
- •Abbreviations
- •1 Overview of Antimicrobial Therapy
- •Factors in Antibiotic Selection
- •Factors in Antibiotic Dosing
- •Microbiology and Susceptibility Testing
- •PK/PD and Other Considerations in Antimicrobial Therapy
- •Antibiotic Failure
- •Pitfalls in Antibiotic Prescribing
- •References and Suggested Readings
- •2 Empiric Therapy Based on Clinical Syndrome
- •Empiric Therapy of CNS Infections
- •Empiric Therapy of HEENT Infections
- •Empiric Therapy of Lower Respiratory Tract Infections
- •Empiric Therapy of GI Tract Infections
- •Empiric Therapy of Genitourinary Tract Infections
- •Empiric Therapy of Sexually Transmitted Diseases
- •Empiric Therapy of Bone and Joint Infections
- •Empiric Therapy of Skin and Soft Tissue Infections
- •Sepsis/Septic Shock
- •Febrile Neutropenia
- •Transplant Infections
- •Toxin-Mediated Infectious Diseases
- •Bioterrorist Agents
- •References and Suggested Readings
- •Gram Stain Characteristics of Isolates
- •Parasites, Fungi, Unusual Organisms in Blood
- •Parasites, Fungi, Unusual Organisms in CSF/Brain
- •Parasites, Fungi, Unusual Organisms in Lungs
- •Parasites, Fungi, Unusual Organisms in Heart
- •Parasites, Fungi, Unusual Organisms in the Liver
- •References and Suggested Readings
- •5 HIV Infection
- •HIV Infection Overview
- •Stages of HIV Infection
- •Acute (Primary) HIV Infection
- •Initial Assessment of HIV Infection
- •Indications for Treatment of HIV Infection
- •Antiretroviral Treatment
- •Treatment of Other Opportunistic Infections in HIV
- •HIV Coinfections (HBV/HCV)
- •References and Suggested Readings
- •6 Prophylaxis and Immunizations
- •Surgical Prophylaxis
- •Post-Exposure Prophylaxis
- •Chronic Medical Prophylaxis
- •Endocarditis Prophylaxis
- •Travel Prophylaxis
- •Tetanus Prophylaxis
- •Immunizations
- •References and Suggested Readings
- •Empiric Therapy of CNS Infections
- •Empiric Therapy of HEENT Infections
- •Empiric Therapy of Lower Respiratory Tract Infections
- •Empiric Therapy of Vascular Infections
- •Empiric Therapy of Gastrointestinal Infections
- •Empiric Therapy of Bone and Joint Infections
- •Empiric Therapy of Skin and Soft Tissue Infections
- •Common Pediatric Antimicrobial Drugs
- •References and Suggested Readings
- •8 Chest X-Ray Atlas
- •References and Suggested Readings
- •9 Infectious Disease Differential Diagnosis
- •11 Antimicrobial Drug Summaries
- •Appendix
- •Malaria in Adults (United States)
- •Malaria in Children (United States)
- •Index
|
Chapter 7. Pediatric Infectious Diseases and Pediatric Drug Summaries |
411 |
|||
|
|
|
|
|
|
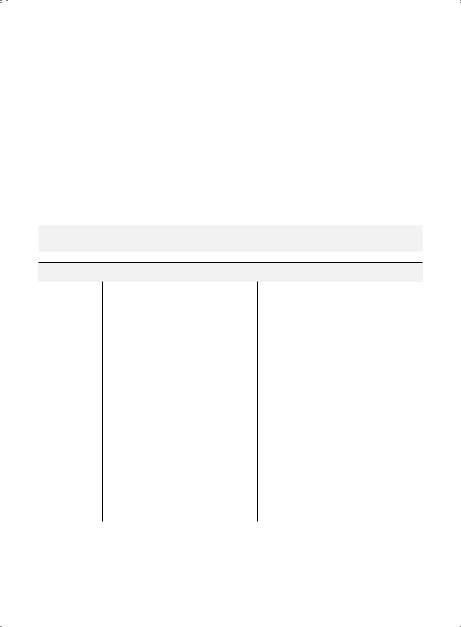
Empiric Therapy of Skin and Soft Tissue Infections |
|
||||
|
|
|
|
|
|
Skin and Soft Tissue Infections |
|
|
|
||
|
|
|
|
|
|
|
Usual |
Preferred IV |
Alternate |
PO Therapy or |
|
Subset |
Pathogens |
Therapy† |
IV Therapy† |
IV-to-PO Switch† |
|
Cellulitis, |
S.. aureus |
Cefazolin or |
Clindamycin‡ × |
Cephalexin or Cefadroxil or |
|
impetigo |
Group A |
nafcillin or |
7–10 days |
Dicloxacillin or Clindamycin |
|
|
streptococci |
oxacillin × |
|
or amoxicillin/clavulanate |
|
|
|
7–10 days |
|
or Erythromycin or |
|
|
|
|
|
Azithromycin ×7–10 days |
|
|
|
|
|
|
|
Severe |
CA-MRSA |
Vancomycin |
Vancomycin or |
TMP–SMX or Doxycycline |
