
Essentials of Orthopedic Surgery, third edition / 05-Children’s Orthopedics
.pdf
5. Children’s Orthopedics |
179 |
20°
15
VARUS 10
AGE |
5 |
|
|
|
|
|
|
|
|
|
|
|
1 |
2 |
3 |
4 |
5 |
6 |
7 |
8 |
9 10 11 12 13 |
||
IN |
0° |
||||||||||
|
|
|
|
|
|
|
|
|
|||
YEARS |
5 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
VALGUS 10
15
20°
FIGURE 5-6. Development of the tibiofemoral angle during growth. (From Tachdjian MO. Pediatric Orthopedics, 2nd ed, vol 1. Philadelphia: Saunders, 1990. Reprinted by permission.)
It is best to record the degree of varus by measuring the number of fingerbreadths accommodated between the child’s knees and the degree of valgus by recording the number of fingerbreadths accommodated between the medial malleoli.
Differential Diagnosis
Recognizing that the vast majority of children with angular patterns are normal and require nontreatment, it is nonetheless important to realize that angular deformities can be a manifestation of pathologic states.
A.Knock-knees (genu valgum) (Fig. 5-7)
1.Physiologic
2.Renal rickets
3.Skeletal dysplasias
4.Trauma
B.Bowlegs (genu varum) (Fig. 5-8)
1.Physiologic
2.Blounts’ disease
3.Rickets (nutritional)
4.Skeletal dysplasias (achondroplasia)
5.Trauma
As one can appreciate from these lists, symmetry is important. Physiologic angular deformity is virtually always symmetrical; the finding of asymmetry should, therefore, suggest a pathologic state and trigger an appropriate workup.
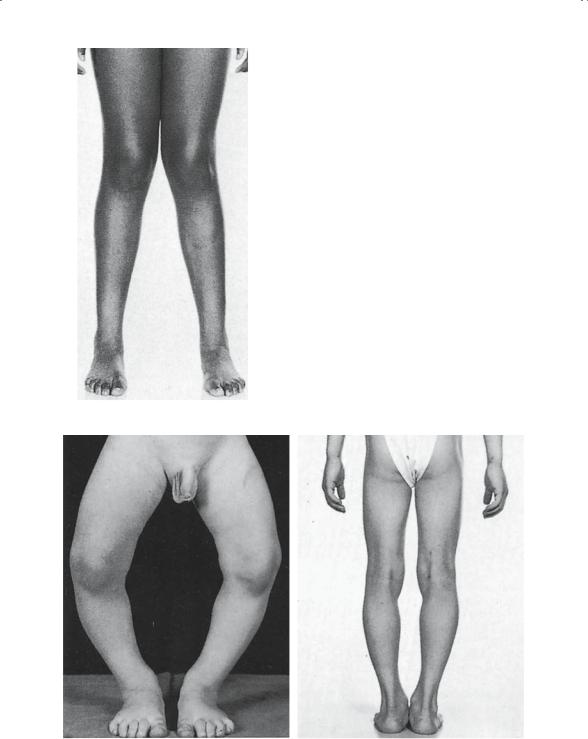
FIGURE 5-7. Bilateral genu valgum in an adolescent. (From Tachdjian MO. Pediatric Orthopedics, 2nd ed, vol 1. Philadelphia: Saunders, 1990. Reprinted by permission.)
A B
FIGURE 5-8. Bilateral genu varum. (A) At age 1.5 years. (B) At 7 years, showing spontaneous correction without treatment. (From Tachdjian MO. Pediatric Orthopedics, 2nd ed, vol 1. Philadelphia: Saunders, 1990. Reprinted by permission.)

5. Children’s Orthopedics |
181 |
General Affectations of the Pediatric Skeleton
Many diseases have skeletal manifestations, which makes it impossible in one short chapter to fully discuss the vast array of pathologic states that have an impact on the musculoskeletal system. Rather, by being introduced to several specific examples in each disease category, one can appreciate some of the general ways in which the skeleton reacts to various insults. Recalling the VITAMIN acronym introduced earlier in the text, we now focus on some of the vascular, infectious, arthritic, metabolic, and neurodevelopmental diseases that produce skeletal manifestations. An entire chapter of this book is devoted to a discussion of tumor and another one to injury; therefore, these concerns are mentioned only insofar as their effects are unique to the growing skeleton.
