must read for those caring for cancer patients. It does not require subscription.
3.Abrahm JL. Assessment and treatment of patients with malignant spinal cord compression. J Support Oncol. 2004;2:377–401.
A very comprehensive evidence-based review on malignant spinal cord compression.

Part IX
Trauma and Burn
M.C. Mishra and Prasad Rajhans