|
pyodermas, |
|
plus |
Linezolid × 7–14 days |
× 7–14 days** |
|
abscesses |
|
Clindamycin × |
|
|
|
|
|
7–14 days |
|
|
|
|
|
|
|
|
|
Animal bite |
Group A |
Ampicillin- |
Piperacillin or Ticarcillin |
Amoxicillin/clavulanate or |
|
wounds (dog/ |
streptococci |
sulbactam × |
× 7–10 days |
Doxycycline × 7–10 days |
|
cat) |
P.. multocida |
7–10 days |
Penicillin allergy: |
|
|
|
Capnocyto |
|
|
|
|
|
|
Clindamycin plus |
|
|
|
|
phaga S.. |
|
|
|
|
|
|
TMP–SMX ×7–10 days |
|
|
|
|
aureus |
|
|
|
|
|
|
(dog bites); Doxycycline |
|
|
|
|
|
|
|
|
|
|
|
|
or Cefuroxime × |
|
|
|
|
|
7–10 days (cat bites) |
|
|
|
|
|
|
|
|
Human bite |
Oral anaerobes |
Ampicillin- |
Piperacillin or Ticarcillin |
Amoxicillin/clavulanate or |
|
wounds |
E.. corrodens |
sulbactam × |
× 5–7 days |
Doxycycline × 5–7 days |
|
|
Group A |
5–7 days |
Penicillin allergic patient: |
|
|
|
streptococci |
|
|
|
|
|
|
Clindamycin plus |
|
|
|
|
S.. aureus |
|
|
|
|
|
|
TMP–SMX × 5–7 days |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Cat scratch |
Bartonella |
Gentamicin × |
|
Azithromycin ×5 days or |
|
disease (CSD)* |
henselae |
10–14 days |
— |
TMP–SMX or Ciprofloxacin |
|
|
|
|
|
or Rifampin ×10–14 days |
|
|
|
|
|
|
|
†See pp. 414–422 for drug dosages.
**In children > 8 years of age..
*No well-controlled trials of antibiotic treatment for CSD to demonstrate benefit.
‡Preferred therapy for patients in geographic regions with a high prevalence of MRSA or for those with penicillin/cephalosporin allergy..
412 A n t i b i o t i c E s s e n t i a l s
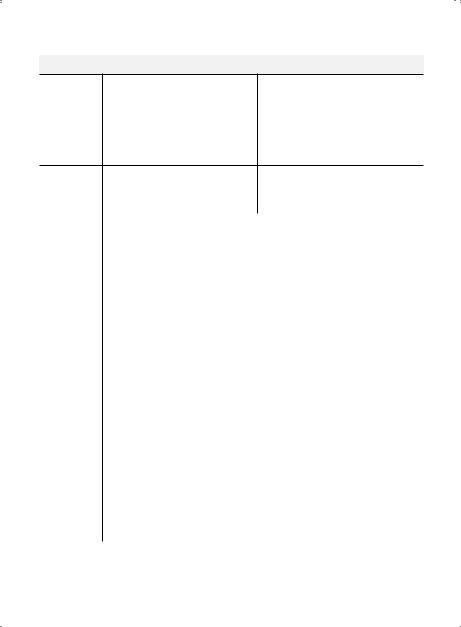
Skin and Soft Tissue Infections (cont’d)
|
|
|
PO Therapy or |
Subset |
Pathogens |
IV Therapy† |
IV-to-PO Switch† |
Chicken pox |
VZV |
Acyclovir × |
Acyclovir or Valacyclovir × 7–10 days |
Immuno- |
|
7–10 days |
|
compromised |
|
|
|
host |
|
|
|
|
|
|
|
Immuno- |
VZV |
Acyclovir × 5 |
Acyclovir or Valacyclovir × 5 days |
competent |
|
days |
|
host |
|
|
|
|
|
|
|
H.. zoster |
VZV |
Same as for |
Acyclovir or Valacyclovir × 10 days |
(Shingles) |
|
chicken pox |
(for individuals ≥ 12 years of age) |
|
|
|
|
Duration of therapy represents total time IV, PO, or IV + PO. . Most patients on IV therapy able to take PO meds should be switched to PO therapy soon after clinical improvement..
†See pp. 414–422 for drug dosages.
Cellulitis
Clinical Presentation: Erythema, warmth, and tenderness of skin.. Impetigo is characterized by a vesiculopapular rash with honey-colored discharge..
Diagnostic Considerations: Primarily a clinical diagnosis. . Group A streptococci is the primary pathogens in healthy children.. Cellulitis, alone without a pustular component, is caused by streptococci (not staphylococci)..
Pitfalls: Differential diagnosis of cellulitis may include hypersensitivity to insect bites.. Herpetic whitlow (HSV) may be mistaken for a bacterial skin or paronychial infection..
Therapeutic Considerations: First generation cephalosporin or semi-synthetic penicillin with antistaphylococcal activity (i..e.., dicloxacillin, nafcillin, oxacillin) are drugs of choice.. Increasing incidence of community-acquired MRSA may affect treatment decisions..
Prognosis: Excellent.. Impetigo may only require topical treatment (Mupirocin)..
