
Essentials of Orthopedic Surgery, third edition / 06-Sports Medicine
.pdf
6
Sports Medicine
JOHN J. KLIMKIEWICZ
The emphasis presently placed on physical fitness in society in terms of overall health is at an all-time high. Participation in both organized and recreational sports has escalated during the past several decades as a result. This increase in participation has lead to an emphasis on treating injuries associated with sporting activities. The advances within medicine regarding the diagnosis of these injuries, such as magnetic resonance imaging (MRI), as well as arthroscopy for their treatment, has improved results only to focus more attention within this field. A number of skilled physicians and other health professionals have developed interests regarding the specific care of athletes. The goal of sports medicine as a subspecialty is the prevention of injury, diagnosis and treatment of athletic injury, and returning athletes to preinjury activity with no acute or long-term sequelae. The purpose of this chapter is to focus on the biologic tissues involved in sporting injuries, highlighting the patterns in which they are injured. An overview then follows regarding the evaluation and treatment principles as they relate to the management of athletes and sport-specific injuries.
Patterns of Injuries
Injuries within the field of sports medicine can be generally classified into one of two categories: microtrauma and macrotrauma. Microtraumatic injuries are those that typically are associated with overuse injury by the athlete, such as many of the tendonopathies or stress fractures that are common in long-distance runners. Microtraumatic injuries are the result of repetitive stresses leading to structural breakdown of the tissue in question. Macrotrauma, on the other hand, involves a single traumatic episode resulting in injury to a specific region. A downhill skier fracturing the tibia, or a soccer player cutting and injuring the anterior cruciate ligament, are two examples of macrotraumatic injury. In these instances the force imparted to a specific tissue is greater than that tissue is able to withstand, resulting in catastrophic mechanical failure of that tissue.
257

258 J.J. Klimkiewicz
Musculoskeletal Tissues
Tendons
Tendons are strong, inextensible tissue that attach muscle to bone. They are composed of closely packed, well-aligned collagen bundles within a matrix of proteoglycan. Fibroblasts are the predominant cell type and are arranged in parallel orientation between the bundles of collagen fibers.
The tendon fibroblasts act to produce both collagen and proteoglycan within the tendon unit. Collagen is a major constituent of tendon. Type I collagen comprises 86% of a healthy tendon’s dry weight, whereas type III is found in lesser amounts. It is the high concentration of collagen in combination with its parallel orientation that gives tendons their high tensile strength. Collagen chains are linked together to form fibrils that in turn are bound together by a proteoglygan matrix to form a fascicle, the primary unit in tendon structure. Fascicles in turn are bound by the endotenon, a layer of elastin-containing loose connective tissue that supports the blood, lymphatic, and neural supply to the tendon unit. It is the endotenon that is contiguous with both the muscle fibers and periosteum at the musculotendinous and tendoosseous junctions, respectively.
Acute tendon injuries may be direct, occurring as a result of laceration or contusion, or indirect, occurring secondary to tensile overload. Both are examples of macrotrauma. Tensile overload is a common injury within the field of sports medicine (i.e., patellar tendon, Achilles tendon ruptures). In the majority of these cases, because most tendons can withstand tensile forces greater than can be exerted by their muscular or bony attachments, avulsion fractures and muscle tendon junction ruptures are far more common than midsubstance ruptures of tendon.
Chronic tendon overload represents the classic microtraumatic injury in sports medicine. These injuries occur at the sites of high exposure to repetitive tensile overload. Examples can be found in Table 6-1. Whether inflammation has a role in the early stages of these overuse injuries is unclear. However, in cases that are not responsive to short periods of rest with persistence of symptoms, similar findings can be seen histologically, reflecting a more-degenerative process. Disruption of collagen fibrils, hyaline degeneration, and proliferation of vasculature are classic in these entities, termed angioplastic fibroplasias, and result in a tendonosis or breakdown of the corresponding tendinous unit. At this stage it is clear that this is not an inflammatory process, as no acute or chronic inflammatory infiltrates are demonstrable on these histologic specimens. Tendonosis is also observed in cases of spontaneous rupture and may be clinically silent until rupture occurs. An example is an Achilles tendon rupture seen in middle-aged athletes participating in strenuous sports.

