
Essentials of Orthopedic Surgery, third edition / 05-Children’s Orthopedics
.pdf
5. Children’s Orthopedics |
199 |
is impossible to recall all the features that define a given dysplastic condition, especially in light of the fact that each is usually quite rare. At best, generalizations can be employed to assist in the diagnosis of a specific patient and thereby guide the appropriate workup and referral to an individual skilled in definitive diagnosis. The anticipated orthopedic problems, treatment, and prognosis will hinge on the diagnosis.
When presented with an individual displaying dysplastic findings, especially short stature, chromosomal evaluation and standard X-rays are good starting points once appropriate history (especially family history) and a careful physical examination have been carried out. The X-rays should include a lateral of the cervical and thoracolumbar spine, an anteroposterior view of the pelvis, and anteroposterior views of the wrists and the knees. These views allow one to evaluate epiphyseal, physeal, metaphyseal, and diaphyseal growth and their aberrations.
Most of the dysplasias tend to affect a specific region of the bone; by assessing each region, clues can be obtained regarding the specific type of dysplasia. For example, spondyloepiphyseal dysplasia affects primarily epiphyseal growth, as the name implies. One should expect to see deformities of the epiphyseal nuclei and disordered apophyseal growth. On the other hand, achondroplasia is a defect in physeal growth and will, therefore, produce significant dwarfing; in fact, it is the most common cause of pathologic short stature.
Most of the skeletal dysplasias are genetically transmitted, and a careful family history will define the pattern. Many, however, are spontaneous mutations or without a defined etiology. It is important to keep in mind that by definition a skeletal dysplasia is a GENERALIZED affectation of the skeleton with all bones showing some changes. Obviously, the end of the bone growing more rapidly demonstrates the defect to a greater degree; thus, the knee and wrist films are more likely to show changes than the hip or elbow views.
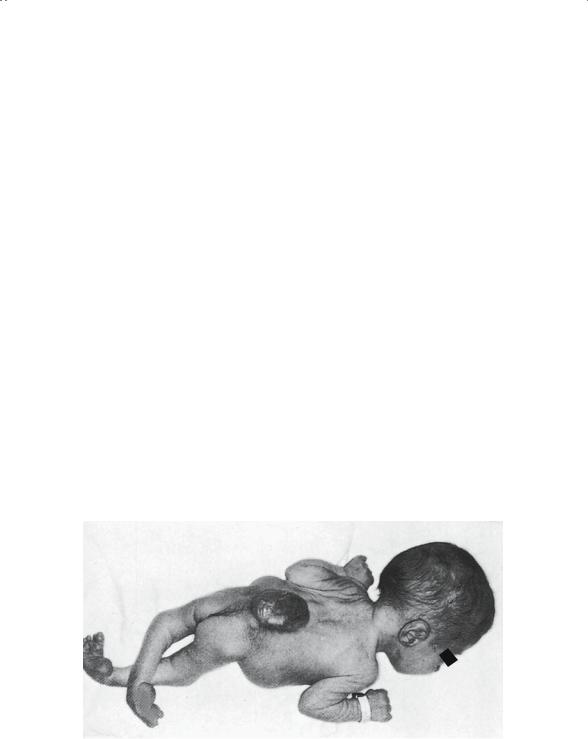
Achondroplasia
As an example of how a dysplasia affects the skeleton, one should consider the most common, achondroplasia. Transmitted as an autosomal dominant in most cases, it is usually apparent at birth. The infant is rhizomelically shortened; that is, the proximal segment of the limbs is relatively shorter than the middle or distal segments (Fig. 5-24). In addition, the child is disproportionately built because the limbs are preferentially involved and, therefore, are very short relative to the spine and trunk.
These children follow the growth curve, but several standard deviations below normal, achieving a mature height between 3 to 4 feet. As with all the true dysplasias, intelligence is not impaired and life expectancy is virtually normal.

200 J.N. Delahay and W.C. Lauerman
A  B
B
FIGURE 5-24. (A) Posterior photograph of achondroplastic dwarf showing distorted growth of long bones. The proximal limb segments are proportionately shorter than the distal, with the hands reaching only to the hip region. The legs are bowed, and the scapulae and pelvis are smaller than normal. Scoliosis is uncommon. (B) Lateral photograph of child with achondroplasia. Note marked lumbar lordosis with prominent buttocks as a result of pelvic tilt. The lordosis is caused in part by differential growth of vertebral body versus posterior elements. (From Bogumill GP. Orthopaedic Pathology: A Synopsis with Clinical Radiographic Correlation. Philadelphia: Saunders, 1984. Reprinted by permission.)