Bite Wounds
Clinical Presentation: 80% of animal bite wounds in children are from dogs, and 15%–50% of dog bites become infected.. More than 50% of cat bites become infected, and due to their long teeth, there is an increased risk of inoculation into bone/joints with development of osteomyelitis/septic arthritis.. Human bite wounds are most prone to infection, and 75%–90% of all human bites become infected..
Diagnostic Considerations: Clinical diagnosis.. Culture of wound exudate may yield organism.. Pitfalls: Failure to assess depth of infection, especially with cat bites, may result in late identification of bone/joint infection.. Macrolides are ineffective against P.. multocida..
Therapeutic Considerations: It is important to cover oral anaerobes, S.. aureus, and Group A streptococci in human bite wounds. . P. . multocida is an important pathogen in cat and dog bite wounds. . Facial/hand lesions require plastic surgery evaluation.. Recurrent debridement may be necessary, especially with human bite wound infections of hand.. Assess tetanus immunization status for all bite wounds

Chapter 7. Pediatric Infectious Diseases and Pediatric Drug Summaries |
413 |
(p.. 377).. For human bites consider the risk of HIV and hepatitis B.. For dog bites consider the risk of rabies.. Antimicrobial therapy initiated within 8 hours of a bite wound and administered for 2–3 days may decrease the rate of infection..
Prognosis: Good with early debridement and antibiotics..
Cat Scratch Disease (CSD)
Clinical Presentation: Classic presentation is a papular lesion at site of cat scratch with lymphadenitis in the draining region (axillary, epitrochlear, inguinal, cervical most commonly). . Frequently associated with fever/malaise 1–2 weeks after scratch.. Infection can present with conjunctivitis and ipsilateral preauricular lymph node (Parinaud oculoglandular syndrome).. Unusual presentations in normal hosts include encephalitis, hepatitis, microabscesses in liver/spleen, fever of unknown origin, osteolytic lesions..
Diagnostic Considerations: Most often secondary to kitten scratch with Bartonella henselae. . Diagnosed using specific serology for antibodies to B.. henselae..
Pitfalls: Failure to obtain history of kitten exposure.. Surgical excision of lymph node is generally not necessary..
Therapeutic Considerations: Most lesions are self-limited and resolve over 2–4 months. . If lymph nodes are fluctuant, I&D may be indicated.. Antibiotic therapy may be helpful in severe cases with hepatosplenomegaly.. Doxycycline, erythromycin, or azithromycin are helpful in immunocompromised hosts.. Prognosis: Very good with spontaneous resolution over 2–4 months..
Chicken Pox/Shingles (VZV)
Clinical Presentation: Primary illness is chicken pox, a generalized pruritic, vesicular rash with fever that erupts in crops of lesions over 3–5 days followed by crusting and recovery.. Complications include bacterial superinfection of skin lesions, sepsis, cerebellar ataxia, thrombocytopenia, hepatitis, pneumonia and encephalitis.. The disease tends to be more severe in adolescents and adults, particularly if immunocompromised.. Primary infection early in pregnancy can rarely result in varicella embryopathy with imb atrophy and CNS malformations in the neonate.. Reactivation disease (shingles) may occur in children and in normal hosts and remains localized to a single dermatome.. Post-herpetic neuralgia occurs less often in children than adults.. Reactivation disease in immunocompromised hosts can spread and re-disseminate..
Diagnostic Considerations: The characteristic eruption of chicken pox occurs in waves—multi- ple stages appear at the same time, from new papules and vesicles to more advanced larger crusted lesions—and is unique to varicella.. Direct fluorescent antibody staining of a scraped lesion or PCR can confirm the diagnosis..
Pitfalls: Initially lesions may be primarily papular, and if the diagnosis is not considered, exposure of others can occur..
Therapeutic Considerations: Antiviral therapy with acyclovir, if started within 24 hours of rash, should be considered for children > 12 years of age, those on steroid or salicylate therapy, and those with underlying chronic pulmonary, skin, or immunosuppressive states.. Oral administration is acceptable, although IV therapy may be preferred for immunocompromised hosts at risk of disseminated disease.. More severe varicella has been observed in individuals acquiring the infection from a household contact, presumably due to a higher inoculum with closer contact; non-immune household contacts may be considered for acyclovir therapy at onset of rash in child.. Additionally,
414 |
A n t i b i o t i c E s s e n t i a l s |
individuals ≥ 13 years may develop more extensive varicella than younger children.. Immunocompromised children or pregnant women without a history of varicella or immunization may benefit from prophylaxis with varicella zoster immune globulin (VZIG) within 96 hours of varicella exposure.. Newborns whose mothers develop chicken pox within 5 days before or 48 hours after delivery and exposed premature infants are also candidates for VZIG.. A like-attenuated varicella vaccine has been licensed since 1995 for use in individuals ≥ 12 months of age who have not had chicken pox.. A twodose vaccine schedule is recommended for children ≥ 12 months of age..
Prognosis: Overall prognosis is good with complete recovery and minimal risk of scarring unless immunosuppressed host with disseminated disease. . Although rare, Group A streptococcal toxic shock syndrome (manifest as cellulitis or in conjunction with necrotizing fasciitis complicating varicella skin lesions) and Group A streptococcal septicemia, which can occur in the absence of apparent secondarily infected skin lesions, may be fatal complications of varicella in normal children..
