
Essentials of Orthopedic Surgery, third edition / 01-Basic Science of Bone and Cartilage Metabolism
.pdf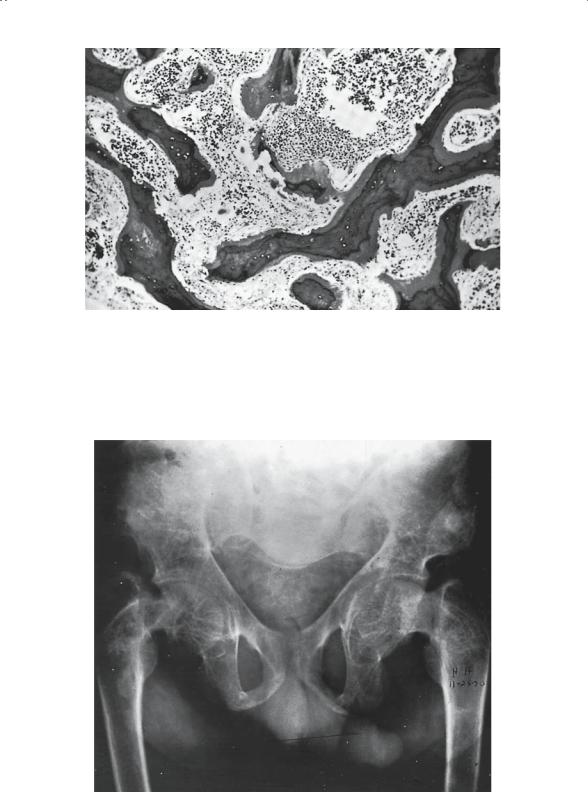
FIGURE 1-17. Renal osteodystrophy. Histologic section of bone exhibiting wide osteoid seams. These seams are seen in patients with primary renal disease, but they are not present in patients with primary hyperparathyroidism because the osteoid produced in primary hyperparathyroidism is normal. (From Bogumill GP. Orthopaedic Pathology: A Synopsis with Clinical Radiographic Correlation. Philadelphia: Saunders, 1984. Reprinted by permission.)
21
22 J.N. Delahay
Sick Cell Syndromes: Osteogenesis Imperfecta
and Osteopetrosis
The underlying mechanism seen in these conditions is a qualitative, functional deficit in a specific cell population, despite the fact that the population is quantitatively normal.
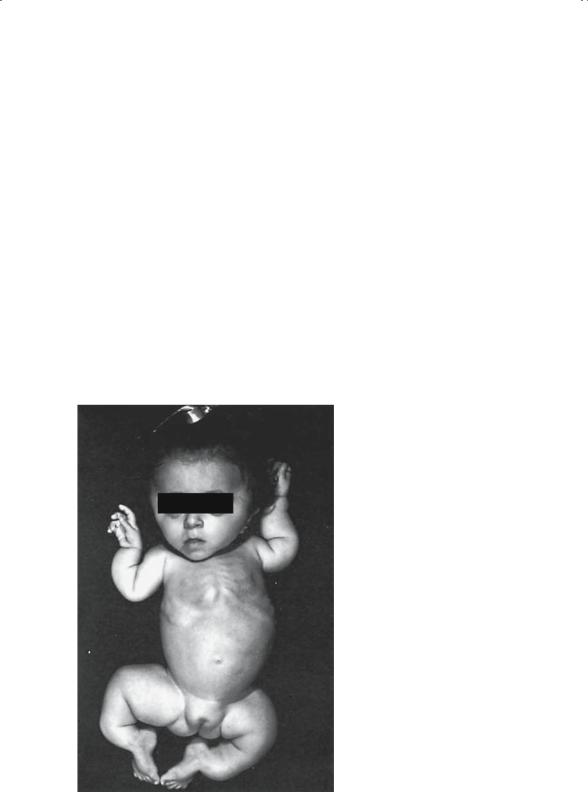
Osteogenesis imperfecta (Fig. 1-19) is typified by the impotence of the osteoblasts; they are unable to manufacture and secrete normal collagen. Ossification is, therefore, abnormal and results in inferior-quality bone.
