
Учебники / Textbook and Color Atlas of Salivary Gland Pathology - DIAGNOSIS AND MANAGEMENT Carlson 2008
.pdf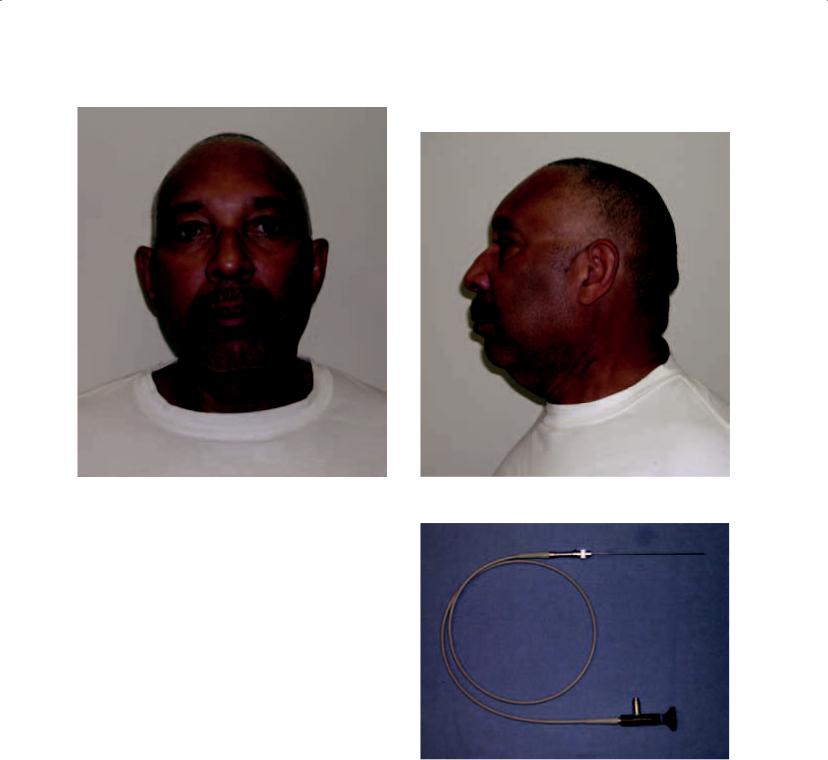
76 Infections of the Salivary Glands
e |
f |
|
Figures 3.6e and 3.6f. At 2 months postoperatively he showed resolution of the disease. |
CHRONIC (RECURRENT OR REFRACTORY) BACTERIAL PAROTITIS
Chronic bacterial parotitis occurs in at least three clinical settings. The first is one in which the patient defers evaluation such that the condition has persisted for at least 1 month. The second includes the setting in which acute bacterial parotitis was managed conservatively but without resolution (refractory sialadenitis). Finally, it is possible for an untreated parotitis to become recurrent such that periods of remission separate recurrent episodes of ABP. The parotid gland may demonstrate evidence of latent infection despite clinical resolution of the disease. The result is scarring in the gland such that function is impaired. Histology will show dilation of glandular ducts, abscess formation, and atrophy (Patey 1965). Pus is rarely observed in chronic bacterial parotitis (Baurmash 2004). Rather, there is a marked reduction of salivary flow, and the parotid secretions are viscous and milky in appearance. The microbiologic etiology of chronic bacterial parotitis is most commonly streptococci and staphylococci, but other organisms may be found as a function of the patient’s immune status, the setting in which the parotitis originally occurred, and medical comor-
Figure 3.7a. The miniature endoscope for diagnostic and interventional sialoendoscopic procedures (Karl Storz Endoscopy-America, Inc., Culver City California). The instrumentation seen here is utilized for diagnostic procedures only. The endoscope may be connected to an operating sheath for interventional procedures (see chapter 5).
bidity. It has been suggested that the accumulation of a semisolid material that obstructs the parotid duct is the culprit in chronic bacterial parotitis (Baurmash 2004). The clinical course of the disease shows pain and swelling waxing and waning.