Common Pediatric Antimicrobial Drugs
Drug |
Dosage in Neonates |
Dosage in Infants/Children* |
|
|
|
Acyclovir |
20 mg/kg (IV) q8h × 14–21 days.. |
HSV encephalitis: 10 mg/kg (IV) q8h × |
|
Dosing interval may need to be |
14–21 days |
|
increased for infants < 34 weeks |
Primary HSV infection: 10–20 mg/kg (PO) |
|
post-maturational age (GA + CA) or if |
q6h × 5–10 days or 5 mg/kg/dose (IV) |
|
significant renal impairment or liver |
q8h × 5 days |
|
failure followed by |
Varicella in immunocompromised hosts: |
|
Chronic suppression: 75 mg/kg |
10 mg/kg (IV) q8h × 7–10 days |
|
(PO) q12h × 6 months |
Varicella in immunocompetent hosts: |
|
|
20 mg/kg (PO) q6h × 5 days (maximum |
|
|
800 mg/dose) |
|
|
|
Albendazole |
Not applicable |
400 mg (PO) q24h |
|
|
|
Amikacin** |
During first week of life dosing is based |
5–7..5 mg/kg (IV or IM) q8h |
|
on gestational age (administer IV dose |
|
over 30 min)
•≤ 27 weeks (or asphyxia, PDA, or indomethacin): 18 mg/kg (IV) q48h
•28–30 weeks: 18 mg/kg (IV) q36h
•31–33 weeks: 16 mg/kg (IV) q36h
•≥34weeks:15mg/kg(IV)q24h
|
Chapter 7. Pediatric Infectious Diseases and Pediatric Drug Summaries |
415 |
|
|
|
|
|
Drug |
Dosage in Neonates |
Dosage in Infants/Children* |
|
After first week of life: Initial dose of 15 mg/kg, then draw serum
concentrations 30 min after end of infusion (peak) and 12–24 hours later (trough) to determine dosing interval.. Aim for peak of 20–30 mcg/mL and trough of 2–5 mcg/mL
Amoxicillin |
Not indicated |
|
22..5–45 mg/kg (PO) q12h |
|
|
|
|
|
|
Amoxicillin- |
Not indicated |
|
22..5–45 mg/kg (of amoxicillin |
|
clavulanate |
|
|
|
component) (PO) q12h |
|
|
|
|
|
Amphotericin B |
0..5–1 mg/kg (IV over 2–6 hours) q24-48h (Some authorities recommend an initial |
|||
(conventional) |
test dose of 0..1–0..5 mg/kg IV over 2–6 hours) |
|||
|
|
|
|
|
Ampicillin |
25–50 mg/kg/dose (IV or IM).. |
25–50 mg/kg (IV or IM) q6h |
||
|
Severe Group B streptococcal sepsis: |
|
||
|
100 mg/kg/dose.. Dosing interval is |
|
||
|
based on gestational age (GA) and |
|
||
|
chronological age (CA): |
|
|
|
|
|
|
|
|
|
GA + CA |
CA (days) |
Interval |
|
|
(weeks) |
|
(hours) |
|
|
|
|
|
|
|
≤ 29 |
0–28 |
12 |
|
|
|
> 28 |
8 |
|
|
|
|
|
|
|
30–36 |
0–14 |
12 |
|
|
|
> 14 |
8 |
|
|
|
|
|
|
|
≥ 37 |
0–7 |
12 |
|
|
|
> 7 |
8 |
|
|
|
|
|
|
Ampicillin- |
Not indicated |
|
25–50 mg/kg (of ampicillin component) |
|
sulbactam |
|
|
|
(IV) q6h |
|
|
|
|
|
Azithromycin |
Not indicated |
|
Otitis media/sinusitis: 30 mg/kg (PO) × 1 |
|
|
|
|
|
dose or 10 mg/kg (PO) q24h × 3 days or |
|
|
|
|
10 mg/kg (PO) on day 1 followed by 5 mg/ |
|
|
|
|
kg (PO) q24h on days 2–5 |
|
|
|
|
Pharyngitis/tonsillitis: 12 mg/kg (PO) |
|
|
|
|
q24h × 5 days |
|
|
|
|
|
*Dosages are generally based on weight (mg/kg), up to adult dose as maximum..
