
- •VOLUME 3
- •CONTRIBUTOR LIST
- •PREFACE
- •LIST OF ARTICLES
- •ABBREVIATIONS AND ACRONYMS
- •CONVERSION FACTORS AND UNIT SYMBOLS
- •EDUCATION, COMPUTERS IN.
- •ELECTROANALGESIA, SYSTEMIC
- •ELECTROCARDIOGRAPHY, COMPUTERS IN
- •ELECTROCONVULSIVE THERAPHY
- •ELECTRODES.
- •ELECTROENCEPHALOGRAPHY
- •ELECTROGASTROGRAM
- •ELECTROMAGNETIC FLOWMETER.
- •ELECTROMYOGRAPHY
- •ELECTRON MICROSCOPY.
- •ELECTRONEUROGRAPHY
- •ELECTROPHORESIS
- •ELECTROPHYSIOLOGY
- •ELECTRORETINOGRAPHY
- •ELECTROSHOCK THERAPY.
- •ELECTROSTIMULATION OF SPINAL CORD.
- •ELECTROSURGICAL UNIT (ESU)
- •EMERGENCY MEDICAL CARE.
- •ENDOSCOPES
- •ENGINEERED TISSUE
- •ENVIRONMENTAL CONTROL
- •EQUIPMENT ACQUISITION
- •EQUIPMENT MAINTENANCE, BIOMEDICAL
- •ERGONOMICS.
- •ESOPHAGEAL MANOMETRY
- •EVENT-RELATED POTENTIALS.
- •EVOKED POTENTIALS
- •EXERCISE FITNESS, BIOMECHANICS OF.
- •EXERCISE, THERAPEUTIC.
- •EXERCISE STRESS TESTING
- •EYE MOVEMENT, MEASUREMENT TECHNIQUES FOR
- •FETAL MONITORING
- •FETAL SURGERY.
- •FEVER THERAPY.
- •FIBER OPTICS IN MEDICINE
- •FICK TECHNIQUE.
- •FITNESS TECHNOLOGY.
- •FIXATION OF ORTHOPEDIC PROSTHESES.
- •FLAME ATOMIC EMISSON SPECTROMETRY AND ATOMIC ABSORPTION SPECTROMETRY
- •FLAME PHOTOMETRY.
- •FLOWMETERS
- •FLOWMETERS, RESPIRATORY.
- •FLUORESCENCE MEASUREMENTS
- •FLUORESCENCE MICROSCOPY.
- •FLUORESCENCE SPECTROSCOPY.
- •FLUORIMETRY.
- •FRACTURE, ELECTRICAL TREATMENT OF.
- •FUNCTIONAL ELECTRICAL STIMULATION
- •GAMMA CAMERA.
- •GAMMA KNIFE
- •GAS AND VACUUM SYSTEMS, CENTRALLY PIPED MEDICAL
- •GAS EXCHANGE.
- •GASTROINTESTINAL HEMORRHAGE
- •GEL FILTRATION CHROMATOGRAPHY.
- •GLUCOSE SENSORS
- •HBO THERAPY.
- •HEARING IMPAIRMENT.
- •HEART RATE, FETAL, MONITORING OF.
- •HEART VALVE PROSTHESES
- •HEART VALVE PROSTHESES, IN VITRO FLOW DYNAMICS OF
- •HEART VALVES, PROSTHETIC
- •HEART VIBRATION.
- •HEART, ARTIFICIAL
- •HEART–LUNG MACHINES
- •HEAT AND COLD, THERAPEUTIC
- •HEAVY ION RADIOTHERAPY.
- •HEMODYNAMICS
- •HEMODYNAMIC MONITORING.
- •HIGH FREQUENCY VENTILATION
- •HIP JOINTS, ARTIFICIAL
- •HIP REPLACEMENT, TOTAL.
- •HOLTER MONITORING.
- •HOME HEALTH CARE DEVICES
- •HOSPITAL SAFETY PROGRAM.
- •HUMAN FACTORS IN MEDICAL DEVICES
- •HUMAN SPINE, BIOMECHANICS OF
536 HUMAN FACTORS IN MEDICAL DEVICES
BIBLIOGRAPHY
Cited References
1.Geddes LA, Whistler SJ. The error in indirect blood pressure measurement with in correct size of cuff. Am Heart 1978; 96(July):4–8.
2.Sapinski A, Hetmanska ST. Standard algorithm of bloodpressure measurement by the oscillometric method. Med Biol Eng Comput 1992;30:671.
3.For example, Zsofia N, Katalin M, Gygorgy D. Evaluation of the Tensioday ambulatory blood pressure monitor according to the protocols of the British Hypertension Society and the Association for the Advancement of Medical Instrumentation. Blood Press Monit 2002;7:191–197.
4.O’Brien E, Atkins N, Staessen J. State of the market: a review of ambulatory blood pressure monitoring devices. Hypertension 1995;26:835–842.
5.Chen W, Kobayashi T, Ichikawa S, Takeuchi Y, Togawa T. Continuous estimation of systolic pressure using the pulse arrival time and intermittent calibration. Med Biol Eng Comput 2000;38:569–574.
6.Ishijima M. Monitoring of electrocardiograms in bed without utilizing body surface electrodes. IEEE Trans Biomed Eng BME 1993;40:593–594.
7.Ishijima M, Togawa T. Observation of electrocardiogram through tap water. Clin Phys Physiol Meas 1989;10:171–175.
8.Tamura T, et al. Unconstrained heart rate monito ring during bathing. Biomed Instrum Technol 1997;31:391–396.
9.Amoateng-Adjepong Y, Mundo JD, Manthous CA. Accuracy of an infrared tympanic thermometer.Chest 1999;115:1002–1005.
10.Robinson JL, Jou H, Spady DW. Accuracy of parents in measuring body temperature with a tympanic thermometer. BMC Family Pract. 2005;6:3.
11.Khan M, et al. Multi-dimension applications of bioelectrical impedance analysis. JEP Online 2005;8(1):56–71.
12.Segal KR, et al. Estimation of human body composition by electrical impedance methods. A comparison study. J Appl Physiol 1985;58:1565–1571.
13.Conway JM, Noms KH, Bodwell CE. A new approach for the estimation of body composition: infrared interactance. Am J Clin Nutr 1984;40:1123–1130.
14.Maruo K, Tsurugi M, Tamura M, Ozaki Y. In vivo noninvasive measurement of blood glucose by near-infrared diffuse-reflectance spectroscopy. Appl Spectrosc 2003;57(10): 1236–1244.
15.Malin SF, et al. Noninvasive prediction of glucose by nearinfrared diffuse reflectance spectroscopy. Clin Chem 1999; 45:1651–1658.
16.Tuomisto T, Pentika¨inen V. Personal health monitor for homes. ERCIM News 1997;29.
17.Yamakoshi K. Unconstrained physiological monitoring in daily living for healthcare. Frontiers Med Biol Eng 2000; 10:239–259.
18.Stevens J, et al. The effect of age on the association between body-mass index and mortality. N Engl J Med 1998;338:1–7.
19.Williamson D, et al. Comparison of digital photography to weighed and visual estimation of portion sizes. J Am Diet Assoc 2003;103:1139–1111.
20.Wang DH, Kogashiwa M, Ohta S, Kira S. Validity and reliability of a dietary assessment method: the application of a digital camera with a mobile phone card attachment. J Nutr Sci Vitaminol (Tokyo) 2002;48:498–504.
21.Tharion WJ, et al. Total energy expenditure estimated using a foot-contact pedometer. Med Sci Monit 2004;10(9):CR504–509.
22.Perrin O, Terrier P, Ladetto Q, Merminod B, Schutz Y. Improvement of walking speed prediction by accelerometry
and altimetry, validated by satellite positioning. Med Biol Eng Comput 2000;38(2):164–168.