Clinically and radiographically, there is marked cortical thinning and attenuation of the diaphyseal caliber. The long bones, because of their altered anatomy, are at very high risk for fracture (Fig. 1-20). This bone fragility is the hallmark feature of osteogenesis imperfecta.
Because osteogenesis imperfecta is caused by a genetic mutation in the normal coding for type I collagen, there is significant phenotypic heterogeneity. In an effort to accommodate the variations in phenotype, the Sillence classification has been adopted by most authors. Four specific types are described in this classification:
FIGURE 1-19. Deformity in a child with severe osteogenesis imperfecta. Note the prominence of the ribs in the abnormally shaped thoracic cage, the flattening of the skull with frontal bulging, and the malformed ribs. (From Gertner JM, Root L. Osteogenesis imperfecta. Orthop Clin North Am 1990;21(1):153. Reprinted by permission.)

1. Basic Science of Bone and Cartilage Metabolism |
23 |
FIGURE 1-20. Radiograph of the lower extremities of a child with osteogenesis imperfecta. The bones are slender and the cortices excessively thin; both femurs have incurred fractures that are partially healed, although deformity still exists. (From Jowsey J. Metabolic Diseases of Bone. Philadelphia: Saunders, 1977. Reprinted by permission.)
Type I is the most common form and the mildest clinically, it is transmitted as an autosomal dominant. These patients demonstrate the classic findings of blue sclera, long bone fractures after the age of walking, and a relatively normal life expectancy.
Type II is the lethal form of the disease. These children are usually stillborn or die shortly after birth, usually as a result of respiratory failure or intracranial hemorrhage.
Type III is the severe nonlethal form, characterized by sclera of normal color, multiple birth fractures, and significant long-term deformity and disability.
Type IV is the intermediate form, with variable manifestations, and is the least common.
Osteopetrosis is similarly considered a sick cell syndrome resulting from the failure of the osteoclasts to remove primary spongiosa bone. This latter osseous material then “piles up” in the skeleton, making it appear very dense radiographically (Fig. 1-21). Despite the fact that the bones look extremely dense and, indeed, lack a medullary canal, they are biomechanically very weak, which results in frequent pathologic fractures. An additional complication is the displacement of marrow elements from the long bones, resulting in a myelophisthic anemia; this in turn generates extramedullary hematopoiesis and the clinical finding of hepatosplenomegaly, usually seen in these patients.
Paget’s Disease
Sir James Paget described a syndrome of unknown etiology that bears his name. The initial description referred to the condition as “ostetitis defor-

24 J.N. Delahay
FIGURE 1-21. Radiologic appearance of the femurs and pelvic girdle of a patient with osteopetrosis. There is almost complete absence of the marrow cavity and lack of remodeling of the femoral neck and acetabulum. (From Jowsey J. Metabolic Diseases of Bone. Philadelphia: Saunders, 1977. Reprinted by permission.)
mans.” The syndrome is most common in individuals of European descent and in patients typically over the age of 55. Men tend to be more affected than women.