**Drug can be given IM but absorption may be variable..

416 |
A n t i b i o t i c E s s e n t i a l s |
|
|
|
|
Drug |
Dosage in Neonates |
Dosage in Infants/Children* |
|
|
|
|
|
Community-acquired pneumonia (not |
|
|
indicated for moderate or severe disease): |
|
|
10 mg/kg (PO) × 5 days or 10 mg/kg (IV |
|
|
or PO) on day 1 followed by 5 mg/kg (IV |
|
|
or PO) q24h on days 2–5 |
|
|
Skin/soft tissue infections (including Cat |
|
|
Scratch Disease): 10 mg/kg (PO) on day |
|
|
1 followed by 5 mg/kg (PO) q24h on |
|
|
days 2–5 |
|
|
|
Aztreonam |
30 mg/kg (IV or IM).. See ampicillin for |
30 mg/kg (IV or IM) q6-8h |
|
dosing interval (p.. 415) |
|
|
|
|
Caspofungin |
70 mg/m2 loading dose, then |
70 mg/m2 loading dose, then |
|
25 mg/m2 (IV) q24h |
50 mg/m2 (IV) q24h (> 3 months) |
Cefadroxil |
Not indicated |
15 mg/kg (PO) q12h |
|
|
|
Cefazolin |
25 mg/kg (IV or IM).. See ampicillin for |
25–100 mg/kg/day (IV or IM) divided |
|
dosing interval (p.. 415) |
q6–q8h |
|
|
|
Cefdinir |
Not indicated |
7 mg/kg (PO) q12h or 14 mg/kg (PO) |
|
|
q24h |
|
|
|
Cefepime |
50 mg/kg (IV) q12h |
33..3–50 mg/kg (IV or IM) q8h |
|
|
|
Cefotaxime |
50 mg/kg (IV or IM).. |
25–50 mg/kg (IV or IM) q6–8h |
|
(25 mg/kg/dose is adequate for |
|
|
gonococcal infection).. See ampicillin |
|
|
for dosing interval (p.. 415) |
|
|
|
|
Cefotetan |
Not indicated |
20–40 mg/kg (IV or IM) q12h |
|
|
|
Cefoxitin |
25–33 mg/kg/dose (IV or IM).. See |
80–160 mg/kg/day (IV or IM) divided |
|
ampicillin for dosing interval (p.. 415) |
q4–8h |
|
|
|
Cefpodoxime |
Not indicated |
5 mg/kg (PO) q12h |
|
|
|
Cefprozil |
Not indicated |
15 mg/kg (PO) q12h |
|
|
|
Ceftazidime |
30 mg/kg/dose (IV or IM).. See |
25–50 mg/kg (IV or IM) q8h |
|
ampicillin for dosing interval (p.. 415) |
|
|
|
|
Ceftibuten |
Not indicated |
9 mg/kg (PO) q24h |
|
|
|
Ceftizoxime |
Not indicated |
50 mg/kg (IV or IM) q6–8h |
|
|
|
*Dosages are generally based on weight (mg/kg), up to adult dose as maximum..

|
Chapter 7. Pediatric Infectious Diseases and Pediatric Drug Summaries |
417 |
|||||
|
|
|
|
|
|
||
Drug |
Dosage in Neonates |
Dosage in Infants/Children* |
|
||||
|
|
|
|
|
|||
Ceftriaxone‡ |
Sepsis and disseminated gonococcal |
50 mg/kg (IV or IM) q24h.. Meningitis: 50 |
|||||
|
infection: 50 mg/kg (IV or IM) q24h |
mg/kg (IV or IM) q12h or 100 mg/kg (IV |
|
||||
|
Meningitis: 100 mg/kg loading dose |
or IM) q24h |
|
||||
|
followed by 80 mg/kg (IV or IM) q24h |
Acute otitis media: 50 mg/kg (IM) × 1 |
|
||||
|
Uncomplicated gonococcal |
|
dose (or 3 doses IM q24h in high-risk |
|
|||
|
ophthalmia: |
|
|
|
patients) |
|
|
|
50 mg/kg (maximum 125 mg) as a |
|
|
||||
|
single dose (IV or IM) |
|
|
|
|||
|
|
|
|
|
|
|
|
Cefuroxime |
Not indicated |
|
10–15 mg/kg (PO) q12h |
|
|||
|
|
|
|
|
|
25–50 mg/kg (IV or IM) q8h |
|
|
|
|
|
|
|
|
|
Cephalexin |
Not indicated |
|
6..25–25 mg/kg (PO) q6h |
|
|||
|
|
|
|
|
|
|
|
Cephalothin |
Not indicated |
|
25 mg/kg (IV or IM) q4-6h |
|
|||
|
|
|
|
|
|
|
|
Clarithromycin |
Not indicated |
|
7..5 mg/kg (PO) q12h |
|
|||
|
|
|
|
|
|
||
Clindamycin |
5..0–7..5 mg (IV or PO).. Dosing interval |
5–10 mg/kg (IV or IM) q6-8h or 10–30 |
|
||||
|
is based on gestational age (GA) and |
mg/kg/day (PO) divided q6-8h |
|
||||
|
chronological age (CA) |
|
|
|
|||
|
|
|
|
|
|
|
|
|
GA + CA |
|
CA (days) |
|
Interval |
|
|
|
(weeks) |
|
|
|
(hours) |
|
|
|
|
|
|
|
|
|
|
|
< 29 |
|
0–28 |
|
12 |
|
|
|
|
|
> 28 |
|
8 |
|
|
|
|
|
|
|
|
|
|
|
30–36 |
|
0–14 |
|
12 |
|
|
|
|
|
> 14 |
|
8 |
|
|
|
|
|
|
|
|
|
|
|
37–44 |
|
0–7 |
|
8 |
|
|
|
|
|
> 7 |
|
6 |
|
|
|
|
|
|
|
|
|
|
Dicloxacillin |
Not indicated |
|
6..25–12..5 mg/kg (PO) q6h |
|
|||
|
|
|
|
|
|||
Doxycycline |
Contraindicated |
|
> 45 kg: 100 mg (PO) q12h |
|
|||
|
|
|
|
|
|
≤ 45 kg: 1..1–2..5 mg/kg (PO) q12h |
|
|
|
|
|
|
|
Use only in children > 8 years (unless |
|
|
|
|
|
|
|
RMSF) |
|
|
|
|
|
|
|
1–2 mg/kg (IV) q12–24h |
|
|
|
|
|
|
|
|
|
* Dosages are generally based on weight (mg/kg), up to adult dose as maximum..