6. Sports Medicine |
259 |
TABLE 6-1. Common sites of sports-related tendon overload.
Site of injury |
Sport |
Achilles tendon |
Running |
Iliotibial band |
|
Flexor hallicus longus tendon |
Dancing |
Patellar tendon |
Basketball, volleyball |
Quadriceps tendon |
|
Supraspinatus tendon |
Swimming, softball, baseball, golf, racquet |
Extensor carpi radialis brevis tendon |
sports |
Flexor pronator origin |
|
Abductor pollicus longus tendon |
Rowing |
Extensor pollicus brevis tendon |
|
|
|
Ligaments
Ligaments are short bands of connective tissue that serve to connect two osseous structures. Similar to tendons, these are very organized hierarchical structures with high tensile strength. Ligaments are likewise composed of bundles of type I collagen fibers, which make up approximately 70% of its dry weight. Small amounts of elastin are combined with fibroblasts in a complex extracellular matrix. This collagen matrix comprises a series of fibers forming a subfasicular unit. Multiple subfascicular units are then bound together to form a fasciculus. These fasiciculi can in turn be oriented in a simple longitudinal fashion, such as the medial collateral ligament of the knee, or can spiral to form a more-helical structure, such as the anterior and posterior cruciate ligaments of the knee.
At their attachments to bone, the transition from ligament to bone occurs gradually in a series of distinct phases. These phases range from ligament to fibrocartilage, from fibrocartilage to mineralized fibrocartilage, and from mineralized fibrocartilage to bone. The size of each zone varies from ligament to ligament and is related to its structural properties. Collagen fibers, known as Sharpey’s fibers, run in continuity throughout this zone of transition and have an important role in securing the ligament to bone. Although somewhat similar to tendons in their microscopic organization and composition, ligaments and tendons are structurally and biochemically different. Ligaments contain a lower percentage of collagen and a higher percentage of extracellular matrix. There is also a more-random alignment of collagen fibers than their tendinous counterparts.
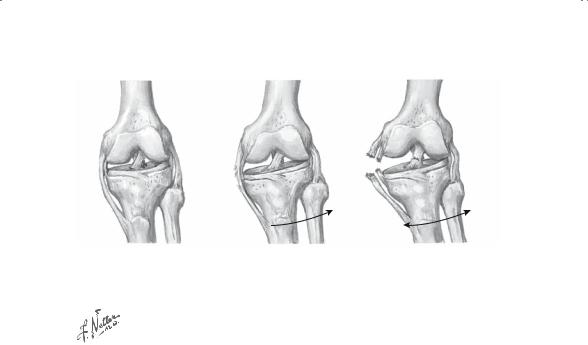
In contrast to injuries to tendons that can be both acute and chronic processes, ligamentous injuries occur as a result of acute trauma and represent a macrotraumatic process. When a stress is applied to a ligament, a sprain occurs, whose severity (grades I–III) depends on the amount of stress applied (Fig. 6-1). A grade I sprain represents the least traumatic episode when some ligamentous fibers are torn on a microscopic level. Structural integrity of the ligament however is maintained. An example of
260 J.J. Klimkiewicz
1st-degree sprain. Localized joint pain and tenderness but no joint laxity
2nd-degree sprain. |
3rd-degree sprain. Complete |
Detectable joint laxity plus |
disruption of ligaments |
localized pain and |
and gross joint instability |
tenderness |
|
FIGURE 6-1. Classification of ligamentous injuries (sprains). (Netter images reprinted with permission from Elsevier. All rights reserved.)
this is a common ankle sprain where traditionally the anterior talofibular ligament is injured. In a grade II sprain, some fibers are macroscopically torn in combination with microscopic damage resulting in a stretching of the ligament. Although the biomechanical properties of the ligament are compromised in this scenario, some structural integrity of the ligament remains. An example of this injury is an injury to the medial collateral ligament to the knee. On application of a valgus force the knee demonstrates increased laxity as compared to the other side, but an endpoint is present to the ligament, signifying some integrity to this structure remains. In a grade III sprain, the ligament structure fails, with no structural integrity of the ligament remaining. After rupture of the anterior cruciate ligament, there is both an increase in anterior translation when an anterior force is applied to the tibia and a nonexistent endpoint; this represents a complete failure.