Infection
Osteomyelitis
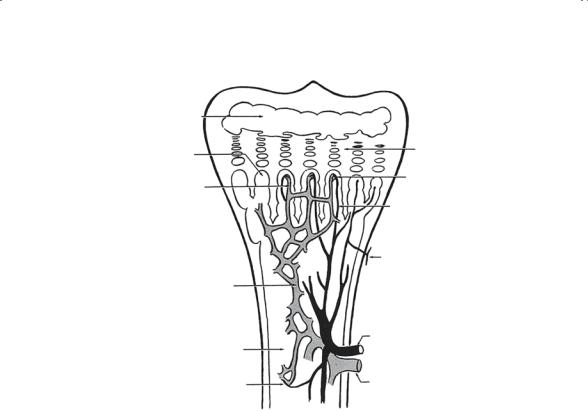
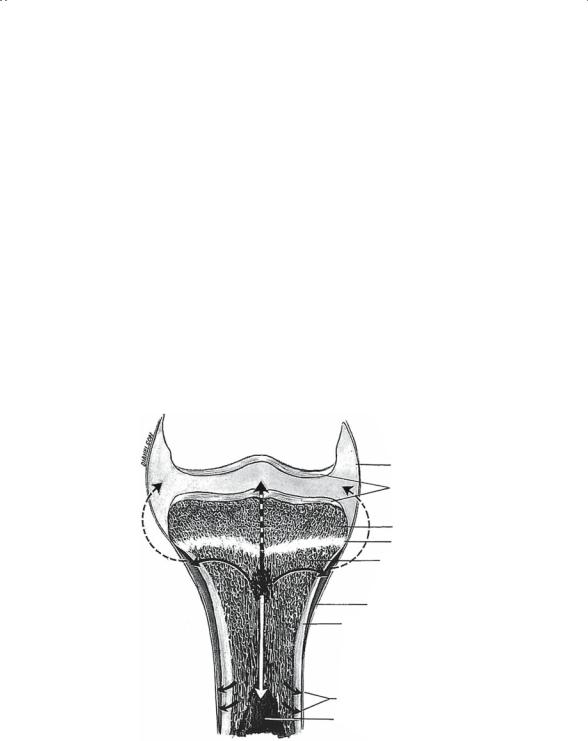
The pediatric skeleton is a prime location for bone and joint infections. In part, this is the result of the many bacterial infections that small children seem to have, hence providing organisms capable of hematogenously spreading from the skin, ear, and nasopharynx. In addition, the unique metaphyseal blood supply (Fig. 5-9) in the child establishes the battlefield for the host–organism interaction. Because the physis creates a barrier to the vessels, they must double back on themselves, thereby forming endloop capillaries and creating an area of stasis in the bony metaphysis. This area of stasis “catches” bacteria as they are showered hematogenously from distant sites. Once entrenched, the bacteria establish a focus of infection, and the classic case of osteomyelitis develops. It is important to recognize that the changes are not simply the result of the damage the bacteria do to the bone, but also the reparative changes initiated by the bone in an effort to localize the infection.
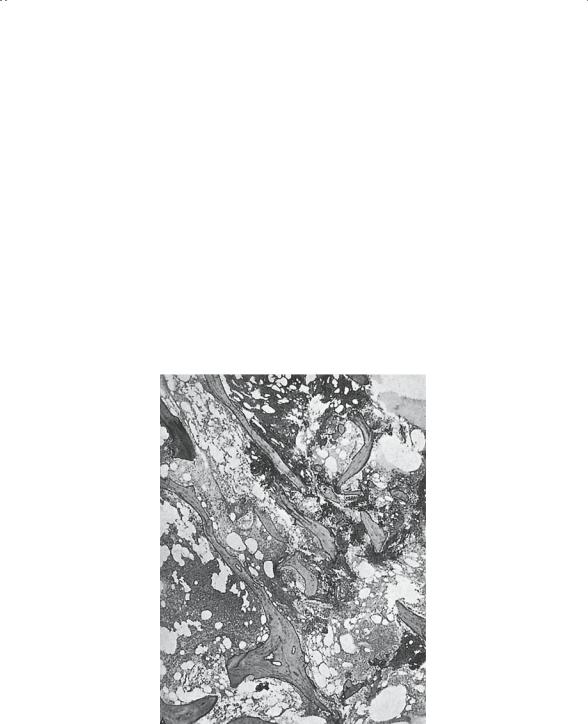
The result of this activity is a mixture of bony destruction by the organisms and new bone formed to wall off the infection and shore up the areas of damage. The dead and dying bony fragments are referred to as “sequestra,” and the new viable bone being formed is called “involucrum” (Fig. 5-10; see also Chapter 3).