23.Celler BG, et al. Remote monitoring of health status of the elderly at home. A multidisciplinary project on aging at the University of New South Wales. Intern J Bio-Medical Comput 1995;40:144–155.
24.Suzuki R, Ogawa M, Tobimatsu Y, Iwaya T. Time course action analysis of daily life investigation in the welfare techo house in Mizusawa. J Telemed Telecare 2001;7:249–259.
25.Ohta S, Nakamoto H, Shinagawa Y, Tanikawa T. A health monitoring system for elderly people living alone. J Telemed Telecare 2002;8:151–156.
26.Sadeh A, Hauri PJ, Kripke DF, Lavie P. The role of actigraphy in the evaluation of the sleep disorders. Sleep 1995;18: 288–302.
27.Salmi T, Partinen M, Hyyppa M, Kronholm E. Automatic analysis of static charge sensitive bed (SCSB) recordings in the evaluation of sleep-related apneas. Acta Neurol Scand 1986;74:360–364.
28.Salmi T, Sovijarvi AR, Brander P, Piirila P. Long-term recording and automatic analysis of cough using filtered acoustic signals and movements on static charge sensitive bed. Chest 1988;94:970–975.
29.Sjoholm TT, Polo OJ, Alihanka JM. Sleep movements in teethgrinders. J Craniomandib Disord 1992;6:184–191.
30.Tamura T, et al. Assessment of bed temperature monitoring for detecting body movement during sleep: comparison with simultaneous video image recording and actigraphy. Med Eng Phys 1999;21:1–8.
31.Lu L, Tamura T, Togawa T. Detection of body movements during sleep by monitoring of bed temperature. Physiol Meas 1999;20:137–148.
32.Milledge JS, Stott FD. Inductive plethysmography--a new respiratory transducer. J Physiol 1977;267:4P–5P.
33.Sackner JD, et al. Non-invasive measurement of ventilation during exercise using a respiratory inductive plethysmograph. I Am Rev Respir Dis 1980;122:867–871.
34.Mendelson Y, Ochs BD. Noninvasive pulse oximetry utilizing skin reflectance. IEEE Trans Biomed Eng 1988;35:798–805.
35.Rhee S, Yang BH, Asada HH. Artifact-resistant powerefficient design of fingerring plethysmographic sensors. IEEE Trans Biomed Eng 2001;48:795–805.
See also HUMAN FACTORS IN MEDICAL DEVICES; MOBILITY AIDS; NUTRITION, PARENTERAL; QUALITY-OF-LIFE MEASURES, CLINICAL SIGNIFICANCE OF; TEMPERATURE MONITORING; TRANSCUTANEOUS ELECTRICAL NERVE STIMULATION (TENS).
HOSPITAL SAFETY PROGRAM. See SAFETY
PROGRAM, HOSPITAL.
HUMAN FACTORS IN MEDICAL DEVICES
DANIEL W. REPPERGER
Wright-Patterson Air Force Base
Dayton, Ohio
INTRODUCTION
The human factors issues related to the use and design of medical devices has experienced significant paradigm shifts since this topic was addressed > 20 years ago (1). Not only has the technology innovation of the Internet

vastly affected how medical professionals both gather and report information, but also standards are now more easily established. In addition, technology in the healthcare industry has concomitantly made significant advances. The evolving characteristics of legal liability with medical devices have also changed. Concurrently, the skill and sophistication of users with computer-aided systems has significantly improved with more tolerance and acceptance of automation. The computer and microprocessor-based medical devices are now the pervasive means of humans dealing with mechanical–electrical systems. First, it is important to define the term Human Factors within the context of medical devices and biomedical engineering. The phrase human factors can be broadly characterized as the application of the scientific knowledge of human capabilities and limitations to the design of systems and equipment to generate products with the most efficient, safe, effective, and reliable operation. A modern expression to describe a systematic procedure to evaluate risk when humans use medical devices is termed human factors engineering (2). The U.S Food and Drug Administration (FDA) is a strong proponent of the use of human factors engineering to manage risk, in particular with application to medical devices. The responsibility of the FDA is to guarantee the safety and efficacy of drugs and medical devices. Since, in the United States, the FDA is one of the leading authorities on medical standards, it is worthwhile to review (3,4) their interpretation on how human factors studies should be conducted with medical device use as perceived by this group. Other U.S. government organizations, such as the National Institute of Health (NIH) (5) and the Agency for Health Care Research and Quality (6), also offer their perspective on the application of human factors studies with respect to the manipulation of medical devices. Other sources of government information are found at (7–12). Also available online are a number of legal sources (13–15) related to injury issues and instrumentation affiliated with healthcare and how they perceive the relevance of human factors engineering. In these sources, there is a strong influence on how human factors procedures have some bearing on liability, abuse, misuse, and other troublesome issues associated with medical devices (16).
From an historical perspective, in the late 1980s, data collected by the FDA demonstrated that almost one-half of all medical device recalls resulted from design flaws. In 1990, the U.S. Congress passed the Safe Medical Devices Act, giving the FDA the ability to mandate good manufacturing practices. These practices involve design controls for manufacturers to use human factors engineering principles within medical device design.
In this article, we initially discuss human factors as defined by the FDA followed by three classic case studies. The ramifications of legal issues are then presented. Concurrent good human factors methods are then described, followed by some key topic areas including alarms, labeling, automation, and reporting. Future issues regarding human factors and medical devices are subsequently offered with conclusions and future directions of this field depicted.
First, it is instructive to review the present state of affairs on how the FDA defines human factors engineering
HUMAN FACTORS IN MEDICAL DEVICES |
537 |
within the context of when humans interact with medical devices. The term human factors engineering is a persuasive term in the literature describing present FDA standards.
A HUMAN FACTORS ENGINEERING PERSPECTIVE FROM THE FDA
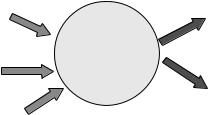
The goal of the FDA is to promote medical device designers to develop highly reliable devices. Human factors engineering is a phrase used to help understand and optimize how people employ and interact with technology. A host of literature describes human factors engineering in many eclectic areas (17–30). When medical devices fail or malfunction, this impacts patients, family members, and professional healthcare providers. A common term used to characterize the potential source of harm is a hazard. A hazard may arise in the use of a medical device due to the inherent risk of medical treatment, from device failures (malfunctions) and also from device use. Figure 1, from the FDA, displays possible sources of device failure hazards that impact the human factors issues in medical devices. Figure 1 may be deceptive in the presumption that equal hazards exist between use related and device failure. More correctly (3,4) the use contribution to the total medical devices hazards may far exceed those from the device failures. In fact, from an Institute of Medicine report (31), as many as 98,000 people die in any given year from medical errors that occur in hospitals. This is more than the number who die from motor vehicle accidents, breast cancer, or acquired immune deficiency syndrome (AIDS). A proportion of these errors may not directly be attributed to the medical device itself; however, the importance of incorporating human factors engineering principles into the early design and use of these important interfaces is a key concern. It is instructive to examine the two major types of errors (hazards) in Fig. 1 and how they are delineated. Risk analysis will refer to managing the forms of risks to be described herein. After the hazards are first clarified, the goal is for the hazards to be mitigated or controlled by modifying the device user interface (e.g., control or display characteristics, logic of operation, labeling) or the background of the users employing the device (training, limiting the use to qualified users). The power in the human factors approach is to help identify, understand, and address use-related problems as well as the original design problem with the physical device itself prior to its acceptance in the workplace of the healthcare professional. Some institutions have now developed in-house usability laboratories, in order to rigorously test any medical device
Figure 1. Hazards from device failure and use related.