‡Do not use in presence of hyperbilirubinemia..

418 |
|
|
A n t i b i o t i c E s s e n t i a l s |
||
|
|
|
|
|
|
Drug |
Dosage in Neonates |
Dosage in Infants/Children* |
|||
|
|
|
|
|
|
Erythromycin |
Chlamydia pneumonitis/conjunctivitis |
10–12..5 mg/kg (PO) q6–8h |
|||
|
or pertussis: 12..5 mg/kg (PO) q6h (E.. |
5–12..5 mg/kg (IV) q6h |
|||
|
estolate preferred) |
|
|
||
|
Other infections: E.. estolate 10 mg/kg |
|
|||
|
(PO) q8h or E.. ethylsuccinate 10 mg/ |
|
|||
|
kg (PO) q6h |
|
|
|
|
|
Severe infections and PO not possible: |
|
|||
|
5–10 mg/kg (IV over ≥ 60 min) q6h |
|
|||
|
|
|
|
|
|
Ertapenem |
Not indicated |
|
15 mg/kg (IV) q12h (not to exceed 1 gm/ |
||
|
|
|
|
|
day) |
|
|
|
|
|
|
Ethambutol |
See p.. 401 |
|
|
See p.. 401 |
|
|
|
|
|
|
|
Ethionamide |
See p.. 401 |
|
|
See p.. 401 |
|
|
|
|
|
|
|
Fluconazole |
Systemic infection or meningitis: 12 |
10 mg/kg (IV or PO) loading dose |
|||
|
mg/kg (IV over 30 min or PO) × 1 dose, |
followed by 12 mg/kg (IV or PO) q24h |
|||
|
then 6 mg/kg/dose (IV or PO) with |
|
|||
|
dosing interval based on gestational |
|
|||
|
age (GA) and chronological age (CA) |
|
|||
|
(below) |
|
|
|
|
|
Prophylaxis (e..g.., extremely low birth |
|
|||
|
weight infants in NICU with high rates |
|
|||
|
of fungal disease): 3 mg/kg/dose (IV |
|
|||
|
or PO) according to dosing interval |
|
|||
|
grid (below) |
|
|
|
|
|
Thrush: 6 mg/kg (PO) × 1 dose, then 3 |
|
|||
|
mg/kg (PO) q24h |
|
|
||
|
|
|
|
|
|
|
GA + CA |
|
CA (days) |
Interval |
|
|
(weeks) |
|
|
(weeks) |
|
|
|
|
|
|
|
|
≤ 29 |
|
0–14 |
72 |
|
|
|
|
> 14 |
48 |
|
|
|
|
|
|
|
|
30–36 |
|
0–14 |
48 |
|
|
|
|
> 14 |
24 |
|
|
|
|
|
|
|
|
37–44 |
|
0–7 |
48 |
|
|
|
|
> 7 |
24 |
|
|
|
|
|
|
|
*Dosages are generally based on weight (mg/kg), up to adult dose as maximum..
|
Chapter 7. Pediatric Infectious Diseases and Pediatric Drug Summaries |
419 |
||
|
|
|
|
|
Drug |
|
Dosage in Neonates |
Dosage in Infants/Children* |
|
|
|
|
|
|
Gentamicin** |
During first week of life dosing is based |
2–2..5 mg/kg (IV or IM) q8h |
|
|
|
on gestational age (administer IV dose |
or |
|
|
|
over 30 min): |
4..5–7..5 mg/kg (IV) q24h |
|
|
|
• |
≤ 29 weeks (or asphyxia, PDA, or |
|
|
|
• |
indomethacin): 5 mg/kg (IV) q48h |
|
|
|
30–33 weeks: 4..5 mg/kg (IV) q48h |
|
|
|
|
• |
34–37 weeks: 4 mg/kg (IV) q36h |
|
|
|
• |
≥ 38 weeks: 4 mg/kg (IV) q24h |
|
|
After first week of life: Initial dose of 4 mg/kg, then draw serum
concentrations 30 min after end of infusion (peak) and 12–24 hours later (trough) to determine dosing interval.. Aim for peak of 5–12 mcg/mL and trough of 0..5–1 mcg/mL
Imipenem |
20–25 mg/kg (IV) q12h |
15–25 mg/kg (IV or IM) q6h |
|
|
|
Iodoquinol |
No information |
10–13..3 mg/kg (PO) q8h |
|
|
|
Isoniazid |
See p.. 401 |
See p.. 401 |
|
|
|
Linezolid |
10 mg/kg (IV) q12h |
10 mg/kg (IV) q8h |
|
|
|
Liposomal/ |
1–5 mg/kg (IV over 2 hours) q24h |
3–6 mg/kg (IV) q24h |
lipid complex |
|
|
Amphotericin |
|
|
preparations |
|
|
|
|
|
Meropenem |
20 mg/kg (IV) q12h |
10 mg/kg (IV) q8h (skin); 20 mg/kg (IV) |
|
|
q8h (intraabdominal); 40 mg/kg (IV) q8h |
|
|
(meningitis) |
|
|
|
Methenamine |
Not indicated |
15–25 mg (PO) q6–8h |
mandelate |
|
|
|
|
|
Metronidazole |
15 mg/kg (IV or PO) × 1 dose, then 7..5 |
5–12..5 mg/kg (PO) q8h |
|
mg/kg/dose (IV or PO) with dosing |
15 mg/kg (IV) × 1 dose followed by |
|
interval based on gestational age (GA) |
7..5 mg/kg (IV) q6h |
|
and chronological age (CA): |
|
*Dosages are generally based on weight (mg/kg), up to adult dose as maximum..