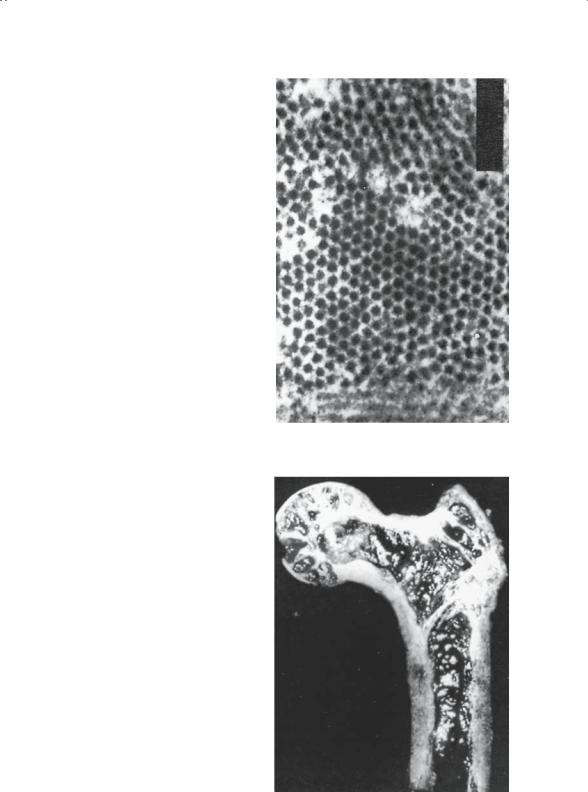
There is strong evidence, specifically the finding of radiodense viral-like particles in the osteoclasts (Fig. 1-22), pointing to a slow virus as the cause of Paget’s disease. It is basically a disease of bone turnover wherein bone formation and bone resorption dramatically increase. The two processes occur alternately rather than simultaneously in any given bone. The net effect is bones of increased density with marked trabecular thickening (Fig. 1-23). The skull, pelvis, spine, tibia, and femur are the favorite targets of this process. Sadly, and not unlike osteopetrosis, the pagetic bones are mechanically weak, making pathologic fracture a frequent complication. Despite the presence of abundant quantities of bone, the bone is poorly formed and the mineral and matrix are poorly integrated. Bone pain, spinal stenosis, and hearing defects resulting from disease in the skull base compromising the eighth nerve are frequent problems in these patients.
Several different therapeutic approaches have been attempted. Currently, bisphosphonates and calcitonin are frequently employed therapeutic agents. Similarly as in osteoporosis, they are used in an attempt to inhibit bone resorption and also to a lesser degree to block bone mineralization. The rationale is to “freeze the skeleton” and thereby decrease bone
1. Basic Science of Bone and Cartilage Metabolism |
25 |
FIGURE 1-22. Viral particles located in osteoclasts within pagetoid bone have been implicated as a causal factor in Paget’s disease. (From Merkow RL, Lane JM. Paget’s disease of bone. Orthop Clin North Am 1990;21(1):172. Reprinted by permission.)
FIGURE 1-23. Example of pagetoid bone demonstrating deformity and thickening of the cortex of the hip. The neck shaft angle has developed varus deformity. (From Merkow RL, Lane JM. Paget’s disease of bone. Orthop Clin North Am 1990;21(1):172. Reprinted by permission.)

26 J.N. Delahay
turnover. Cyclic treatment regimens are currently being employed in hopes of allowing new bone to become mineralized while decreasing the osteoclastic activity. The serum alkaline phosphatase level provides a reliable way of monitoring the response to treatment because it is elevated in the presence of active bone turnover.
Arthritis
Because any significant discussion on this subject is well beyond the scope of this chapter, it is hoped that presentation of some basic concepts will allow consideration of this diagnosis in the scheme of differential diagnosis. It is important to recall that a diarthrodial joint includes three tissues: bone, cartilage, and synovium. Each of the arthritic diseases tends to impact one of these tissues, with changes in the other two resulting as secondary phenomena. The radiographic and microscopic changes encountered represent a composite of the result of the initial injury and the organism’s attempt at repair of that injury.
Noninflammatory Arthritis: Osteoarthritis
Osteoarthritis can be primary or secondary, if one considers the degenerative joint disease that can follow trauma or other primary events. The process itself targets the articular cartilage. Whether the initial event is mechanical or biochemical remains controversial. The net result is progressive damage to the articular surface. The secondary bone changes that occur are reparative in nature. Joint space narrowing, subchondral sclerosis, osteophytes, and subchondral cysts, therefore, are the classic radiographic changes. Because this is most typically a disease of weight-bearing joints, the hip and knee are the joints that usually require orthopedic care. Total joint arthroplasty has become the mainstay of surgical management in these patients, producing reliable long-term results.