538 HUMAN FACTORS IN MEDICAL DEVICES
Environment |
Safe and effective |
|
|
factors |
outcome |
|
How the |
User factors |
device is |
|
|
|
used |
Unsafe or
Physical
ineffective
device factors
outcome
Figure 2. Human factors consideration in medical device use.
before utilization. It is worthwhile to first elaborate on use related hazards as they are relevant in this area.
Use-Related Hazards
Addressing the hazards related to device use, the essential components include (1) device users (patient, caregiver, physician, family member, etc.); (2) typical and atypical device use; (3) characteristics of the environment for the application of the medical device; and (4) the interaction between users, devices, and use environments.
Figure 2 portrays an abstraction on all possible uses for a medical device.
Device Failure Hazards
When understanding hazards from the perspective of risk analysis, it is common to consider the following classes of hazards as they pertain to device design: (1) chemical hazards (e.g., toxic chemicals); (2) mechanical hazards (e.g., kinetic or potential energy from a moving object); (3) thermal hazards (high temperature components); (4) electrical hazards (electric shock, electromagnetic interference); (5) radiation hazards (ionizing and nonionizing); and (6) biological hazards (allergic reactions, bioincompatibility, and infection).
In an effort to address good human factors design when dealing with medical devices, it is instructive to now discuss three classic misadventures in the medical device arena when human factors procedures could have been modified to preclude untoward events. One usually thinks of medical errors occurring, for example, in surgery (wrong site surgery), as the amputation of the wrong appendage (32,33) or from chemotherapy overdoses (34). In 2005, it is now a common practice, in holding areas before surgery, for the surgeon and medical team to discuss with the patient the impending surgery and to have the patient mark on his body precisely where the surgery will be performed with a magic marker. This procedure assures the patient that no confusion may occur as a function of a patient mix-up, after the patient is under anesthesia. Three examples are now presented of untoward events that could have been prevented with improved human factors use methodologies. In the final analysis, the enemy of safety is complexity, which appears in these case studies. Complex systems fail because of the contribution of multiple small failures, each individual failure may be insufficient to cause an accident, but in combination, the results may be tragic.
EXAMPLES OF CASE STUDIES WHERE HUMAN FACTORS ISSUES ARISE
It is worthwhile to examine a few classic case studies where human factors procedures interacting with medical devices needed to be reevaluated. It is emphasized that the errors described herein may not be attributed to any one person or system. Rather, the complex interaction of humans with poorly defined procedures involving certain medical devices has given rise to events, which were not planned or expected. However, with a more structured interaction of humans with these systems, improved results could be obtained. The reference by Geddes (35) provides many interesting examples where enhanced human factors planning would have prevented errors in medical treatment.
Case Study 1 from Ref. 35 and Reported in the South African
Cape Times (1996)
‘‘For several months, our nurses have been baffled to find a dead patient in the same bed every Friday morning’’ a spokeswoman for the Pelonomi Hospital (Free State, South Africa) told reporters. ‘‘There was no apparent cause for any of the deaths, and extensive checks on the air conditioning system, and a search for possible bacterial infection, failed to reveal any clues.’’
Although device failure could cause such deaths, why they occurred on Fridays is difficult to understand? The Cape Times later reported:
It seems that every Friday morning a cleaner woman would enter the ward, remove the plug that powered the patient’s life support system, plug her floor polisher into the vacant socket and then go about her business. When she had finished her chores, she would then replug the life support machine and leave, unaware that the patient was now dead. She could not, after all, hear the screams and eventual death rattle over the shirring of her polisher.
‘‘We are sorry, and have sent a strong letter to the cleaner in question. Further, the Free State Health and Welfare Department is arranging for an electrician to fit an extra socket, so there should be no repetition of this incident. The inquiry is now closed.’’
This example emphasizes that when unplanned influences or events interact with medical device operation, tragic results may occur. In a later section, we describe several human factors procedures and techniques that are now designed to help preclude these types of untoward events.
In Ref. 36, a second example shows how important (delicate) care is requisite to providing appropriate interaction of humans with medical devices.
Case Study 2 from Ref. 36
Besides putting patients at high risk for injury, clinicians who use a device they are not familiar with are placing themselves in legal jeopardy. The case of Chin vs. St. Barnabos Medical Center (160 NJ 454 [NJ 1999]) illustrates
this point. A patient died after gas inadvertently was pumped into her uterus during a diagnostic hysteroscopy. Evidence established that the two perioperative nurses implicated in the case had no experience with the new hysteroscope and used the wrong hook up for the procedure. They connected the exhaust line to the outflow port. The 45-year-old patient died from a massive air embolism. It was also discovered that the nurses never received any education regarding the device. The manufacturer was not found liable because records indicated that the device did not malfunction or break. Damages in the amount of $2 million were awarded to the plaintiff and apportioned among the surgeon, nurses, and hospital. As discussed in the sequel, new training methods have been developed in the human factors area to preclude the occurrence of events of this type.
The last case study deals with a poor interface design. Usability Testing, to be discussed later, provides methods to preclude some of these difficulties encountered.
Case Study 3 from Ref. 37
‘‘A 67 year-old man has ventricular tachycardia and reaches the emergency room. Using a defibrillator, nothing happens. The doctor suggests the nurse to start a fluid bolus with normal saline. The nurse opens the IV tubing wide open, but within minutes the patient starts seizing. The nurse then realizes that the xylocaine drip instead of the saline had been inadvertently turned up. The patient is then stabilized and the nurse starts her paperwork. She then realizes that the defibrillator was not set on the cardio version, but rather on an unsynchronized defibrillation. This is because the defibrillator she uses, every day, automatically resets to the nonsynchronized mode after each shock. The second shock must have been delivered at the wrong time during the cardiac cycle, causing ventricular fibrillation.’’ By performing a usability study as described later, with better training, this type of event could have been prevented.
The changing effect of legal influences also has had its impact on human factor interactions of caregivers with medical devices. It is worthwhile to briefly describe some of these recent influences and how they impact on human dealings with medical devices.
NEW LEGAL INFLUENCES THAT AFFECT HUMAN FACTORS
As mentioned previously in Refs. 13–15, there have been a number of modifications in the legal system that affect how humans now interact with medical devices. It is not unusual in the year 2005 to hear prescription drugs advertised on television or on the radio with a disclaimer near the end of each commercial. The disclaimer lists major possible side effects and warns the user to discuss the drug with their physician. As the aging ‘‘baby boomers’’ of the post-World War II era now require more and more medications, the drug companies make major efforts and studies to ensure that safe and effective drugs are delivered to an ever increasing public audience. Experience from prior mistakes has significantly modified how the drug industry must deal with a larger, and more highly informed, popu-
HUMAN FACTORS IN MEDICAL DEVICES |
539 |
lation base. Some major modifications that occur involving legal issues and medical device operation include
1. The legal profession (13) now recognizes the importance of human factors engineering [also known as usability engineering or ergonomics (a term used outside the United States)] in studying how humans interact with machines and complex systems. Ergonomics is a factor in the design of safe medical devices; A user-friendly device is usually a safe one (38).
2. Healthcare Institutions employ results of human factors engineering testing of devices in making key decisions in evaluation as well as major purchase judgments. If these components fail, but have been tested within a rigorous framework, the legal consequences are mitigated since standards were adhered to in the initial selection of the medical device and procedure of use.
3. Insurance premiums to Healthcare Institutions are correspondingly reduced if adherence to standards set forth by good human factors engineering principles are maintained. The insurance costs are directly related to the potential of legal expenses and thus sway the decisions on how medical devices are purchased and used.
A number of new ways of improving how human factor design with medical devices has evolved, which will now be discussed as pertinent to the prior discussion. These methods affect training, utilization procedures, design of the devices, testing, and overall interaction with caregivers in the workplace.