**Drug can be given IM but absorption may be variable..

420 |
|
A n t i b i o t i c E s s e n t i a l s |
|||
|
|
|
|
|
|
Drug |
Dosage in Neonates |
Dosage in Infants/Children* |
|||
|
|
|
|
|
|
|
GA + CA |
CA (days) |
|
Interval |
|
|
(weeks) |
|
|
(hours) |
|
|
|
|
|
|
|
|
≤ 29 |
0–28 |
|
24 |
|
|
|
> 28 |
|
48 |
|
|
|
|
|
|
|
|
30–36 |
0–14 |
|
24 |
|
|
|
> 14 |
|
12 |
|
|
|
|
|
|
|
|
37–44 |
0–7 |
|
24 |
|
|
|
> 7 |
|
12 |
|
|
|
|
|
|
|
Micafungin |
10 mg/kg (IV) of q24h |
|
4–12 mg/kg (IV) q24 (higher dose for |
||
|
|
|
|
|
patients < 8 year of age |
|
|
|
|
||
Mupirocin |
Not indicated |
|
Nasal cream: ½ of single use tube into |
||
|
|
|
|
|
nostril q12h × 5 days; |
|
|
|
|
|
Cream: apply q8h × 5–10 days |
|
|
|
|||
Nafcillin |
25–50 mg/kg/dose (IV).. See ampicillin |
12..5–50 mg/kg (IV or IM) q6h |
|||
|
for dosing interval (p.. 415) |
|
|
||
|
|
|
|
||
Nitazoxanide |
Not applicable |
|
Children 1–3 years old: 100 mg (PO) |
||
|
|
|
|
|
q12h; children 4–11 years old: 200 mg |
|
|
|
|
|
(PO) q12h |
|
|
|
|
||
Nitrofurantoin |
Not indicated |
|
UTI: 1..25–1..75 mg/kg (PO) q6h |
||
|
|
|
|
|
UTI prophylaxis: 1–2 mg/kg (PO) q24h |
|
|
|
|||
Nystatin |
Oral: 1 mL (preterm) to 2 mL (term) of |
Suspension: 4–6 mL swish and swallow |
|||
|
100,000 U/mL suspension applied with |
4×/day |
|||
|
swab to each side of mouth q6h until 3 |
Troche: 1–2 troches 4–5×/ day |
|||
|
days after resolution of lesions |
|
|||
|
Topical: Apply ointment or cream to |
|
|||
|
affected area q6h until 3 days after |
|
|||
|
resolution of lesions.. |
|
|
||
|
|
|
|||
Oxacillin |
25–50 mg/kg/dose (IV).. See ampicillin |
25–50 mg/kg (IV or IM) q6h |
|||
|
for dosing interval (p.. 415) |
|
|
||
|
|
|
|
||
Paromomycin |
Not applicable |
|
10 mg/kg (PO) q8h |
||
|
|
|
|||
Penicillin G |
25,000–50,000 IU/kg/dose (IV).. See |
12,500–75,000 U/kg (IV or IM) q4–6h |
|||
|
ampicillin for dosing interval (p.. 415) |
|
|||
|
Meningitis: 75,000–100,000 IU/kg |
|
|||
|
|
|
|
|
|
*Dosages are generally based on weight (mg/kg), up to adult dose as maximum..