Inflammatory Arthritis: Rheumatoid Arthritis
Rheumatoid arthritis, and to some degree its variants, target the synovial membrane as the site for the immunologic process that is the root mechanism of this disease. As the synovium hosts this inflammatory process, it becomes hyperplastic and hypertrophic. The thickened synovium destroys the articular cartilage by enzymatic degradation and destroys the underlying bone by pressure necrosis and erosion (Fig. 1-24). In contrast to osteoarthritis, repair changes are, for the most part, abortive. The radiograph reflects this overall atrophic process. Soft tissue swelling, osteopenia on both sides of the joint, and bone erosions are the standard findings (Fig. 1-25). Joint destruction is generally symmetrical and much more global than with osteoarthritis. Extensive alterations in normal anatomy usually necessitate multiple joint arthroplasties.

FIGURE 1-24. Diagram (A) and section (B) of a finger joint of a patient with rheumatoid arthritis. The marked synovitis is evident in the synovial recesses with erosions into the bone on both sides of the articular surface (long curved arrows). The pannus is beginning to encroach on margins of the joint (short arrows). Although the cartilage retains its normal appearance in the center of the joint, the proteoglycan structure is affected by the altered synovial fluid. It is susceptible to rapid removal by wear and tear as well as by the encroaching pannus. Because the pannus grows in from the margins, the earliest radiographic erosions are seen at the margins, and the contract surfaces are spared until relatively late. (From Bogumill GP. Orthopaedic Pathology: A Synopsis with Clinical Radiographic Correlation. Philadelphia: Saunders, 1984. Reprinted by permission.)

28 J.N. Delahay
FIGURE 1-25. Radiograph of both hands of a patient with long-standing rheumatic arthritis. Osteoporosis in all bones is marked. The wrist joints show advanced destruction. There is dislocation of the metacarpophalangeal joints of all fingers. Steroid therapy causes expansion of metacarpals and phalanges secondary to changes in the marrow fat (steroid lipomatosis). (From Bogumill GP. Orthopaedic Pathology: A Synopsis with Clinical Radiographic Correlation. Philadelphia: Saunders, 1984. Reprinted by permission.)
Metabolic Arthritides: Crystalline Arthropathy
The common denominator of the metabolic arthritides is the deposition of crystals or metabolic by-products in or around joints. Destructive changes in these joints necessitate rheumatologic and frequently orthopedic care.
In gout, sodium urate crystals are deposited in and around the joints. Finding these crystals in joint fluid is the diagnostic sine qua non of this metabolic imbalance. An intense chemical synovitis and bony erosions can occur. Typically, the first metatarsophalangeal joint is the classic site, but certainly the process can present in any joint, including the spine. The acute onset and signs of acute inflammation should suggest the diagnosis, which is best confirmed by arthrocentesis. The finding of needle-like, negatively birefringent crystals under polarized light confirms the diagnosis. The treatment is usually medical. However, in the presence of late destructive changes, surgical intervention can be considered.
Pseudogout is one of the many causes of chondrocalcinosis and should not be considered synonymous with it. The presence of weakly positively
1. Basic Science of Bone and Cartilage Metabolism |
29 |
birefringent crystals, rhomboid in shape, attests to the diagnosis. The calcium pyrophosphate crystals are radiopaque and, as such, can be viewed on standard radiographs as calcification of cartilage, including the menisci and articular surfaces. The condition rarely mandates surgical intervention, and treatment frequently revolves around nonsteroidal antiinflammatory drugs or intraarticular steroid injections.