Clinical Features
The child’s head shows flattening of the nasal bridge and prominent frontal bones. Both findings result from the disparity between the normal intramembranous calvarial growth and the retarded enchondral growth of the basilar portions of the skull.

5. Children’s Orthopedics |
201 |
The extremities are short, with each of the bones being short in length, but relatively normal in girth, because periosteal bone formation remains relatively unaffected. The spine and pelvis also show some decrease in height, but of greater significance is the decrease in the interpedicular distance, which effectively creates a spinal stenotic syndrome; this, coupled with a hyperlordotic lumbar spine, creates many achondroplasts to develop disk symptoms at an early age.
The major problem of the older adolescent is obesity, which complicates many of the other abnormalities. As adults, multiple tendonitis and bursitis problems are commonplace.
Neuromuscular Disease
In contrast to the skeletal dysplasias, which are intrinsic abnormalities of the skeleton, this group of diseases is extrinsic, but drastically alter the normal skeleton, primarily by the muscle imbalance they create.
Common themes can be seen that emphasize the fact that the problem is disparity in the agonist–antagonist relationship. Major joints tend to dislocate, with the hip being a prime example. The flexor pattern tends to become dominant, causing the femoral head to dislocate posteriorly. Scoliosis should be expected as asymmetry of spinal muscle action alters normal balance. If the neurologic defect is asymmetrical, as in polio, then the growth plates in one leg will “feel” a different muscle pull than those of the other, and a leg-length discrepancy can be anticipated.
Cerebral Palsy
Cerebral palsy is a static neurologic disease of children caused by an insult to the immature brain during the perinatal period. The defect is, therefore, central, damaging the normal inhibitory influences on the peripheral gamma efferent system. Without central damping, the peripheral reflex arc functions autonomously, and the result is increased tone or spasticity.
Cerebral palsy is classified in one of two ways:
1.Physiologic classification
a.Spastic: Hypertonia, hyperflexia, and contractures are seen. This is the most common form of the syndrome.
b.Athetoid: This is far less common today than it was in years past. Rh incompatibility and erythroblastosis fetalis were a common etiology of this form.
c.Rigid
d.Ballismic
e.Mixed

202 J.N. Delahay and W.C. Lauerman
FIGURE 5-25. Spastic quadriplegia with total body involvement. At 4 years of age. The marked scissoring of the hips and equinus deformity of the ankles provide a poor base upon which balance can develop. Note the pes valgus. (From Tachdjian MO. Pediatric Orthopedics, 2nd ed, vol 1. Philadelphia: Saunders, 1990. Reprinted by permission.)
2.Geographic classification
a.Hemiplegia: The most common form, it is frequently associated with seizures.
b.Diplegia: Both lower extremities predominate the pattern.
c.Quadriplegia: The most severe cases involve children, many of whom are retarded and few of whom will ever walk.
Cerebral palsy is really a syndrome rather than a disease (Fig. 5-25), and no two children are the same, which makes comparison of procedures and other treatments extremely difficult if not impossible. The muscles all tend to be spastic; however, the muscle imbalance is created between spastic and more spastic muscles. Contractures, joint dislocations, limb deformities, and scoliosis should all be anticipated.
5. Children’s Orthopedics |
203 |
Polio
With the introduction of the Salk vaccine in 1954, this disease has become rare in the United States; however, it is certainly not eradicated in the Third World. Because immigrants are seen in our larger cities on an increasingly frequent basis with the sequelae of this disease, some familiarity with it seems appropriate.
The polio virus has unique predilection for the anterior horn cells of the cord and the bulbar portion of the brain. In most cases, the involvement is spotty and the degree of paralysis is variable. The victim is left with a mix of normal muscle, weak muscle, and absent muscle, thus creating a broad spectrum of muscle imbalance but in an asymmetrical distribution. It is important to remember that the sensory fibers are NOT affected, which gives these children a clear and distinct benefit over the children with spina bifida.
