
Учебники / Textbook and Color Atlas of Salivary Gland Pathology - DIAGNOSIS AND MANAGEMENT Carlson 2008
.pdf
176 Tumors of the Parotid Gland
Figure 8.3e. Histopathology confirms diagnosis of pleomorphic adenoma. Note marked pseudocapsule of collagenous tissue. The patient is disease free 10+ years post-surgery.
adenoma (53%) and intra-parotid lymph node (36%). Malignant salivary gland tumors with the highest false negative rate were acinic cell carcinoma (49%), low-grade mucoepidermoid carcinoma (43%), and adenoid cystic carcinoma (33%). It was felt the data confirmed the difficulty inherent in FNAB of salivary glands (Hughes, Volk, and Wilbur 2005). A paper from the Memorial Sloan Kettering Cancer Center concluded that an FNAB result positive for a malignant neoplastic process is generally predictive of the final histologic diagnosis, whereas the predictive value of a negative FNAB is low (Cohen, Patel, and Lin et al. 2004).
Surgical Management
The basic surgical procedure is the superficial parotidectomy in which the superficial lobe of the parotid is removed, preserving the facial nerve unless it is directly infiltrated by the tumor. The author’s usual incision is the modified Blair or “lazy S.” The skin flap is elevated in a plane through the subcutaneous fat superficial to the parotid capsule (Figure 8.4). Recently the use of a face lift incision has been advocated to improve esthetic results of the scar (Honig 2005; Meningaud, Bertolus, and Bertrand 2006). These authors have also combined face lift incisions with a separate SMAS (superficial musculoaponeurotic system) dissection to eliminate hollowing and reduce Frey’s syndrome. Concerns regarding access to anteriorly sited tumors when using a face lift approach for
parotidectomy do not appear to be borne out in anatomic studies (Nouraei, Al-Yaghchi, and Ahmed et al. 2006) (Figures 8.5 and 8.6).
Once the skin flap is elevated, the sternocleidomastoid muscle (SCM) is identified with the overlying greater auricular nerve, whose branch to the earlobe may be preserved if it does not compromise tumor resection (Figure 8.4e). The anterior border of the SCM is dissected free of the posterior parotid gland, which is retracted anteriorly. Deeper dissection at the superior end of the SCM will allow identification of the posterior belly of the digastric muscle. The facial nerve trunk lies 4 mm superior to the digastric and at the same depth and is an important landmark. Next, attention is turned to the preauricular region with sharp and blunt dissection down the cartilage of the external auditory meatus to the bony portion of the meatus. A strip of parotid tissue remains, which separates the cervical from the preauricular dissection, and this tissue is carefully dissected away to the depth of the digastric muscle. Some troublesome bleeding has to be controlled with bipolar diathermy under direct vision superficial to where the facial nerve will be identified. The facial nerve trunk can be confirmed with a nerve stimulator and the nerve branches are dissected out peripherally to mobilize and remove the superficial parotid. It is usually best to dissect either the frontal or mandibular branches first, depending on the site of the tumor, and then proceed stepwise inferiorly or superiorly dissecting the branches in order and staying superficial to the nerves.
If the tumor directly overlies the facial nerve trunk, making it impossible to access safely, then the peripheral branches can be identified and followed backward as a retrograde parotidectomy, although this is more tedious. The mandibular branch of the facial nerve, where it crosses the anterior facial vein or the buccal branch with its close relationship to the parotid duct (Pogrel, Schmidt, and Ammar 1996), can be found initially. Despite a 66% incidence of weakness 1 week postparotidectomy, normal facial nerve function was present in 99% of 136 retrograde parotidectomies in one series (O’Regan et al. 2007).
In tumors of the deep lobe it is usually necessary to undertake a total parotidectomy. The superficial parotidectomy is performed, preserving the facial nerve and dissecting the superficial lobe from superiorly so that it remains attached to the deep lobe inferiorly and at the tail. Most deep lobe

Figure 8.4c. CT scan of left parotid showing superfi cial lobe tumor.
a
b
Figures 8.4a and 8.4b. Patient with pleomorphic adenoma |
Figure 8.4d. Modifi ed Blair incision. |
of the left parotid gland preoperatively. |
|
177

Figure 8.4e. Skin fl ap raised, the instrument indicates the sensory branch of the greater auricular nerve to the ear, which was preserved in this case.
Figure 8.4f. The parotidectomy has been commenced from inferiorly and the superficial lobe is being retracted superiorly. The arrow indicates the deep surface of the tumor, which was adjacent to the nerve bifurcation (seen inferior to the tumor) and has no normal parotid tissue covering the tumor capsule.
Figure 8.4g. The surgical specimen is seen with the tumor superiorly with no good surrounding “cuff” of tissue.
Figure 8.4h. The surgical site post-parotidectomy with complete dissection of the facial nerve.
Figure 8.4i. A free abdominal fat graft is placed to reduce “hollowing,” which was a concern of the patient.
178

j |
k |
|
Figures 8.4j and 8.4k. Six months postoperatively. |
a |
b |
|
Figures 8.5a and 8.5b. Preoperative facial views of patient with left parotid pleomorphic adenoma. Patient requests bilateral |
|
face lift at the same time as parotidectomy. |
179

Figure 8.5c. Surgical access through face lift incision running into occipital hair line. Arrow shows facial nerve trunk being dissected.
d |
e |
|
Figures 8.5d and 8.5e. Six months postoperatively. Notice absence of neck incision. (Aesthetic portions of this case |
|
undertaken by Dr. A. Pazoki, DDS, MD.) |
180