Intraand extraarticular ligaments differ in their response to acute trauma; this is influenced by a difference in the local vascular supply of these entities, as well as the degree of the injury, and whether a significant gap forms between the two ends of ligamentous rupture. Typically, extraarticular ligaments have a high potential for healing and gradually heal with predominantly type I collagen within 6 to 12 weeks. Maturation of this ligament scar can take up to 1 year in some cases despite histologic evidence of healing as early as 6 weeks. Contrastingly, intraarticular ligaments such as the anterior cruciate ligament have a poor healing potential. In

6. Sports Medicine |
261 |
cases of complete disruption of this structure, dissociation of the midsubstance “mop ends” results in significant gap formation with inhibition of the healing process. These differences result in different treatment approaches to these injuries, as extraarticular ligamentous injuries are frequently treated conservatively whereas intraarticular injuries are typically treated surgically secondary to a poor healing response.
Muscle
Injuries of skeletal muscle and the musculotendinous junction commonly lead to prolonged clinical disability. Muscle strains alone account for up to 50% of injuries in particular sports.
Active force generation within muscle depends on its contractile apparatus. The contractile apparatus is composed of actin and myosin myofilaments that are arranged into functional units called sarcomeres. Muscle contraction consists of an energy-dependent process of cross-bridge unlinking and advancement of the myofilaments within the sarcomere. Either aerobic or anaerobic processes provide cellular energy for this process. Muscle fibers may be characterized by their capacity for aerobic respiration. Oxidative (red) fibers are characterized by sustained, slow contractions, whereas glycolytic (white) fibers contract rapidly under anaerobic conditions. Fiber type composition varies significantly between muscular groups and among different individuals. The force of muscle contraction is directly related to its cross-sectional area, which is reflective of its number of parallel contractile elements.
Muscular injury can result from direct mechanical deformations that occur in muscular strains, contusions, and lacerations or indirect mechanisms such as vasculature or neurologic injury as is seen in the cases of acute and chronic (exercise-induced) compartment syndromes.
Muscular strains involve either partial or complete disruption of the muscle–tendon unit; this represents a macrotraumatic process. Clinical and experimental observations suggest that most muscular strain injuries involve the muscle–tendon junction. Common examples involve hamstring and adductor strains surrounding the hip, which usually occur with passive stretch or with lengthening during muscular contraction (eccentric contraction). Complete injuries are often associated with muscle retraction, hematoma formation, and local inflammation, while lesser-degree strains involve more microscopic failure. Functional recovery is dependent on the coordinated specific repair of the contractile elements with their surrounding connective tissues and neurovascular structures. This process can take up to 6 months in some cases. After injury, individual muscular fibers may contract normally after repair and regeneration, but whole muscle contractile function rarely is normal after gross skeletal muscular injury.
Less common are muscular contusions that are a result of direct trauma. In these cases, such as a quadriceps contusion, skeletal muscle damage

262 J.J. Klimkiewicz
results from nonpenetrating sudden high-energy force directed to the muscular group in question. These forces can result in the temporary or permanent loss of vascular and neurologic function secondary to direct trauma imparted to the musculature. These injuries are often characterized by a large associated hematoma. Ultimate recovery is often related to the magnitude of original injury. A relatively infrequent complication of this is myositis ossificans. In this case, normal mesenchymal cells involved in the healing process differentiate into osteoblasts, resulting in the formation of bone. This abnormal bone often results in a prominence in the injured area, with subsequent symptoms.
Articular Cartilage
Often associated with trauma surrounding a particular joint are injuries and more long-term degeneration of the articular cartilage. When diffuse and occurring over a period of time, this process can result in osteoarthritis (microtrauma); however, there is an additional subset of these injuries that are more focal and result from a direct injury, often referred to as osteochondral injuries (macrotrauma). Although highly desirable, functional restoration of injury to articular cartilage remains one of the most challenging of orthopedic problems with the sports medicine field.