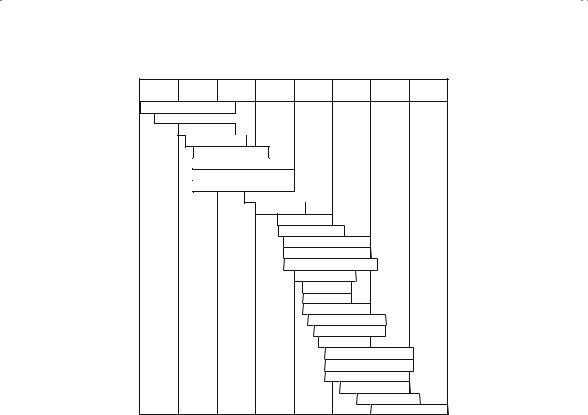
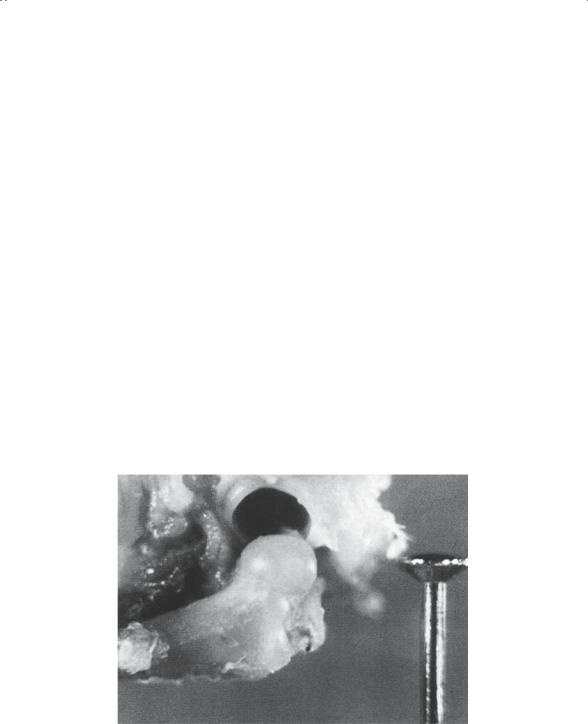
Spina Bifida
Despite the improvement in antenatal testing, many children with myelodysplasia are born in the United States each year. Because of open cord defects at a certain level (Fig. 5-26), these children are essentially congenital paraplegics; they are without motor and sensory modalities below the level of the defect. Needless to say, the higher their level of defect, the poorer their function and, hence, the prognosis (Fig. 5-27). For example, a child with a T12 level (the spinal roots that are the last to function are
FIGURE 5-26. Newborn infant with lumbosacral myelomeningocele. Note the severe equinovarus deformity of both feet. (From Tachdjian MO. Pediatric Orthopedics, 2nd ed, vol 1. Philadelphia: Saunders, 1990. Reprinted by permission.)
204 J.N. Delahay and W.C. Lauerman
L1 |
L2 |
L3 |
L4 |
L5 |
S1 |
S2 |
S3 |
ILIO PSOAS
SARTORIUS
PECTINEUS
GRACILIS
ADD.LONGUS
ADD.BREVIS
ADDUCTOR MAGNUS
QUADRICEPS
OBT.EXT.
TIB.ANT.
TIB.POST.
TEN.FAS.LATA
GLUT.MED.&NIN.
SEMIMEMBRANOSUS
SEMITENDINOSUS
EXT.HALL.L.
EXT.DIG.L.
PER.TERT.
PER.BREVIS
PER.LONGUS
LAT.HIP.ROT.
GASTROCN.
SOLEUS & PLANT
BICEPS FEMORIS
GLUTEUS MAX.
FLEX.HALL.L.& B.
FLEX.DIG.L.& B.
FOOT INTRINSICS
FIGURE 5-27. Neurosegmental innervation of muscles of lower limb. (From Tachdjian MO. Pediatric Orthopedics, 2nd ed, vol 1. Philadelphia: Saunders, 1990. Reprinted by permission.)
T12) has no motor power and no sensation below the waist. These children will be wheelchair confined and have bowel and bladder compromise. On the other hand, children with an S1 level (the last functioning spinal level is S1) have only minimal motor involvement and usually walk without braces. Their major problems are bowel and bladder malfunction.
The absence of sensation below the level of the lesion creates many additional problems for these children. Not unlike a diabetic patient with severe neuropathy, children with spina bifida are prone to foot ulceration, infection, and the development of neuropathic joints.
One recently identified problem in this group is latex allergy. Perhaps as a result of repeated catheterization with latex rubber catheters, these patients can become severely sensitized to all latex contact, to the point of anaphylaxis. Specific protocols are now used at the time of surgical procedures to avoid contact with any latex products, including gloves, catheters, and IV tubing.
Last, it is important to realize that these children, as well as many of those with cerebral palsy, are multiply handicapped. They have learning difficulties, perceptual problems, and hearing and visual impairments, not
5. Children’s Orthopedics |
205 |
to mention emotional issues, all of which require a coordinated effort by multiple specialists to provide optimal care.
Regional Orthopedic Problems
The Pediatric Hip
Most of the showcase pediatric orthopedic maladies affect the hip. Developmental dysplasias, Perthes’ disease, and slipped capital epiphysis have established the hip as the preeminent joint of a child’s musculoskeletal system. Several unique anatomic features predispose this joint to long-term problems following septic, vascular, developmental, and traumatic insults.