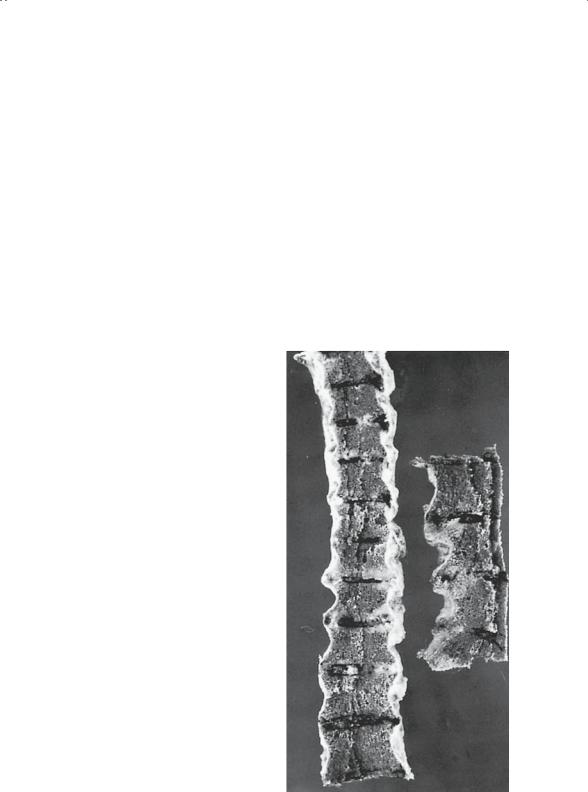
Ochronosis is an inborn error of metabolism. The error is an absence of homogentisic acid oxidase. As a result, homogentisic acid accumulates and targets articular cartilage for its deposition. The articular cartilage is stiffened by the presence of this by-product and loses its resiliency. The net result is fissuring and fibrillation of the articular surface; these changes radiographically and pathologically mimic osteoarthritis. The unique feature of this condition is the fact that this material pigments and stains the cartilage black (Fig. 1-26), thereby accounting for the blackish tinge of the earlobes and the tip of the nose seen in these patients.
FIGURE 1-26. Gross appearance of vertebral bodies in a patient with ochronosis. Notice the diminution of the intervertebral disks, black discoloration of the cartilage components, virtual disappearance of all joint spaces, and bony bridging. (From Bogumill GP. Orthopaedic Pathology: A Synopsis with Clinical Radiographic Correlation. Philadelphia: Saunders, 1984. Reprinted by permission.)
30 J.N. Delahay
Vascular Disease
This diagnostic category is a somewhat diverse grouping of clinical entities that are best considered under this heading lest they be overlooked.
Circulatory Disease: Avascular Necrosis
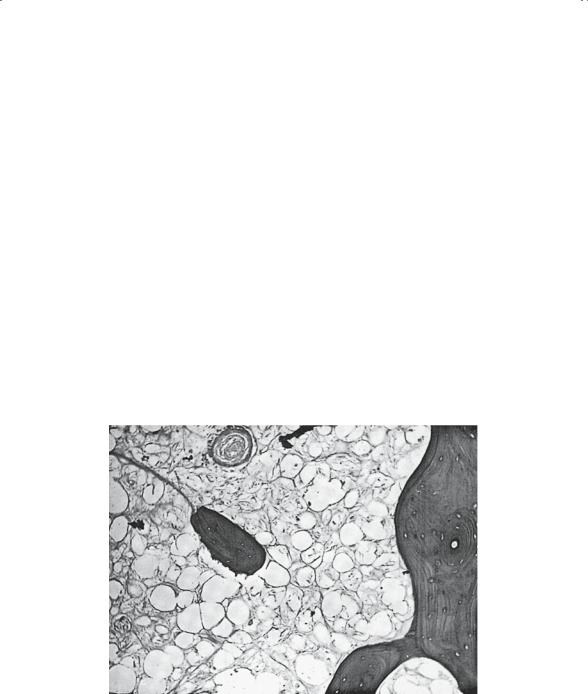
Afflictions of the vascular tree, especially the arterial side, tend to produce similar lesions in bone, despite the etiology. Bone deprived of a portion of its blood supply becomes necrotic, as do all other tissues (Fig. 1-27). Depending on the extent of the vascular involvement, the infarcts can range from small areas of bony necrosis in the metaphysis (Fig. 1-28), which are clinically inconsequential, to extensive involvement at the ends of the long bones that progresses to significant degenerative joint disease.
The radiographic appearance of dead bone is essentially that of sclerosis. In truth, the dead tissue is incapable of changing its density because no viable cells exist. Rather, the viable bone adjacent to the necrotic
FIGURE 1-27. Bone from central area of infarction, exhibiting infarcted fatty tissue, obliterated vessels, and infarcted bone. Note absence of either osteoclastic or osteoblastic activity. The trabeculae in this zone have retained their original density. (From Bogumill GP. Orthopaedic Pathology: A Synopsis with Clinical Radiographic Correlation. Philadelphia: Saunders, 1984. Reprinted by permission.)