Figure 3.7b. A series of duct dilators are sequentially |
Figure 3.7d. A representative image is noted that demon- |
inserted into Stenson’s duct prior to placing the |
strates normal findings in a patient with chronic parotid |
sialoendoscope. |
pain. The sialoendoscopy procedure, including dilatation |
|
and irrigation of the duct, resulted in resolution of |
|
symptoms. |
Figure 3.7c. The sialoendoscope placed into Stenson’s duct.
77

78 Infections of the Salivary Glands
Treatment of Chronic Bacterial Parotitis
Treatment of chronic bacterial parotitis centers on palliative therapy with parotidectomy reserved as a last resort. Effective treatment is centered on the gland inflammation as well as the precipitated intraductal material. Patients should be treated with culture specific systemic antibiotics, ductal antibiotic irrigations during periods of remission,
a
b
Figures 3.8a and 3.8b. A 35-year-old man with a 2-year history of left parotid pain and swelling.
analgesics, and avoidance of dehydration and antisialogogue medications (Goldberg and Bevilacqua 1995). Sialoendoscopy represents a technique that may obviate the need for aggressive surgical intervention (Hasson 2007; Nahlieli et al. 2006). Sialoendoscopic findings of patients with chronic obstructive parotitis include ductal stricture, mucous plugs, and desquamative epithelial cells
Figure 3.8c. Computerized tomograms showed sclerosis of the parotid parenchyma as well as a suspected abscess. The patient underwent left superficial parotidectomy with a clinical and radiographic diagnosis of chronic bacterial parotitis with abscess formation.
Figure 3.8d. The superficial parotidectomy was accessed with a standard incision.

e
f
Figures 3.8e and 3.8f. A nerve-sparing approach was followed (e) that allowed for delivery of the specimen (f).
Figure 3.8g. Histopathology showed chronic sialadenitis with abscess formation.
h
i
Figures 3.8h and 3.8i. At 3 years postoperatively he displays resolution of the disease.
79

80 Infections of the Salivary Glands
and inflammatory cells (Qi, Liu, and Wang 2005). A sialoendoscopic procedure may address any or all of these problems, thereby sparing the gland (Figure 3.7). If pain and swelling become intolerable for the patient, or if special imaging studies reveal abscess formation in the parotid gland, then nerve-sparing parotidectomy is the treatment of choice (Figure 3.8).
CHRONIC RECURRENT
JUVENILE PAROTITIS
Recurrent juvenile parotitis is commonly noted prior to puberty and is manifested by numerous episodes of painful enlargements of the parotid gland. Chronic recurrent parotitis in children is ten times more common than chronic recurrent parotitis in adults (Baurmash 2004). Several etiologies have been offered including congenital abnormalities or strictures of Stenson’s duct, trauma, foreign bodies within the duct, or a history of viral mumps. Many cases will resolve prior to the onset of puberty such that conservative measures are recommended. These include long-term antibiotics and analgesia. Spontaneous regeneration of salivary function has been reported (Galili and Marmary 1985).
BARTONELLA HENSELAE (CAT SCRATCH DISEASE)
Cat scratch disease (CSD) is a granulomatous lymphadenitis that most commonly results from cutaneous inoculation caused by a scratch from a domestic cat. The causative microorganism is Bartonella henselae, a Gram-negative bacillus. Approximately 90% of patients who have cat scratch disease have a history of exposure to cats, and 75% of these patients report a cat scratch or bite (Arrieta and McCaffrey 2005). Dogs have been implicated in 5% of these cases. This disease process begins in the preauricular and cervical lymph nodes as a chronic lymphadenitis and may ultimately involve the salivary glands, most commonly the parotid gland by contiguous spread (English, Wear, and Margileth et al. 1988).
The diagnosis of CSD has changed with advances in serologic and molecular biologic techniques. These methods have replaced the need for the Rose Hanger skin test previously used. Testing for the presence of antibodies to Bartonella henselae
is now the most commonly used test to confirm the diagnosis. The two methods used for antibody detection are the indirect fluorescent antibody (IFA) and the enzyme immunoassay (EIA). When tissue is removed for diagnosis, histologic examination might demonstrate bacilli with the use of Warthin-Starry staining or a Steiner stain. Lymph node involvement shows reticular cell hyperplasia, granuloma formation, and occasionally a stellate abscess.
In most cases, no active therapy is required. The patient should be reassured that the lymphadenopathy is self-limited and will spontaneously resolve in 2–4 months. Antibiotic therapy is indicated when patients are symptomatic. Antibiotics reported to be most effective include rifampin, erythromycin, gentamycin, azithromycin, and ciprofloxacin. Surgery becomes necessary when the diagnosis is equivocal, or when incision and drainage is indicated (Figure 3.9).
Figure 3.9a. A 21-year-old woman with a 2-week history of left submandibular pain and swelling. A history of animal scratch was provided.