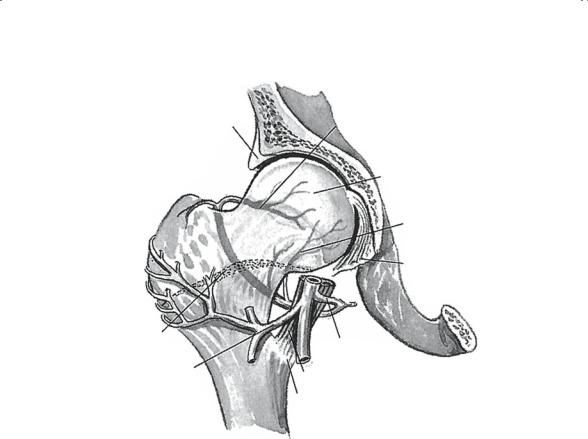
In the newborn, the upper end of the femur (Fig. 5-28) is entirely cartilaginous, representing the secondary ossification centers of both the greater trochanter and the femoral head (capital femoral epiphysis) as a composite chondroepiphysis. The two bony ossification centers develop within this one cartilage mass and grow differentially to their ultimate adult size and shape. Implicit in this fact is that the growth of one is in part dependent on the growth of the other. Normally, the bony centrum of the capital femoral epiphysis is radiographically visible by 3 to 6 months of age.
FIGURE 5-28. Embryology of the hip joint. Note the spherical configuration of the femoral head and acetabulum. The limbus and transverse acetabular ligament are well-formed structures. (From Tachdjian MO. Pediatric Orthopedics, 2nd ed, vol 1. Philadelphia: Saunders, 1990. Reprinted by permission.)
206 J.N. Delahay and W.C. Lauerman
Acetabular labrum |
Posterior superior branch |
|
of medial circumflex |
|
femoral a. |
|
Head of femur |
|
Posterior |
|
inferior |
|
branch |
|
Ligamentum |
|
teres |
Epiphyseal |
|
plate |
Medial circumflex |
Lateral circumflex |
femoral a. |
|
|
femoral a. |
Iliopsoas tendon |
|
Lesser trochanter |
FIGURE 5-29. Posterior view of the normal blood supply of the upper end of the femur in an infant. (From Tachdjian MO. Pediatric Orthopedics, 2nd ed, vol 1. Philadelphia: Saunders, 1990. Reprinted by permission.)
The growth of this epiphysis is dependent primarily on the blood supply of the upper end of the femur (Fig. 5-29). It is essential to recognize that up until 1 year of age there is communication between the metaphyseal and epiphyseal circulations, and this connection protects the capital femoral epiphysis from isolation in the event of an insult to the epiphyseal side. Unfortunately, as the physis thickens and matures by 18 months of age, it becomes an impenetrable barrier between the two circulations, leaving the epiphysis of the head totally dependent on the epiphyseal vessels for its viability. Less than 10% of the femoral head is supplied by the branch of the obturator artery through the ligamentum teres. The epiphyseal vessels are supplied by the medial and lateral circumflex branches of the femoral artery. This vascular isolation of the upper end of the femur is largely responsible for the disastrous complications of developmental dislocation of the hip (DDH), Perthes’ disease, and slipped capital femoral epiphysis (SCFE).
The acetabulum develops from two cartilage segments. The first is the triradiate cartilage, which a bilaminar physis forms at the junction of the
5. Children’s Orthopedics |
207 |
ilium, ischium, and pubis. Integrity of this growth plate is essential for acetabular height to be normal. The depth of the acetabulum is a function of the cartilaginous labrum that circumferentially surrounds the developing acetabulum.