Clinical Features
One should inquire about a past history of trauma, as well as infections elsewhere, that may have provided a source for the organism. Occasionally, no such history is available and one is evaluating a child who presents with pain in a limb and fever. The combination of these two findings—pain in an extremity and fever—should be presumed to be osteomyelitis until proven otherwise.
182 J.N. Delahay and W.C. Lauerman
Epiphyseal marrow |
|
|
Primary marrow |
Epiphyseal |
|
cartilage |
||
outgrowths |
||
|
||
Descending limb |
Dilated turning |
|
point |
||
|
Ascending limb of |
|
|
terminal arterial |
|
|
branch |
|
|
Metaphyseal artery |
|
Venous capillary |
|
|
network in marrow |
|
|
|
Nutrient artery |
|
Diaphyseal marrow |
|
|
Transition point |
Nutrient vein |
FIGURE 5-9. Localization of osteomyelitis caused by structure of metaphyseal sinusoids. Diagram of blood supply of long bones in children showing the structure of metaphyseal sinusoids to be the cause for localization of pathogenic bacteria in the metaphysis. (From Tachdjian MO. Pediatric Orthopedics, 2nd ed, vol 1. Philadelphia: Saunders, 1990. Reprinted by permission.)
In children under 1 year of age, the findings may be more nonspecific and poorly localized, for example, irritability, changes in feeding habits, and few signs of sepsis. Pseudoparalysis (failure to use the limb) may be the only localized finding.
Localized physical findings such as swelling, heat, localized tenderness, erythema, and signs of systemic sepsis are frequently seen in the older child.
Diagnosis
Standard laboratory studies usually show an elevated white blood cell (WBC) count and sedimentation rate (ESR). The C-reactive protein (CRP) is similarly elevated. The ESR and CRP are both acute-phase reactants; however, the latter responds more rapidly to the presence of infection and, therefore, tends to be a more sensitive measure of skeletal involvement. X-rays initially may be negative, because it takes 10 days for the pathology to become demonstrable radiographically. Bone resorption and new peri-
5. Children’s Orthopedics |
183 |
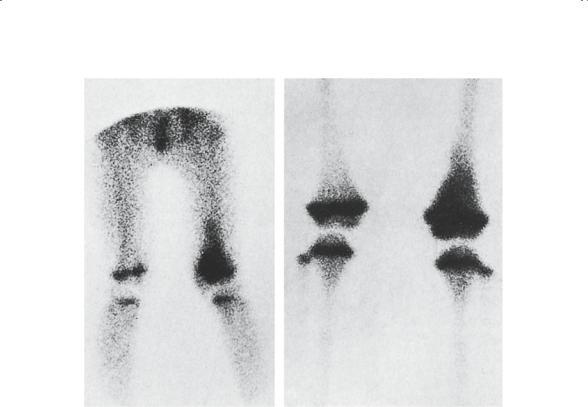
osteal bone formation are the characteristic changes. However, neither of these may be seen initially. A standard total body bone scan is often quite helpful in the evaluation of these children. The bone scan is particularly useful in the localization of pathology (Fig. 5-11).
Appropriate cultures are essential. Blood cultures are reportedly positive in approximately 50% of cases of acute hematogenous osteomyelitis. Source cultures from the throat, ear, skin, etc. should also be obtained. Bony aspiration is essential in the complete evaluation of these children. It is axiomatic that to diagnose a bone infection one must culture the bone. To that end, and using a large-bore needle, one should aspirate at the point of maximal tenderness in an effort to retrieve organisms. Reportedly, aspiration will be positive in approximately 60% of cases. The organisms vary slightly with age, but ordinarily either Staphylococcus aureus or Streptococcus species should be anticipated. In neonates, one needs to consider the possibility of gramnegative organisms.
FIGURE 5-10. Histologic findings in acute osteomyelitis. (A) Necrotic trabeculae of bone surrounded by inflammatory cells (× 25). (From Tachdjian MO. Pediatric Orthopedics, 2nd ed, vol 1. Philadelphia: Saunders, 1990. Reprinted by permission.)
184 J.N. Delahay and W.C. Lauerman
A B
FIGURE 5-11. Scintigraphic findings with technetium-99m in acute diphosphonate of the left distal femoral metaphysis. Note the increased localized uptake.
(A) Early vascular flush. (B) Two hours later. (From Tachdjian MO. Pediatric Orthopedics, 2nd ed, vol 1. Philadelphia: Saunders, 1990. Reprinted by permission.)