Articular cartilage composition and thickness varies from joint to joint and is directly age dependent. The tissue typically is composed of 75% to 80% water and dense extracellular matrix consisting of 50% to 75% type II collagen and 15% to 30% proteoglycan macromolecules. Water and proteoglycans make up its extracellular matrix. A remarkable characteristic if articular cartilage is its acellularity, as chondrocytes occupy less than 10% of this tissue. These cells maintain the extracellular matrix and aid in cellular homeostasis. The collagen provides tensile strength to articular cartilage while the proteoglycans and extracellualr matrix provide its more important compressive role.
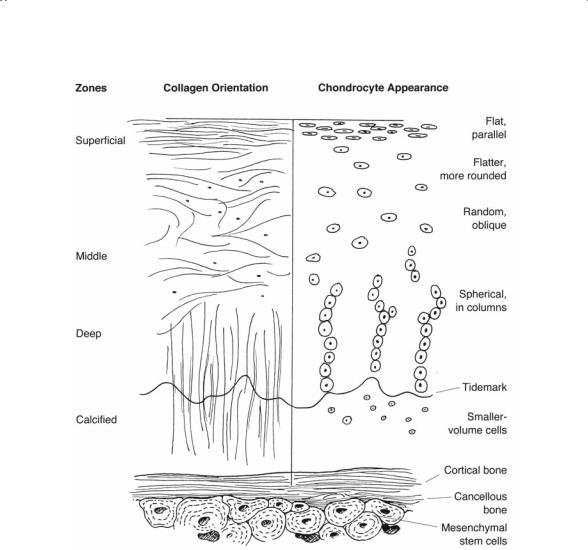
Structurally, articular cartilage is highly organized into four zones of depth from the articular surface to the underlying subchondral bone (Fig. 6-2). Zone 1, also called the superficial layer, makes up approximately 10% of cartilage, determines its load-bearing ability, and serves as a gliding surface. Within this layer chondrocytes are arranged with collagen fibers are parallel to the joint surface to provide high tensile strength and stiffness. Zone 2 is a transitional layer and is composed of chondrocytes and randomly oriented collagen fibers. It has a higher concentration of proteoglycan and lower concentration of collagen as compared to Zone 1. Zone 3 or the deep layer is composed of collagen fibers and clusters of chondrocytes oriented perpendicular to the underlying subchondral plate, providing compressive strength. Zone 4, the calcified layer, acts to join the deep zone of uncalcified cartilage to the subchondral bone. There are few cells within this layer. It contains the tidemark adjacent to the subchondral bone.
6. Sports Medicine |
263 |
FIGURE 6-2. Morphology of articular cartilage. (From Browne JE, Branch TP. Surgical alternatives for treatment of articular cartilage lesions. Copyright 2000 American Academy of Orthopaedic Surgeons. Reprinted from the Journal of the American Academy of Orthopaedic Surgeons, Volume 8 (3), pp. 180–189 with permission.)
Articular cartilage is an avascular as well as aneural tissue. As an avascular tissue it exchanges gases, nutrients, and waste products through a process of diffusion through tissue fluid or synovium. This poor blood supply results in poor reparative capability in the event of acute injury or chronic wear.
Injuries to articular cartilage are best described by the Outerbridge classification system (Fig. 6-3). This system characterizes the injury to articular cartilage based on its qualitative appearance at the time of surgery: grade I, softening with swelling; grade II, fragmentation and fissuring; grade III,

264 J.J. Klimkiewicz
FIGURE 6-3. Outerbridge classification. (From Browne JE, Branch TP. Surgical alternatives for treatment of articular cartilage lesions. Journal of the American Academy of Orthopaedic Surgeons 2000;8:180–189. Reprinted by permission.)
fragmentation and fissuring down to subchondral bone; grade IV, exposed subchondral bone. Grade I/II lesions are thought to involve superficial injury and are best left untreated while grade III/IV lesions represent fullthickness cartilaginous injuries and are best treated surgically.