METHODS TO IMPROVE HUMAN FACTOR DESIGN AND MEDICAL DEVICES
Professionals working in the area of human factors have now devised a number of new means of improving how healthcare professionals can better deal with medical devices. We present some of the most popular methods in the year 2005, most of which now pervasively affect the development of a user’s manual, training, and manner of use with respect to medical devices. Some of these techniques appear to have overlap, but the central theme of these approaches is to better assist the healthcare professional to mitigate untoward events. One of the most popular methods derived from human factors studies is cognitive task analysis (CTA). In short, the way that CTA works is that a primary task is subdivided up into smaller tasks that must be performed. It is necessary to specify the information needed to perform each subtask, and the decisions that direct the sequence of each subtask. Note, this type of task description is independent of the automation involved. For example, for the same tasks, information and decisions are required regardless of whether they are performed by a human or a machine. Also considered in this analysis are the mental demands that would be placed on the human operator while performing these selected subtasks.
540 HUMAN FACTORS IN MEDICAL DEVICES
Cognitive Task Analysis and How it Affects Human Factors and Medical Devices
The principle behind CTA is to take a large and complex task and divide it up into smaller subtasks (39). Each subtask should be attainable and reasonable within the scope of the user. If the subtask is not yet in the proper form, further subdivisions of that subtask are performed until the final subtask is in the proper form. The expression ‘‘proper form’’ implies the subtask is now attainable, sufficiently reasonable to perform, the proper information has been provided, and sufficient control is available to execute this subtask. An important aspect of CTA is to define if the user has the proper information set to complete his duties and also has the proper control means over the situation so that the task can be achieved adequately. Cognitive task analysis has great value in establishing a set of final subtasks that are both attainable and relevant to the overall mission. With this analysis, the caregiver can be provided better training and have an enhanced understanding of the role of each task within the overall mission. This procedure has been used in the nursing area for assessing risk of infants (40) and for patient-controlled analgesia machines (41). It has been noted (42) that 60% of the deaths and serious injuries communicated to the Medical Device Reporting system of the U.S. Food and Drug Administration (FDA) Center for Devices and Radiological Health have been attributed to operator error. Cognitive task analysis has evolved out of the original area of Critical Decision Methods (43) and is now an accepted procedure to analyze large and complex interactions of humans with machines.
A second popular method to shape procedures to interact with medical devices involves User Testing and Usability Engineering.
User Testing and How It Affects Human Factors and Medical
Devices
User Centered Design has found popularity when humans have to interact with medical devices for ultrasound systems (44) and for people with functional limitations (45). Usability engineering methods are applied early in the system lifecycle to bridge the gap between users and technology. The ultimate goal is to design an easy to use system that meets the needs of its users. A basic principle of usercentered design is making design decisions based on the characteristics of users, their job requirements and their environments (46–50). It is often the complaint of human factors professionals that they are brought into the design process much too late to influence the construction of the overall system. It is all too common for the experimental psychologist to have to deal with an interface built without prior considerations of the human’s limitations and preferences in the initial design construction. The usability engineering methods bring to light needs for users and tasks early on, and suggest specific performance testing prior to the recommendation of the final design of an interface.
A third method discussed here to influence how to work with medical devices involves Work Domain Analysis.
Work Domain Analysis and How It Affects Human Factors and Medical Devices
A third and popular method to better understand the interplay between human factors issues and medical devices is via an integrated method involving the technical world of physiological principles and the psychological world of clinical practice. This work domain analysis was originally proposed by Rasmussen et al. (51,52) and has found application in patient monitoring in the operating room (53). A variety of tables are constructed based on data to be utilized. Columns in the tables include a description of the task scenario and the relations between key variables of the work environment and the work domain. The tables portray interactions and different strategies that are elicited to help in monitoring and control.
As discussed earlier in Ref. 1, today many new advances have also been made in alarms. These inform the healthcare provider of troublesome events and many innovative changes and studies have been instituted in this area that warrant discussion. Alarm deficiencies compromise the ability to provide adequate healthcare. For alarms, some research has focused on the identification of alarm parameters that improve or optimize alarm accuracy (i.e., to improve the ratio of true positives to false positives: the signal/noise ratio).
ALARMS AND HUMAN FACTORS ISSUES
Alarms are key to the detection of untoward events when humans interact with medical devices. One does not want to generate designs that invite user error. We cannot deal with confusing or complex controls, labeling, or operation. Many medial devices have alarms or other safety devices. If, however, these features can be defeated without calling attention to the fact that something is amiss, they can be easily ignored and their value is diminished (54). The efficacy of alarms may be disregarded because it is not attention getting. For example, if a multifunction liquidcrystal display (LCD) has a low battery warning as its message, but is not blinking, it does not call attention to itself. Alternatively, an improved design occurs in the case of a low battery alarm design commonly found in household smoke detectors. In this case, a low battery will cause the unit to chirp once a minute for a week, during which the smoke detector is still functional. The chirp may be confusing at first, but it cannot be ignored for a week. A battery test button is still available for the testing when the battery power is satisfactory. Adequate alarm systems are important to design in a number of analogous medical scenarios. For example, use of auditory systems (55) is preferable to a visual display, since this reduces the visual workload associated with highly skilled tasks that may occur, for example, in the operating room. For anesthesia alarms (56), care must be exercised to not have too many low level alarms that indicate, for example, that limits are exceeded or that the equipment is not functioning properly. The danger of false positives (alarms sounding when not necessary) provides an opportunity for the user to ignore information, which may be critical in a slightly different setting. An example where information of this type cannot be

ignored is in applications of human factors training to the use of automated external defibrillators. It is known that without defibrillation, survival rates drop by 10% for every minute that passes after cardiac arrest (57). A great deal of work still continues in the area of management of alarm systems in terms of their efficacy and utility (58,59).
Another significant issue with human factors is proper labeling. Medication misadventures are a very serious problem. We briefly summarize changes that impact how humans will interact with their prescriptions as well as medical devices in general and how they are influenced by their labeling constraints.
LABELING AND HUMAN FACTORS ISSUES
By government regulation and industry practice, instructions accompanying distribution of medical devices to the public are termed ‘‘labeling’’. Medical device labeling comprises directions on how to use and care for such practices. It also includes supplementary information necessary for the understanding and safety, such as information about risks, precautions, warning, potential adverse reactions, and so on. From a humans factors perspective, the instructions must have the necessary efficacy, that is, they must provide the correct information to the user. There are a number of standards on how the instructions must be displayed and their utility in the healthcare industry (60). For example, for prescription medications (61–64), they represent the most important part of outpatient treatment in the United States. This provides > 2 billion possible chances for patient error each year in the United States. To maximize the benefits and minimize the dangers of using these medications, users must comply with an often complex set of instructions and warnings. Studies show that seven specific system failures account for 78% of adverse drug events in hospitals. All seven of these failures could be corrected by better information systems that detect and correct for errors. The top seven system failures for prescription medications are (1) drug knowledge dissemination; (2) dose and identification checking; (3) patient
HUMAN FACTORS IN MEDICAL DEVICES |
541 |
information availability; (4) order transcription error; (5) allergy defense; (6) medication order tracking; (7) improved interservice communication.
As mentioned previously, as computers and the Internet become more persuasive, patients, caregivers, doctors, and others become more tolerant and dependent on automation. The goal is to make a task easier, which is true most of the time. There are a number of issues with regard to automation that need to be addressed.
AUTOMATION ISSUES AND HUMAN FACTORS
As computers and microprocessor-based devices have become more ubiquitous in our modern age, there is increased tendency to foster automation (65) as a means of improving the interaction of users with medical devices. The original goal of automation was to reduce the workload (physical and mental) and complexity of a task to the user. This is specific to the desired response from the device of interest. There is an obvious downside of this concept. The idea that the automation has taken over and has a mind of its own is ghastly within human thinking. Also, if the automated system is too complex in its operation and the user is not comfortable in understanding its causality (input–output response characteristics), the trust in the device will decrease accordingly and the human–machine interaction will degrade. The classical work by Sheridan (66) defines eight possible levels of automation, as portrayed in Fig. 3. One easily sees the relationship of loss of control to increased automation. For medical device usage, this may be problematic to trade off simplicity of use to loss of control and eventual efficacy. Automation studies continue to be of interest (67–73).