Figure 8.6a. Preauricular portion of omega face lift incision for parotidectomy for benign cystic lesion in the retromandibular portion of the superficial lobe of the left parotid gland.
Figure 8.6c. A partial parotidectomy of the retroauricular portion of the superficial lobe is almost completed. The specimen is pedicled to the remains of the parotid tail.
Figure 8.6e. The patient 3 months postoperatively with no visible scar.
Figure 8.6b. Post-auricular portion of omega incision runs in the post-auricular sulcus.
Figure 8.6d. Close-up of the dissection. Arrow points to the mandibulo-cervical trunk, which was the only branch of the facial nerve that was dissected, as it crosses superficial to the retromandibular vein.
181

182 Tumors of the Parotid Gland
tumors will be retromandibular and lie inferior to the trunk of the nerve. The space inferiorly is larger and by gentle retraction of the nerve trunk and blunt dissection around the tumor it can usually be delivered into the neck. In larger tumors the neoplasm may be impacted between the mandible and the mastoid with no means of mobilizing it without either dislocating the mandible forward or a subsigmoid or “C” osteotomy to give more space. As contemporary surgery has evolved, more emphasis has been placed on reducing morbidity. Deep lobe tumors may be removed without removing the superficial lobe but leaving it attached anteriorly and then replacing it after excising the deep lobe tumor (Coleela et al. 2007). This technique preserves facial contour and 84% of glandular function compared to the contralateral parotid.
In those tumors with parapharyngeal extension, blind finger enucleation may lead to capsular rupture or cause brisk hemorrhage. In order to visualize and safely remove these tumors an osteotomy of the mandible with or without lip split is utilized (Kolokythas, Fernandes, and Ord 2007) (Figures 8.7 and 8.8).
There is currently a controversy among surgeons regarding superficial parotidectomy or extracapsular dissection. This important topic will be discussed below in the section on pleomorphic adenomas.
Figure 8.7b. Standard lip split incision for mandibulotomy.
Figure 8.7a. MR shows parapharyngeal pleomorphic |
Figure 8.7c. Mandible is retracted out of the field and the |
adenoma. |
pleomorphic adenoma is dissected preserving the overly- |
|
ing lingual nerve. |

Figure 8.8a. Deep lobe parotid tumor with parapharyngeal extension presenting as a palatal mass.
b |
c |
Figures 8.8b and 8.8c. Axial and coronal CT scans show the tumor in the lateral pharyngeal space.
183

Figure 8.8d. The mandible is accessed via a cervical incision from mastoid to chin without lip split. Subsigmoid osteotomy cut marked with saw through buccal cortex only (arrows) and plate has been applied prior to completing the osteotomy.
Figure 8.8e. Osteotomy marked with a saw through the buccal cortex (long arrow) anterior to the mental nerve (short arrow). Two miniplates applied prior to completing the osteotomy.
Figure 8.8f. The plates are removed, the double osteotomy is completed, and the osteotomized hemimandible is retracted upward and rotated to expose the lateral pharyngeal space, and the tumor is being delivered under direct vision.
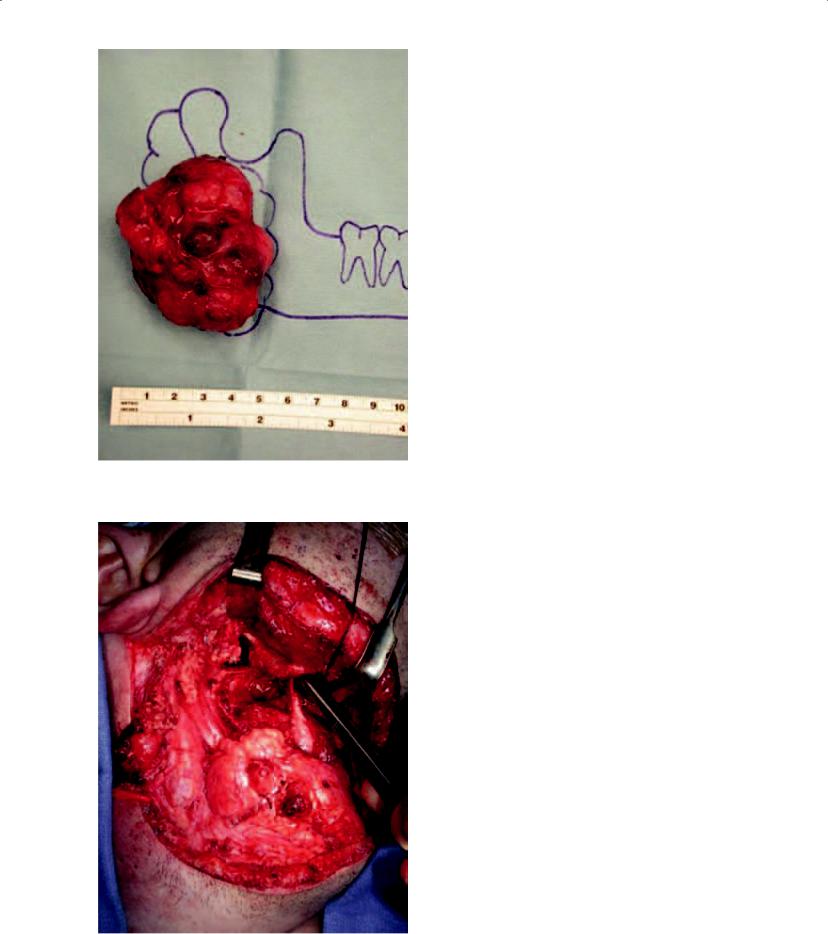
Figure 8.8g. The final specimen, which was PA, seen in relation to the mandible.
Figure 8.8h. The post-resection tumor bed. The plates are reapplied to reconstruct the original position of the mandible and occlusion.
185