|
Chapter 7. Pediatric Infectious Diseases and Pediatric Drug Summaries |
421 |
|
|
|
|
|
Drug |
Dosage in Neonates |
Dosage in Infants/Children* |
|
|
|
|
|
|
(IV) in meningitis (IV)..† Q8–12h based |
|
|
|
on GA + CA, See ampicillin for dosing |
|
|
|
interval (p.. 415).. Crystalline penicillin G: |
|
|
|
IM: procaine penicillin G q24 hours.. |
|
|
|
Congenital syphilis: Aqueous penicillin |
|
|
|
G 50,000 IU/kg (slow IV push) q12h ×7 |
|
|
|
days, then q8h to complete 10–14 days |
|
|
|
or procaine penicillin G 50,000 IU/kg |
|
|
|
(IM) q24h ×10–14 days |
|
|
|
|
|
|
Penicillin V |
Not indicated |
6..25–12..5 mg/kg (PO) q6-8h |
|
|
|
|
|
Piperacillin |
50–100 mg/kg/dose (IV or IM).. |
25–75 mg/kg (IV or IM) q6h; may increase |
|
|
See ampicillin for dosing interval (p.. |
to q4h in severe infection, especially with |
|
|
415) |
pseudomonas |
|
|
|
|
|
Piperacillin- |
Not indicated |
100–300 mg/kg/day (IV) (of piperacillin |
|
tazobactam |
|
component) divided q6-8h |
|
|
|
|
|
Pyrazinamide |
See p.. 401 |
See p.. 401 |
|
|
|
|
|
Quinupristin/ |
No information |
7..5 mg/kg (IV) q12h |
|
dalfopristin |
|
|
|
|
|
|
|
Rifampin |
10–20 mg/kg (PO) q24h or 5–10 mg/ |
20 mg/kg (PO) q24h or 10 mg/kg (PO) |
|
|
kg (IV) q24h |
q12h |
|
|
|
10–20 mg/kg/day (IV) divided q12–24h |
|
|
|
|
|
Streptomycin |
See p.. 401 |
See p.. 401 |
|
|
|
|
|
Sulfisoxazole |
Contraindicated |
30–35 mg/kg (PO) q6h |
|
|
|
Otitis media prophylaxis: 37..5 mg/kg |
|
|
|
(PO) q12h |
|
|
|
|
|
Tetracycline |
Contraindicated |
5–12..5 mg/kg (PO) q6h.. Use only in |
|
|
|
children > 8 years |
|
|
|
|
|
Ticarcillin |
75–100 mg/kg/dose (IV).. See ampicillin |
25–75 mg/kg (IV or IM) q6h |
|
|
for dosing interval (p.. 415) |
|
|
|
|
|
|
Ticarcillin- |
75–100 mg/kg/dose (of ticarcillin |
25–75 mg/kg (of ticarcillin component) |
|
clavulanate |
component) (IV).. See ampicillin for |
(IV or IM) q6h |
|
|
dosing interval (p.. 415) |
|
|
|
|
|
|
Tinidazole |
Not applicable |
50–60 mg/kg (PO) q24h |
|
|
|
|
|
Tobramycin |
Same as gentamicin (p.. 419) |
2–2..5 mg/kg (IV or IM) q8h or 4..5–7..5 mg/ |
|
|
|
kg (IV) of q24h |
|
|
|
|
|
*Dosages are generally based on weight (mg/kg), up to adult dose as maximum..

422 |
|
A n t i b i o t i c |
E s s e n t i a l s |
||
|
|
|
|
|
|
Drug |
Dosage in Neonates |
|
Dosage in Infants/Children* |
||
|
|
|
|
|
|
Trimethoprim- |
Contraindicated |
|
|
UTI: 4–5 mg/kg (of trimethoprim |
|
sulfameth- |
|
|
|
|
component) (PO) q12h |
oxazole |
|
|
|
|
Pneumocystis carinii pneumonia (PCP) |
(TMP–SMX) |
|
|
|
|
5 mg/kg (PO) q6h (typically after initial |
|
|
|
|
|
IV therapy) |
|
|
|
|
|
UTI prophylaxis: 2–4 mg/kg (PO) q24h |
|
|
|
|
|
IV dosing |
|
|
|
|
|
PCP or severe infection: 5 mg/kg (of |
|
|
|
|
|
trimethoprim component) (IV) q6h |
|
|
|
|
|
Minor infections: 4–6 mg/kg (of |
|
|
|
|
|
trimethoprim component) (IV) q12h |
|
|
|
|
|
|
Vancomycin |
Bacteremia: 10 mg/kg/dose (IV) |
|
10–20 mg/kg (IV) q6h |
||
|
Meningitis: 15 mg/kg/dose (IV).. |
|
|
||
|
Administer IV dose over 60 min.. |
|
|
||
|
Dosing interval is based on gestational |
|
|||
|
age (GA) and chronological age (CA): |
|
|||
|
|
|
|
|
|
|
GA + CA |
CA (days) |
Interval |
|
|
|
(weeks) |
|
(weeks) |
|
|
|
|
|
|
|
|
|
≤ 29 |
0–14 |
18 |
|
|
|
|
> 14 |
12 |
|
|
|
|
|
|
|
|
|
30–36 |
0–14 |
12 |
|
|
|
|
> 14 |
8 |
|
|
|
|
|
|
|
|
|
37–44 |
0–7 |
12 |
|
|
|
|
> 7 |
8 |
|
|
|
|
|
|
|
|
Voriconazole |
Not applicable |
|
|
7 mg/kg (IV) q12h |
|
|
|
|
|
|
8 mg/kg (PO) q12h × 1 day, then 7 mg/ |
|
|
|
|
|
kg (PO) q12h |
|
|
|
|
|
|
*Dosages are generally based on weight (mg/kg), up to adult dose as maximum..