REPORTING AND HUMAN FACTORS ISSUES
Reporting of failures of proper medical device operation has now commonly advanced to Web-based systems (3,74). The healthcare provider must be increasingly skilled with the use of computer systems. Sometimes the terms digital
Figure 3. The eight levels of automation.

542 HUMAN FACTORS IN MEDICAL DEVICES
divide is employed to distinguish those that have the requisite computer skills from those that are not as competent in this area. This may be a consequence of humans factors procedures instituted to deal with a more elderly patient group (75–82) who may not be comfortable with computers. Education is the best means to deal with this problem (83). It is important that modern healthcare givers who use medical devices in their work setting have the obligatory skills to accurately report failures and have the suitable computer training to make relevant reports to the necessary sources.
A number of new areas are growing and influence how human factors have been evolving with the interaction of medical devices. It is important to spend some time mentioning these contemporary and emergent areas.
NEW ISSUES INVOLVING HUMAN FACTORS AND MEDICAL DEVICES
With advances in technology, several new areas should be mentioned that seem to have relevance to novel advances in medical devices. The concept of telemedicine is now a developing field that certainly addresses the future uses of medical devices.
The Growth of Telemedicine
The term telemedicine literally means ‘‘medicine at a distance’’ (84) and is now an increasing and popular means of providing healthcare. The advantages are obvious in rural settings and numerous other scenarios (cf. Fig. 4). For example, having an expert physician or surgeon located at a remote and safe location, but performing a medical procedure on a person in a hazardous or distant environment provides a distinct advantage. The human at the hazardous environment may be placed in a battlefield in a combat situation, they may be in a space shuttle, or simply be in another country or distant location from the expert medical practitioner. Another simple example of telemedicine occurs in a simple endoscopic (colonoscopy) procedure or in a laparoscopic operation, for example, for knee surgery. For these procedures, a small insertion is made into
Figure 4. The concept of telemedicine.
the patient and the process is carried out from a remote location with the physician observing the process on a television monitor. The advantages are obvious: (1) with smaller entrance incisions or openings into the patient, the trauma is significantly reduced; (2) recovery time is much quicker; and (3) the risk of infection is substantially mitigated. Some of the new human factors issues regarding medical devices used within this context include (1) Dealing with the time delay between observing and making actions and the associated instabilities that may occur in the closed loop interaction; (2) having the lack of a sense of presence about a remote environment; and (3) having a strong dependence on mechanical systems or automation at the end-effector of the device inside the patient. These methods have been advanced to the point where robots are now being used to perform heart surgery, and so on, and some operations have been conducted over the Internet. Recent applications of robots performing heart procedures on humans need only two very small incisions in the patient. This allows for much quicker recovery time to the patient (1 vs. 7 weeks for a typical open heart surgery). From the surgeon’s perspective, a significant advantage for the small incisions is that: It is not necessary to insert my hands inside the chest cavity. Thus the size of the incisions can be substantially reduced. One sees the disadvantage of traditional surgery in this area because it is the size of the surgeon’s hands being required to be inside the chest cavity as the only reason for a large incision in the chest cavity. When the surgeon’s hands no longer have to be inside the chest cavity, then the correspondingly two small incisions give rise to reduced possible infection, less trauma to the patient, and a shorter recovery time before the patient can return to normal work and living activities. This area of healthcare will only continue to advance as medical practices move more and more to this form of undertaking. In recent times, a number of studies in teleoperation have shown the efficacy of improving the sense of presence of the operator about the remote environment through ‘‘haptic’’ feedback. Haptic refers to forces reflected back on the physician (by various robotic interface devices) to improve their sense of presence about the remote environment, so the operator can ‘‘feel’’ the task much as they see it on a television monitor. A number of studies have shown both an improved sense of presence and performance about these teleoperation scenarios using haptic feedback (85–88). Auditory systems have also found analogous use in surgery (89). The problems in anesthesia are also well studied (90–93).
Another growth area includes more participation by the patient directly in their own healthcare.
The Growth of Increased Patient Participation
in the Healthcare Process
As discussed previously, with the pervasive nature of automation, more and more of the healthcare responsibility and work will be performed by the patient, themself. Modern insurance procedures also encourage additional homecare scenarios and many times without a trained caregiver. This saves expensive care at the hospital, but transfers the burden onto the patient or their family members to become the primary caregiver. A paradigm
shift of this type is a consequence of present insurance reimbursement procedures requiring the patient to now spend much of their time away from the hospital. New human factors issues are consequently introduced when dealing with medical devices in this scenario. The design of the human computer interface (94–97) now becomes critical for the efficacy of the healthcare provided. Even in cancer treatment, the responsibility of the proper administration of radioisotopes may become the burden of the patient (98) or if they have to manipulate their own chemotherapy level. For pain treatment (99–101) the patient has to be proactive in the selection of the analgesia level of the device provided. Modern TENS (Transcutaneous Electrical Nerve Stimulator) units now have been constructed to be wireless and shown to have equivalent efficacy in terms of pain management as compared to long wired units that have been in existence for >40 years (102). The movement to more wireless medical devices is certainly in the future. For the TENS units, by eliminating the long and entangling wires, this provides more reliability, less chance of wires breaking or shorting, more efficient use of electric power, but different forms of control with these analgesia devices. For example, the physician or caregiver may use a remote control to program the voltage level of the TENS microprocessor in a wireless manner rather than making manual adjustments with the traditional, long wired, TENS devices.
A third area of modern concern is the impact of electromagnetic fields on the operation of other medical devices, especially if they are implanted.
The Growth of Electromagnetic Fields on the Operation of Other Medical Devices
The Geddes reference (35) describes numerous examples of documented problems when medical devices inadvertently interact with unexpected exposure to external electromagnetic fields. Electromagnetic interference (EMI) is used to describe the malfunction of a device exposed to electromagnetic waves of all types that propagate through space. The EMI can intervene with electrodes on a patient, it can bias results for EEG recording of generalized epileptiform activity, and can give false positives to alarm systems, Silbert et al. (103).Other caseswheremalfunctionscan occurinvolve heart machines, apnea monitors, ventilator mishaps, and in drug infusion pumps. Pacemakers are known to be affected by low frequency EMI signals. There are many exogenous sources of EMI including, but not limited to, Electrostatic Discharge, arc welding, ambulance sirens, and other sources (104). The growth of EMI is only increasing and human factors professionals need to carefully consider sources of problems from EMI that may have to be dealt with.
A fourth area of potential problems of humans factors interaction with medical devices occurs when two or more medical devices are simultaneously in operation, but their concurrent action may interact with each other in a destructive way.
The Potential Interaction of Multiple Medical Devices
As medical devices become more and more sophisticated, they may concurrently be in operation on the same patient
HUMAN FACTORS IN MEDICAL DEVICES |
543 |
(105–109). The action of one medical device may produce an undesired response of another device, especially if it may be implanted. From Geddes (35): ‘‘Between 1979 and 1995, the Center for Devices and Radiological Health (CDRH) of the U.S. Food and Drug Administration (FDA) has received over one hundred reports alleging the electromagnetic interference (EMI) resulted in malfunction of electronic medical devices.’’ The source of the EMI was from one medical device treating the patient. The malfunction occurred in a second medical device, which was also, simultaneously, being used to treat the same patient.