Developmental Dislocation of the Hip
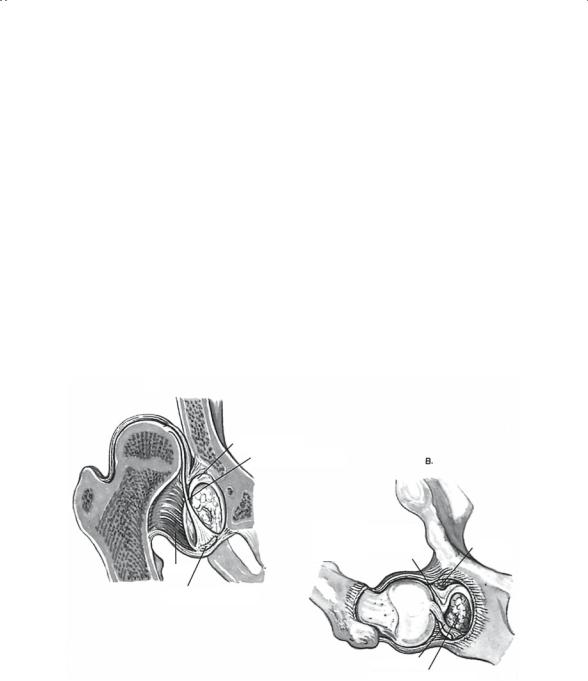
The previous nomenclature, “congenital dislocation,” was recently changed to “developmental dislocation” in recognition of the fact that some of these hips are located at birth and go on to dislocate in the postnatal period. The incidence of this condition is about 1 per 1,000 live births and is more common in females. Although it is fair to say that the etiology is unknown, it is important to recognize that there are both genetic and environmental factors; hence, it is considered a multifactorial trait. It is also critical to recognize that this is a true dysplasia (i.e., aberrant growth), and NOT simply a femoral head that is not located in the acetabulum (Fig. 5-30). It
A
Limbus inverted
Ligamentum teres |
|
|
|
B |
|
elongated |
|
|
|
|
|
|
|
|
Limbus from posterior and superior border of acetabulum interposed between femoral epiphysis and acetabulum preventing reduction of femoral head
Capsule
Transverse acetabular ligament pulled upward
Ligamentum teres
Pulvinar fibrofatty in acetabulum
Capsular adhesions
FIGURE 5-30. Pathology of the dislocated hip that is irreducible owing to intraarticular obstacles. (A) The hip is dislocated. (B) The hip cannot be reduced on flexion, abduction, or lateral rotation. Obstacles to reduction are inverted limbus, ligamentum teres, and fibrofatty pulvinar in the acetabulum. The transverse acetabular ligament is pulled upward with the ligamentum teres. (From Tachdjian MO. Pediatric Orthopedics, 2nd ed, vol 1. Philadelphia: Saunders, 1990. Reprinted by permission.)
208 J.N. Delahay and W.C. Lauerman
is important to stress this fact to the parents in an effort to assist them in understanding the pathology.
Early diagnosis is the key to optimal treatment and the best prognosis. First, consider the risk factors:
1.First-born female
2.Breech presentation
3.Positive family history
4.Hip “click”
5.Presence of a muscular torticollis
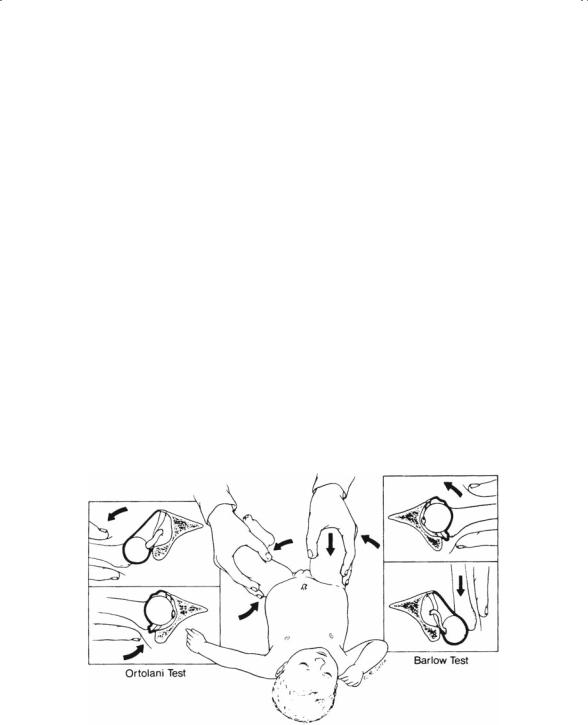
With these in mind, a careful physical examination of the hips is the logical next step. In the newborn, one should attempt to demonstrate laxity and instability (Fig. 5-31). The Barlow test is performed with the infant supine and the hips flexed. As the hips are brought from the abducted to adducted position, a positive test is noted as the femoral head subluxes posteriorly over the posterior rim of the acetabulum; this indicates instability. The Barlow is a provocative test: the hip is located and the maneuver dislocates it. Conversely, the Ortolani test is a reduction maneuver; the hip is dislocated and the test reduces it; this is accomplished by abducting the adducted hip and noting a palpable (but rarely audible) “clunk” as the femoral head reduces over the posterior acetabular rim.
FIGURE 5-31. On the left, the Ortolani (reduction) test is demonstrated. The Barlow (provocation dislocation) test is shown on the right. These tests must be performed on a relaxed infant. (From Sabiston DC Jr. Essentials of Surgery. Philadelphia: Saunders, 1987. Reprinted by permission.)