Treatment
Diagnosis is critical before initiating antimicrobial treatment. All too often broad-spectrum antibiotics are given before a bacteriologic diagnosis is made. The result is a “partially treated osteomyelitis.” These children present a challenging problem because the classical physical findings tend to be damped or eradicated completely. The problem, however, is that the organisms are frequently not killed; they only await antibiotic withdrawal before initiating a new wave of bony destruction. The principles of management have been established for many years and are best summarized as follows: (1) complete bacteriologic diagnosis; (2) appropriate antibiotic selection; (3) antibiotic delivery by the appropriate route and for the appropriate duration; (4) immobilization to decrease the risk of pathologic fracture; and (5) surgical drainage of abscesses. For many years, the tradition of intravenous antibiotic delivery has been accepted as essential. Although some would argue that the oral route is adequate, the IV route is still considered by most to be the standard mode of delivery despite the inconve-
5. Children’s Orthopedics |
185 |
nience caused to child, family, and physician. The traditional duration of 6 weeks has been altered in some protocols to 3 weeks intravenous and 3 weeks oral based on clinical response.
The indication for surgical drainage is the presence of loculated pus. Typically, this is seen within the metaphysis and/or under the periosteum (Fig. 5-12). These subperiosteal abscesses typically follow breakthrough of the thin cortical bone in the metaphyseal region. As these subperiosteal collections strip the periosteum from the underlying cortex, the cortex is devascularized and segments become avascular. In severe cases of acute hematogenous osteomyelitis, it is not uncommon to see sequestration of the entire bony diaphysis.
Septic Arthritis
Infection of a child’s joint typically results from one of three pathologic mechanisms:
1. Hematogenous spread: just as in osteomyelitis, organisms can localize in the joint, finding the highly vascular synovium a favorable location for replication.
Joint capsule
Articular cartilage
Epiphysis
Epiphyseal line
Cancellous bone of metaphysis
Periosteum
Cortical bone
Haversian canals
Medullary cavity
FIGURE 5-12. Diagram showing spread of acute hematogenous osteomyelitis. The interrupted lines are rare routes. (From Tachdjian MO. Pediatric Orthopedics, 2nd ed, vol 1. Philadelphia: Saunders, 1990. Reprinted by permission.)
186J.N. Delahay and W.C. Lauerman
2.Breakthrough from a metaphyseal osteomyelitis: this occurs in specific joints where a portion of the metaphysis is intraarticular. Anatomically, the synovial reflection extends below the physis and includes a portion of metaphyseal cortical bone. The transverse Volkmann’s canals provide a conduit for pus in the metaphysis to access the joint. In doing so, a secondary septic arthritis results. This phenomenon of breakthrough is most typical in the hip (Fig. 5-13), but it can also occur in the elbow, where the radial head is intraarticular, the shoulder, and the ankle.
3.Penetrating trauma: this results in joint sepsis when organisms are directly injected into the joint.
Clinical Feature
Joint swelling and redness are the typical physical findings that one would expect. Systemic signs of sepsis are also usually readily apparent. In contradistinction to acute hematogenous osteomyelitis, children affected with septic arthritis tend to be more toxic, exhibiting high fevers, listlessness, and poor feeding. In addition, these children resist any attempt to move the involved joint.
Diagnosis
A workup similar to that for osteomyelitis should be carried out and, at the risk of appearing repetitious, one cannot seriously consider this diag-
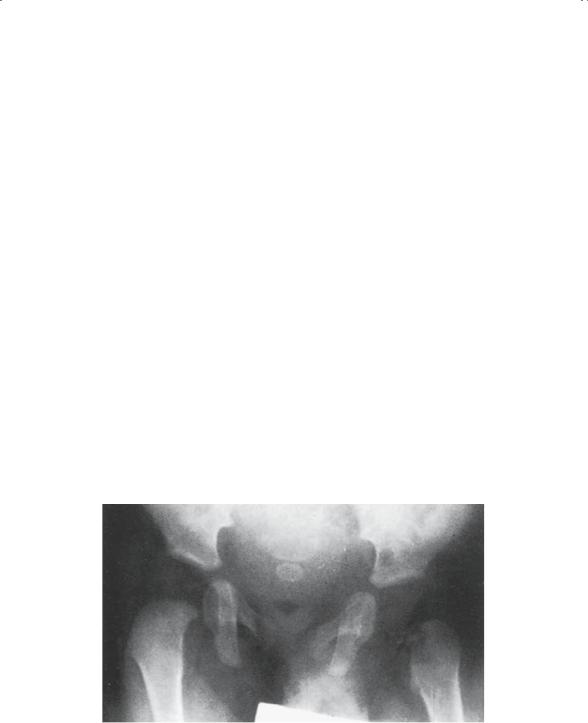
FIGURE 5-13. Septic arthritis of left hip. Lateral subluxation and area of rarefaction in the femoral neck are evident. (From Tachdjian MO. Pediatric Orthopedics, 2nd ed, vol 1. Philadelphia: Saunders, 1990. Reprinted by permission.)