‘‘For example, about 100,000 cardiac pacemakers are implanted annually. These stimulators can be interrogated and programmed by an external device that uses a radio frequency link. Electro surgery, which also uses radio frequency electric current may interact with the pacemaker causing serious arrhythmias. Even though the two technologies are safe, when used alone, their simultaneous combination has resulted in injury.’’ More specifically, nowadays with the prevalence use of cellular telephones for both caregivers as well as the patients in care situations, there are documented cases of resulting injury to the patient. Cell phones have now been recognized to cause instances of malfunction of drug infusion pumps and patient monitors. These interactions have to be considered for new human factors interactions with medical devices in the future, Silbergerg (110) with increased interest in the errors created (111,112) and the specific technology used (113).
With the changing style of litigation with respect to the medical profession, there has been more public awareness of sources of human factor error induced by the medical professional working in a state of extreme fatigue.
Increased Public Awareness to Fatigue Issues and the Medical Professional
There has now been a substantial increased awareness of the general public to the fact that their medical professional may have compromised performance due to the fact that they are suffering from long hours of work. Fatigue studies continue to receive increased concern (114–120). This certainly has its influence on human factors procedures when dealing with medical devices and the overall success of the medical interaction. For example (115), it is known that physicians had demonstrated levels of daytime sleepiness worse then that of patients with narcolepsy or sleep apnea when required to perform long hours of duty.
Finally, since the publication of Ref. 1, the healthcare industry must now deal with a substantially larger population of acquired immune deficiency syndrome (AIDS) survivors who need medical, dental, and other types of interactions with healthcare professionals (121).
Changing Medical Procedures to Deal with Active Human Immunodeficiency Virus Patients
With the advent of advanced drug therapies, people with human immunodeficiency virus (HIV) are now living longer and longer. These same people need dental care, have medical attention requests, and require other types of consideration. The medical professional must exercise
544 HUMAN FACTORS IN MEDICAL DEVICES
forethought to not have exposure to body fluids and new procedures are in place to provide discrimination free care to these people. In the early days of public exposure to people with HIV, there were documented cases of health professionals refusing to give adequate care. For example, for resuscitation, fireman and others would avoid contact with individuals suspected of having HIV. New devices have now been constructed to keep body fluids and other contact more separated between the patient and the caregiver. There have been new laws passed to prevent discrimination to people suspected of having HIV in housing, in the workplace, and also in receiving adequate healthcare.
CONCLUSION
The modern human factors interactions with medical devices have been strongly influenced by the advent of new technologies including the Internet, microprocessors, and computers. People are becoming more accustomed to automation and dealing with other sophisticated means of delivering healthcare. One lesson that can be learned from the improvement of human factors interactions with medical devices is that we can create safety by anticipating and planning for unexpected events and future surprises. Another change in this new millennium is that the responsibility of the patient is now shifted more to the individual or their family to have a greater role and duty over their own therapies and venue, and perhaps work in their home setting. Telemedicine and wireless means of dealing with controls over the medical devices are certainly on the increase and will influence how the patient has to deal with their healthcare professional in the future.
BIBLIOGRAPHY
Cited References
1.Hyman WA. Human Factors in Medical Devices. In Webster JG editor Encyclopedia of Medical Devices and Instrumentation. 1st ed. New York: Wiley; 1988.
2.Fries RC. Reliable Design of Medical Devices. New York: Marcel Dekker; 1997.
3.U. S. Food and Drug Administration, Guidance for Industry and FDA Premarket and Design Control Reviewers–Medical Device Use-Safety: Incorporating Human Factors Engineering into Risk Management. Available at http://www.fda.gov/ cdrh/humfac/1497.html.
4.Sawyer D. An Introduction to Human Factors in Medical Devices. U. S. Department of Health and Human Services, Public Health Service, FDA; December, 1996.
5.Murff HJ, Gosbee JW, Bates DW. Chapter 41. Human Factors and Medical Devices. Available at http://www.ncbi.nlm.- nih.gov.books/.
6.Human Factors and Medical Devices. Available at http:// www.ahrq.gov/clinc/ptsafety/chap41b.htm.
7.Association for the Advancement of Medical Instrumentation. Human Factors Engineering Guidelines and Preferred Practices for the Design of Medical Devices. ANSI/AAMI HE48-1993, Arlington (VA); 1993.
8.Backinger CL, Kingsley P. Write it Right: Recommendations for Developing User Instructions for Medical Devices in
Home Health Care. Rockville (MD): Department of Health and Human Services; 1993.
9.Burlington DB. Human factors and the FDA’s goals: improved medical device design. Biomed Instrum Technol Mar.–Apr., 1996;30(2):107–109.
10.Carpenter PF. Responsibility, Risk, and Informed Consent. In: Ekelmen KB, editors. New Medical Devices: Invention, Development, and Use. Series on Technology and Social Priorities. Washington (DC): National Academy Press; 1988. p 138–145.
11.Policy statements adopted by the governing council of the American Public Health Association. Am J Public Health. Nov. 12, 1997;88(3):495–528.
12.Reese DW. The Problem of Unsafe Medical Devices for Industry, Government, Medicine and the Public. Dissertation Abs International: Sect B: Sci Eng 1994;54(11-B):5593.
13.Claris Law, Inc. Use of Human factors in Reducing Devicerelated Medical Errors, available at http://www.injuryboard. com/.
14.Green M. An Attorney’s Guide to Perception and Human Factors. Available at http://www.expertlaw.com/library/ attyarticles/perception.html.
15.Green M. Error and Injury in Computers and Medical Devices. Available at http://www.expertlaw.com/library/attyaricles/ computer_negligence.html.
16.Sokol A, Jurevic M, Molzen CJ. The changing standard of care in medicine-e-health, medical errors, and technology add new obstacles. J Legal Med 2002;23(4):449–491.
17.Bruckart JE, Licina JR, Quattlebaum M. Laboratory and flight tests of medical equipment for use in U.S. army medevac helicopters. Air Med J 1993;1(3):51–56.
18.Budman S, Portnoy D, Villapiano AJ. How to Get Technological Innovation Used in Behavioral Health Care: Build It and They Still Might Not Come. Psychother Theory, Res Practice, Training 40 (1–2), Educational Publishing Foundation; 2003. p 45–54.
19.Burley D, Inman WH, editors. Therapeutic Risk: Perception, Measurement, Management. Chichester: Wiley; 1988.
20.Hasler RA. Human factors design-what is it and how can it affect you?. J Intravenous Nursing May–Jun, 1996;19(3)(Suppl.): S5–8.
21.McConnell EA. How and what staff nurses learn about the medical devices they use in direct patient care. Res Nursing Health 1995;18(2):165–172.
22.Obradovich JH, Woods DD. Users as designers: how people cope with poor HCI design in computer-based medical devices. Human Factors 1996;38(4):574–592.
23.Phillips CA. Human Factors Engineering. New York: Wiley; 2000.
24.Senders JW. Medical Devices, Medical Errors, and Medical Accidents. Human Error in Medicine. Hillsdale (NJ): Lawrence Erlbaum Associates, Inc.; 1994. p 159–177.
25.Ward JR, Clarkson PJ. An analysis of medical device-related errors: prevalence and possible solutions. J Med Eng Technol Jan–Feb, 2004;28(1):2–21.
26.Goldmann D, Kaushal R. Time to tackle the tough issues in patient safety. Pediatrics Oct. 2002;110(4):823–827.
27.Gosbee J. Who Left the Defibrillator On? Joint Comm J Quality Safety May, 2004;30(5):282–285.
28.Kaptchuk TJ, Goldman P, Stone DA, Stason WB. Do medical devices have enhanced placebo effects? J Clin Epidemiol 2000;53:786–792.
29.Lambert MJ, Bergin AE. The Effectiveness of Psychotherapy. In: Bergin AE, Garfield SL, editors. Handbook of Psychotherapy and Behavior Chance. 4th ed. New York: Wiley; 1994. p 143–189.