Figure 3.9b. Computerized tomograms revealed a mass of the left submandibular gland. The patient was taken to the operating room, where excision of the submandibular gland and mass was performed.
c
d
Figures 3.9c and 3.9d. Wide access was afforded (c) and the mass was exposed (d).
Figure 3.9e. The specimen.
Figure 3.9f. Histopathology showed a stellate abscess.
Figure 3.9g. A Steiner stain showed Bartonella (gram negative bacillus).
81

82 Infections of the Salivary Glands
h |
i |
Figures 3.9h and 3.9i. Her disease resolved without long-term antibiotics as seen in 5-year postoperative images.
ACUTE BACTERIAL SUBMANDIBULAR SIALADENITIS (ABSS)
Acute bacterial submandibular sialadenitis is usually associated with physical obstruction of Wharton’s duct. Since sialolithiasis, the likely cause of obstruction of the duct, is discussed in chapter 5, it is only briefly mentioned here. Suffice it to say that the submandibular ductal system is prone to stone formation. The common features of ABSS are swelling in the submandibular region associated with prandial pain. ABSS is a community acquired disease that less frequently is associated with dehydration and hospitalization as compared to ABP. Purulence may be expressed from the opening of Wharton’s duct, but in many cases complete obstruction to pus and saliva occurs.
Treatment of ABSS
Treatment of ABSS consists of antibiotic therapy, hydration, avoidance of anti-sialogogues, and removal of a sialolith, if one is identified. Empiric antibiotics used to treat ABSS are similar to ABP, including an extended-spectrum penicillin, a firstgeneration cephalosporin, clindamycin, or a macrolide. Patients are also encouraged to use sialogogues, such as sour ball candies.
CHRONIC RECURRENT SUBMANDIBULAR SIALADENITIS
Chronic recurrent submandibular sialadenitis usually follows ABSS and is associated with recurrent sialolithiasis. Chronic recurrent submandibular sialadenitis occurs more commonly than chronic

recurrent bacterial parotitis. Initial treatment for chronic recurrent submandibular sialadenitis begins with antibiotic therapy, sialogogues, and hydration. Sialoendoscopic intervention may also be of benefit
Figure 3.10a. A 52-year-old man with a 1-year history of vague discomfort in the left upper neck.
Infections of the Salivary Glands |
83 |
in the treatment of chronic recurrent submandibular sialadenitis prior to subjecting the patient to sialadenectomy. Ultimately, removal of the submandibular gland is often necessary (Figure 3.10).
Figure 3.10c. His diagnosis was chronic submandibular sialadenitis and he was prepared for left submandibular gland excision.
Figure 3.10b. Screening panoramic radiograph showed |
Figure 3.10d. The surgery was carried through anatomic |
no evidence of a sialolith. |
planes, including the investing layer of the deep cervical |
|
fascia. |

Figure 3.10e. The dissection is carried deep to this layer since a cancer surgery is not being performed that would require a dissection superficial to the investing fascia. Exposure of the gland demonstrates a small submandibular gland due to scar contracture.
Figure 3.10f. Inferior retraction of the gland allows for identifi cation and preservation of the lingual nerve.
g
h
Figures 3.10g and 3.10h. The specimen (g) is bivalved (h), which allows for the appreciation of scar within the gland.
Figure 3.10i. The resultant tissue bed shows the hypoglossal nerve, which is routinely preserved in excision of the submandibular gland.
84

Infections of the Salivary Glands |
85 |
Figure 3.10j. Histopathology shows a sclerosing siala- |
Figure 3.10k. The patient’s symptoms were eliminated |
denitis. |
postoperatively, and he healed uneventfully, as noted at 1 |
|
year following the surgery. |
TUBERCULOUS MYCOBACTERIAL DISEASE
The most common head and neck manifestation of mycobacterium tuberculosis is infection of the cervical lymph nodes. Tuberculous infection of the salivary glands is generally seen in older children and adults. The infection is believed to originate in the tonsils or gingiva and most commonly ascends to the parotid gland via its duct (Arrieta and McCaffrey 2005). Secondary infection of the salivary glands occurs by way of the lymphatic or hematogenous spread from the lungs. Clinically, tuberculous salivary gland infection presents in two different forms. The first is an acute inflammatory lesion with diffuse glandular edema that may be confused with an acute sialadenitis or abscess. The chronic lesion occurs as a slowgrowing mass that mimics a tumor.
NONTUBERCULOUS
MYCOBACTERIAL DISEASE
Nontuberculous mycobacterial disease has become an important entity in the pediatric population. It has been estimated that greater than 92% of mycobacterial cervicofacial infections in children are a result of nontuberculous mycobacteria (Arrieta and McCaffrey 2005). The disease primarily affects children younger than 5 years of age. The specific organisms are M. Kansasii, M. aviumintracellulare, and M. scrofulaceum. The typical clinical presentation is that of a rapidly enlarging and persistent parotid and/or neck mass that has failed to resolve with antibiotic therapy (Figure 3.11). A characteristic violaceous discoloration to the skin develops. The treatment of choice is surgical removal of the involved salivary gland and associated lymph nodes.