5. Children’s Orthopedics |
187 |
nosis in the differential without having made an attempt to retrieve organisms from the joint. It is important to be sure that the joint is, indeed, being aspirated, and this frequently requires fluoroscopic control, especially if the joint in question is the hip. The pediatric hip is often difficult to enter under the best of circumstances, and radiographic control using an arthrogram is recommended.
Microbiogically, the most common organism retrieved in the child is Staphylococcus aureus. As is the case with osteomyelitis, neonates should be suspected of having unusual organisms including gram negatives. In the adolescent patient, one must never forget the most common cause of septic arthritis: Neisseria gonorrhoeae.
Treatment
Septic arthritis, in contrast to acute hematogenous osteomyelitis, is a surgical emergency. It is imperative that the pus be removed from the joint as soon as possible. The articular cartilage is extremely vulnerable and easily damaged by enzymes, those produced by the microorganisms as well as those produced by the white cells. It is, therefore, NOT enough to simply kill the organisms in the joint. The joint must be rid of all WBCs, bacterial by-products, and enzymes. In most young children, this requires an arthrotomy. Occasionally, in the older child, arthroscopy is an appropriate technique for cleaning out a more-accessible joint such as the knee. Repeated needle aspirations are rarely effective in cleaning the inflamed joint. In addition, repetitive aspiration in the child is yet another example of “man’s inhumanity to man.”
Antibiotic management is similar to that for osteomyelitis. The choice of antibiotic and the route of delivery are usually identical. The duration of administration, however, is frequently shortened. The prognosis for septic arthritis in a child depends on early diagnosis, aggressive drainage, and appropriate antibiotic management. Delay in diagnosis or delay in adequate surgical drainage can have disastrous long-term effects on the joint, typically producing irreversible changes.
Complications of Bone and Joint Infections
Long-term sequelae can result from bacterial damage to these relatively vulnerable tissues (Fig. 5-14). In addition to the bone and articular cartilage, the child has a physis, which is likewise exposed to the insult.
Septic Joint Destruction
Loss of articular cartilage and arthrofibrosis ultimately result in joint contracture, deformity, and occasionally bony ankylosis (fusion). Salvage of the irreparably damaged articulations is difficult at best and frequently impossible.
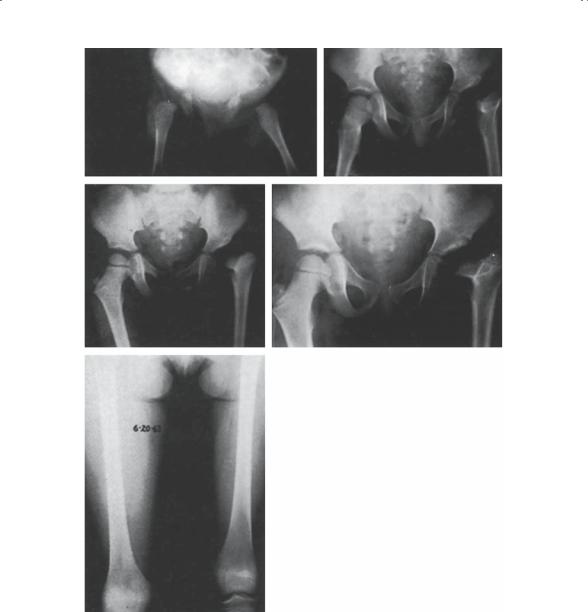
A B
C D
E
FIGURE 5-14. Suppurative arthritis of the left hip in a 3-month-old infant. Onset was at 4 weeks of age. Erroneous diagnosis of fibrocystic disease and thrombophlebitis resulted in a 2-month delay in diagnosis. (A) Radiograms of hips show marked effusion of left hip with lateral subluxation. (B–D) Serial radiograms of hips show failure of ossification of the femoral head (due to avascular necrosis) and the development of coax vara. (E) Teleoradiograms taken 9.5 years after onset of sepsis in left hip. There is a 3.9-cm shortening of the left femur. A subtrochanteric abduction osteotomy was performed 4 years earlier. The left hip has functional range of motion. Skeletal growth of lower limbs is being followed, and the plan is to perform distal femoral epiphyseodesis on the right at the appropriate age. (From Tachdjian MO. Pediatric Orthopedics, 2nd ed, vol 1. Philadelphia: Saunders, 1990. Reprinted by permission.)
188