30.Perry SJ. An Overlooked Alliance: Using human factors engineering to reduce patient harm. J Quality Safety 2004; 30(8):455–459.
31.Leape L. Error in medicine. J Am Med Assoc 1994;21(3):272.
32.Leape LL. The preventability of medical injury. In: Bogner MS, editor. Human Error in Medicine Hillsdale (NJ): Lawrence Erbaum Associates; 1994. p 13–25.
33.Ganiats T. Error. J Am Med Asso 1995;273:1156.
34.Bogner MS. Medical human factors. Proc Human Factors Ergonomics Soc, 40th Annu Meet; 1996. p 752–756.
35.Geddes LA. Medical Device Accidents. 2nd ed. Lawyers and Judges, Publishers 2002.
36.Wagner D. How to use medical devices safely. AORN J Dec. 2002;76(6):1059–1061.
37.Fairbanks RJ, Caplan S. Poor interface design and lack of usability testing facilitate medical error. Human Factors Engineering Series. J Quality Safety Oct. 2004;30(10):579–584.
38.Phillips CA. Functional Electrical Rehabilitation, SpringerVerlag, 1991.
39.Militello LG. Learning to think like a user: using cognitive task analysis to meet today’s health care design challenges. Biomed Instrum Technol 1998;32(5):535–540.
40.Militello L. A Cognitive Task Analysis of Nicu Nurses’ Patient Assessment Skills. Proc Human Factors Ergonomics Soc, 39th Annu Meet; 1995. p 733–737.
41.Lin L, et al. Analysis, Redesign, and Evaluation of a PatientControlled Analgesia Machine Interface. Proc Human Factors Ergonomics Soc, 39th Annu Meet; 1995. p 738–741.
42.Bogner MS. Medical devices and human error. In: Mouloua M, Parasuraman R, editors. Human Performance in Automated Systems: Current Research and Trends. Hillsdale (NJ): Erlbaum; 1994. p 64–67.
43.Klein GA, Calderwood R, MacGregor D. Critical decision method for eliciting knowledge. IEEE Trans. Systems, Man, Cybernetics 1989;19(3):462–472.
44.Aucella AF, et al. Improving Ultrasound Systems by UserCentered Design. Proc Human Factors Ergonomics Society, 38th Annu Meet; 1994. p 705–709.
45.Law CM, Vanderheiden GC. Tests for Screening Product Design Prior to User Testing by People with Functional Limitations. Proc Human Factors Ergonomics Soc, 43rd. Annu Meet; 1999. p 868–872.
46.Neilsen J. Usability Engineering. Boston: Academic; 1993.
47.Whiteside BJ, Holtzblatt K. Usability engineering: our experience and evolution. In: Helander M, editor. The Handbook of Human Computer Interaction. New York: Elsevier Press; 1988.
48.Nielsen J. Heuristic evaluation. In: Nielson J, Mack R, editors. Usability Inspection Methods. New York: Wiley; 1994. p 54–88.
49.Welch DL. Human factors in the health care facility. Biomedical Instrum Technol. May–Jun, 1998;32(3):311–316.
50.Lathan BE, Bogner MS, Hamilton D, Blanarovich A. Humancentered design of home care technologies. NeuroRehabilitation 1999;12(1):3–10.
51.Rasmussen J, Pejtersen AM, Goodstein LP. Cognitive Systems Engineering. New York: Wiley; 1994.
52.Rasmussen J. Information Processing and Human-Machine Interaction: An Approach to Cognitive Engineering. New York: North-Holland; 1986.
53.Hajdukiewicz JR, et al. A Work Domain Analysis of Patient Monitoring in the Operating Room. Proc Human Factors Ergonomics Soc, 42th Annu Meet; 1998. p 1038–1042.
54.van Gruting CWD. Medical Devices–International Perspectives on Health and Safety. New York: Elsevier; 1994.
55.Simons D, Fredericks TK, Tappel J. The Evaluation of an Auditory Alarm for a New Medical Device. Proc Human Factors Ergonomics Soc, 41st Annu Meet; 1997. p 777–781.
56.Seagull FJ, Sanderson PM. Anesthesia Alarms in Surgical Context. Proc Human Factors Ergonomics Soc, 42nd. Annu Meet; 1998. p 1048–1051.
HUMAN FACTORS IN MEDICAL DEVICES |
545 |
57.Aguirre R, McCreadie S, Grosbee J. Human Factors and Training Evaluation of Two Automated External Defibrillators. Proc Human Factors Ergonomics Soc, 43rd Annu Meet; 1999. p 840–844.
58.Woods DD. The alarm problem and directed attention in dynamic fault management. Ergonomics 1995;38(11):2371– 2394.
59.Laughery KR, Wogalter MS. Warnings and risk perception. design for health and safety. In: Salvendy G, editor. Handbook of Human Factors and Ergonomics. 2nd ed. New York: Wiley; 1997. p 1174–1197.
60.Callan JR, Gwynee JW. Human Factors Principles for Medical Device Labeling. Available at http://www.fda.gov/cdrh/ dsma/227.html.
61.Isaacson JJ, Klein HA, Muldoon RV. Prescription Medication Information: Improving Usability Through Human Factors Design. Proc Human Factors Ergonomics Soc, 43rd Annu Meet; 1999. p 873–877.
62.Collet JP, Bovin JF, Spitzer WO. Bias and confounding in pharmacoepidemiology. In: Strom BL, editor. Pharmacoepidemiology. New York: Wiley; 1994. p 741.
63.Senn S. Statistical Issues in Drug Development. New York: Wiley; 1997.
64.Twomey E. The usefulness and use of second-generation antipsychotic medications: review of evidence and recommendations by a task force of the World Psychiatric Association. Curr Opinion Psychiat 2002;15(Suppl 1):S1–S51.
65.O’Brien TG, Charlton SG. Handbook of Human Factors Testing and Evaluation. Lawrence Erlbaum Associates; 1996.
66.Sheridan TB. Humans and Automation: System Design and Research Issues. New York: Wiley; 2002.
67.Obradovich JH, Woods DD. Users as Designers: How People Cope with Poor HCI Design in Computer-based Medical Devices. Human Factors 1996;38(4):574–592.
68.Howard SK. Failure of an automated non-invasive blood pressure device: the contribution of human error and software design flaw. J Clin Monitoring 1993; 9.
69.Sarter NB, Woods DD, Billings CE. Automation surprises. In: Salvendy G, editor. Handbook of Human Factors/Ergonomics. 2nd ed. New York: Wiley; 1997. p 1926–1943.
70.Andre J. Home health care and high-tech medical equipment, caring. Nat Assoc Home Care Mag Sept. 1996; 9–12.
71.Dalby RN, Hickey AJ, Tiano SL. Medical devices for the delivery of therapeutic aerosols to the lungs. In: Hickey AJ, editor. Inhalation Aerosols: Physical and Biological Basis for Therapy. New York: Marcel Dekker; 1996.
72.Draper S, Nielsen GA, Noland M. Using ‘No problem found’ in infusion pump programming as a springboard for learning about human factors engineering. Joint Comm J Quality Safety Sept. 2004;30(9):515–520.
73.Weinger MB, Scanlon TS, Miller L. A widely unappreciated cause of failure of an automatic noninvasive blood pressure monitor. J Clin Monitoring Oct. 1992;8(4):291–294.
74.Walsh T, Beatty PCW. Human factors error and patient monitoring. Physiol Meas 2002;23:R111–132.
75.Agree EM, Freedman VA. Incorporating assistive devices into communitybased long-term care: an analysis of the potential for substitution and supplementation. J Aging Health 2000;12:426–450.
76.Rogers WA, Fisk AD. Human Factors Interventions for the Health Care of Older Adults. Mahwah (NJ): Lawrence Erlbaum Associates, Publishers; 2001.