Meniscus
The meniscus of the knee is formed of a combination of fibrocartilage with some proteoglycan. The collagen fibers are type I and are arranged in a predominantly circumferential orientation. It is this orientation that gives this tissue its unique loading characteristics and function within the knee. This highly structured network provides the ability of the meniscus to allow the compressive forces of joint loading to be dissipated circumferentially along these parallel collagen fibers, termed hoop stresses. The meniscus biomechanically transmits a compressive force to one that is tensile in nature and absorbed within the meniscus. Injury to the meniscus results in a decreased ability to perform its function, resulting in higher compressive forces being transmitted across the knee joint.

6. Sports Medicine |
265 |
Similar to articular cartilage, the vascularity of the meniscus is poor. Only the peripheral one-third of the meniscus receives a blood supply, and therefore the potential for healing after injury is limited. Location and type of meniscal tearing in a symptomatic knee determine one’s ability for potential healing. Meniscal injuries are best categorized by the location of the tear as well as the morphology of the tear. The location can be best described in reference to the blood supply of the meniscus. Red–red tears involve the peripheral one-third of the meniscus and have excellent healing potential. Red–white tears involve a zone of the meniscus with good blood supply on the peripheral aspect of the tear and poor blood supply on the more-central portion and have intermediate healing potential. White–white tears involve those tears in the avascular zone completely with poor healing potential. Morphologic classification of meniscal tears is demonstrated in Fig. 6-4.
A Vertical Longitudinal |
|
B Oblique |
|
C Degenerative |
|
|
|
|
|
|
|
|
|
|
D Transverse (Radial) |
E Horizontal |
FIGURE 6-4. Morphology of meniscus tears. (From Fu FH, Harner CD, Vince KG (eds) Knee Surgery, vol 1. Philadelphia: Williams & Wilkins, 1994. Reprinted by permission.)

266 J.J. Klimkiewicz
Evaluation of Common Sports Medicine Injuries
The principles involved in the initial evaluation of the injured athlete focus on history and physical examination in combination with auxiliary tests and are similar in comparison to other orthopedic injuries. This subspecialty differs from that of a general orthopedic setting in two distinct manners. One large difference in the management of the athlete is the ability to provide prompt “on-the-field” attention as a result of game time coverage by the sports medicine physician; this allows one to often visualize the injury directly and distinguish as to whether the mechanism was a direct result of blunt trauma as compared to a more-indirect mechanism (i.e., cutting injury). Additionally, it provides one with a golden window of time to evaluate the injury before the effects of swelling and subsequent pain and spasm complicate the physical exam. It often allows one the opportunity to make the diagnosis without the need for auxiliary tests that are often required when evaluating these injuries on a more-subacute basis. Furthermore, the sports medicine physician is often asked the safety of returning to play in light of a specific injury. Knowledge of the common injuries as well as the sporting activities themselves is important in making these decisions. The following sections focus on the history as well as physical examination in the sports medicine setting. Specifics regarding the injuries are elaborated in their respective chapters.
History
The history in many sporting injuries is straightforward and related to acute trauma. Examples include twisting the ankle when coming down for a rebound, feeling the shoulder “pop out” when being tackled, or hearing a “pop” within one’s knee on cutting cross-field. Important in this history is the mechanism of injury, as this often relates very closely with the structure injured. When this is more ambiguous on questioning the athlete, input from other players, trainers, and coaches as well as game-time film can be invaluable in determining the mechanism of injury. Other injuries within this field are a result of microtrauma, or overuse, and have no specific mechanism of injury. Examples can include plantar fasciitis of the foot or shin splints. For these insidious conditions, its important to obtain the specifics of recent activity including change in recent activity, change in shoe wear or other equipment, the surface involved (track to road, flat surface to hills, etc.). Other pertinent details include whether this problem has occurred before, and if so, how it happened, what type of treatment was rendered, and what was the outcome. Previous problems may alert the clinician to a different treatment problem to prevent recurrence of the injury. Examples include the management of “first-time” as opposed to recurrent shoulder dislocations.