77.Vanderheiden GC. Design for people with functional limitations resulting from disability, aging, or circumstance. In: Salvendy G, editor. Handbook of Human Factors and Ergonomics. 2nd ed. New York: Wiley; 1997. p 2010–2052.
546HUMAN FACTORS IN MEDICAL DEVICES
78.Billing J. The Incident Reporting and Analysis Loop. In Enhancing Patient Safety and Reducing Medical Errors in Health Care. Chicago: National Patient Safety Foundation; 1999.
79.Fisk D, Rogers WA. Psychology and aging: enhancing the lives of an aging population. Curr Directions Psychol Sci Jun. 2002;11(3):107–111.
80.Gardner-Bonneau D. Designing medical devices for older adults. In: Rogers WA, Fisk AD, editors. Human Factors Interventions for the Health Care of Older Adults Mahwah (NJ): Erlbaum; 2001. p 221–237.
81.Park C, Morrell RW, Shifren K. Processing of medical information in aging patients: cognitive and human factors perspectives. Lawrence Erlbaum Associates; 1999.
82.Sutton M, Gignac AM, Cott C. Medical and everyday assistive device use among older adults with arthritis. Can J Aging 2002;21(4):535–548.
83.Glavin RJ, Maran NJ. Practical and curriculum applications integrating human factors into the medical curriculum. Med Educ 2003;37(11):59–65.
84.Birkmier-Peters DP, Whitaker LA, Peters LJ. Usability Testing for Telemedicine Systems: A Methodology and Case Study. Proc Human Factors Ergonomics Soc, 41st Annu Meet; 1997. p 792–796.
85.Repperger DW. Active force reflection devices in teleoperation. IEEE Control Systems Jan. 1991;11(1) 52–56.
86.Repperger DW, et al. Effects of haptic feedback and turbulence on landing performance using an immersive cave automatic virtual environment (CAVE). Perceptual Motor Skills 2003;97:820–832.
87.Repperger DW. Adaptive displays and controllers using alternative feedback. CyberPschol Behavior 2004;7(6):645–652.
88.Repperger DW, Phillips CA. A haptics study involving physically challenged individuals. Encyclopedia of Biomedical Engineering. New York: Wiley; 2005.
89.Wegner CM, Karron DB, Surgical navigation using audio feedback. Studies in Health Technology and Informatics. 1997;39:450–458.
90.Cooper J. An analysis of major errors and equipment failures in anesthesia management: considerations for prevention and detection. Anesthesiology 1984;60:34–42.
91.Gaba DM, Howard SK, Jump B. Production pressure in the work environment: California anesthesiologists’ attitudes and experiences. Anesthesiology 81: 1994; 488–500.
92.Howard SK, et al. Anesthesia crisis resource management training: teaching anesthesiologists to handle critical incidents. Aviation Space Environ Med 63:763–770.
93.Weinger MB. Anesthesia incidents and accidents. Misadventures in health care: Inside Stories. Mahwah, (NJ): Lawrence Erlbaum Associates, Publishers; 2004. p 89–103.
94.Obradovic JH, Woods DD. Users as Designers: How People Cope with Poor HCI Design in Computer-Based Medical Devices. Proc Human Factors Ergonomics Soc, 38th Ann Meet; 1994. p 710–714.
95.Kober, Mavor A, editors. Safe, Comfortable, Attractive, and Easy to Use: Improving the Usability of Home Medical Devices. Report of National Research Council to U.S. Congress 1996, Washington (DC): National Academy Press; 1996. p 5–8.
96.Baldwin GM. Experiences of Siblings of In-Home Technol- ogy-Dependent Children. Dissertation Abst Int: Sec B: Sci Eng 1997;58(5-B):2714.
97.Mykityshyn AL, Fisk AD, Rogers WA. Learning to use a home medical device: mediating age-related differences with training. Human Factors 2002;44(3):354–364.
98.Schoenfeld I. Risk Assessment and Approaches to Addressing Human Error in Medical Uses of Radioisotopes. Panel: Proc Human Factors Ergonomics Soc, 37th Ann Meet; 1993. p 859–862.
99.Lin L. Human Error n Patient-Controlled Analgesia: Incident Reports and Experimental Evaluation. Proc Human Factors Ergonomics Soc, 42th Ann Meet; 1998. p 1043–1047.
100.Lin L, et al. Applying human factors to the design of medical equipment: patient controlled analgesia. J Clin Monitoring 1998;14:253–263.
101.McLellan H, Lindsay D. The relative importance of factors affecting the choice of bathing devices. Pain B J Occup Therapy 2003;66(9):396–401.
102.Repperger DW, Ho CC, Phillips CA. Clinical short-wire TENS (transcutaneous electric nerve stimulator) study for mitigation of pain in the Dayton va medical center. J Clin Eng Sept./Oct. 1997; 290–297.
103.Silbert PL, Roth PA, Kanz BS. Interference from cellular telephones in the electroencephalogram. J Polysomnographic Technol Dec. 1994;10:20–22.
104.Radiofrequency interference with medical devices. A technical information statement. IEEE Eng Med Bio Mag 1998;17(3):111–114.
105.Roy G. Child-proofing of hearing aids to prevent hazards posed by battery swallowing. J Speech-Language Pathol Audiol 1992;16(3):243–246.
106.Beery TA, Sommers M, Sawyer M, Hall J. Focused life stories of women with cardiac pacemakers. Western J Nursing Res 2002;24(1):7–23.
107.Romano PS. Using administrative data to identify associations between implanted medical devices and chronic diseases. Ann Epidemiol 2000;10:197–199.
108.Wiederhold K, Wiederhold MD, Jang DP, Kim SI. Use of cellular telephone therapy for fear of driving. CyberPsychol Behavior 2000;3(6):1031–1039.
109.Zinn HK. A Retrospective Study of Anecdotal Reports of the Adverse Side Effects of Electroconvulsive Therapy. Dissertation Abs Int Sec B: Sci Eng 2000;60(9-B):4871.
110.Silbergerg J. What Can/Should We Learn From Reports of Medical Device Electromagnetic Interference? At Electromagnetic, Health Care and Health, EMBS 95, Sept. 19–20, 1995, Montre´al, Canada: Standards Promulgating Organizations; 1995.
111.Leape LL, et al. Promoting patient safety by reducing medical errors. JAMA Oct. 1998;280:28 1444–1447.
112.Rasmussen J. The concept of human error: Is it useful for the design of safe systems in health care? In: Vincent C, DeMoll B, editors. Risk and Safety in Medicine. London: Elsevier; 1999.
113.Woods DD, Cook RI, Billings CE. The impact of technology on physician cognition and performance. J Clin Monitoring 1995;11:92–95.
114.Gaba DM, Howard SK. Fatigue among clinicians and the safety of patients. N Engl J Med 2002;347:1249–1255.
115.Howard SK, Gaba DM, Roseking MR, Zarcone VP. Excessive daytime sleepiness in resident physicians: risks, intervention, and implication. Acad Med 2002;77:1019–1025.
116.Cook RI, Render ML, Woods DD. Gaps in the continuity of care and progress on patient safety. Br Med J March 18, 2000;320:791–794.
117.Fennell PA. A Fourx-phase approach to understanding chronic fatigue syndrome. In: Jason LA, Fennell PA, Taylor RR., editors. The Chronic Fatigue Syndrome Handbook 2003. Hoboken (NJ): Wiley; 2003. p 155–175.
118.Fennell PA. Phase-based interventions. In: Jason LA, Fennell PA, Taylor RR, editors. The Chronic Fatigue Syndrome Handbook. Hoboken (NJ): Wiley; 2003. p 455–492.
119.Jason LA, Taylor RR. Community-based interventions. In: Jason LA, Fennell PA, Taylor RR, editors. The Chronic Fatigue Syndrome Handbook. Hoboken (NJ): Wiley; 2003. p 726–754.
