
- •1. Topographic Surface Anatomy
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •3. Superficial Face
- •Guide
- •Facts & Hints
- •4. Neck
- •Guide
- •Facts & Hints
- •5. Nasal Region
- •Guide
- •Facts & Hints
- •6. Oral Region
- •Guide
- •Facts & Hints
- •7. Pharynx
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •13. Cerebral Vasculature
- •Guide
- •Facts & Hints
- •14. Topographic Anatomy
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •16. Spinal Cord
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Thorax
- •18. Topographic Anatomy
- •Guides
- •Facts & Hints
- •19. Mammary Gland
- •Guides
- •Facts & Hints
- •20. Body Wall
- •Guides
- •Facts & Hints
- •21. Lungs
- •Guides
- •Facts & Hints
- •22. Heart
- •Guides
- •Facts & Hints
- •23. Mediastinum
- •Guides
- •Facts & Hints
- •Abdomen
- •24. Topographic Anatomy
- •Guide
- •Facts & Hints
- •25. Body Wall
- •Guide
- •Facts & Hints
- •26. Peritoneal Cavity
- •Guide
- •Facts & Hints
- •27. Viscera (Gut)
- •Guide
- •Facts & Hints
- •28. Viscera (Accessory Organs)
- •Guide
- •Facts & Hints
- •29. Visceral Vasculature
- •Guide
- •Facts & Hints
- •30. Innervation
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •32. Topographic Anatomy
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •35. Urinary Bladder
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •39. Testis, Epididymis & Ductus Deferens
- •Guide
- •Facts & Hints
- •40. Rectum
- •Guide
- •Facts & Hints
- •41. Vasculature
- •Guide
- •Facts & Hints
- •42. Innervation
- •Guide
- •Facts & Hints
- •Upper Limb
- •43. Topographic Anatomy
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •48. Neurovasculature
- •Guide
- •Facts & Hints
- •Lower Limb
- •49. Topographic Anatomy
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •51. Knee
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •Guide
- •Facts & Hints
- •54. Neurovasculature
- •Guide
- •Facts & Hints
FACTS & HINTS
Anatomic Points
page 170
page 171
Measurements of the Pelvic Inlet
Used to determine capacityof female pelvis for childbearing
True conjugate diameter
measured radiologicallyon a lateral x-ray
distance from superior border of pubic symphysis to sacral promontory
Transverse diameter: widest distance of pelvic inlet
Oblique diameter: distance from sacroiliac joint to contralateral iliopectineal line
Clinical Points
Fractures of the Pelvis
Alarge force is required to fracture the pelvis and fractures usuallyresult from direct trauma, such as occurs in automobile accidents
The bonypelvis mayfracture at anypoint and there maybe associated damage to pelvic viscera, for example, bladder and urethral rupture can occur with fractures involving the pubis
Pelvic fractures are classified as stable or unstable.
In a stable fracture, the pelvis remains stable and there is onlyone break-point in the pelvic ring with minimal hemorrhage.
 In an unstable fracture, the pelvis is unstable with two or more break-points in the pelvic ring with moderate to severe hemorrhage. Signs of a fractured pelvis include: pain in the groin, hip or lower back; difficultywalking; urethral, vaginal or rectal bleeding; scrotal hematoma; and shock as a result of concealed hemorrhage (contained bleeding into the pelvic cavity)
In an unstable fracture, the pelvis is unstable with two or more break-points in the pelvic ring with moderate to severe hemorrhage. Signs of a fractured pelvis include: pain in the groin, hip or lower back; difficultywalking; urethral, vaginal or rectal bleeding; scrotal hematoma; and shock as a result of concealed hemorrhage (contained bleeding into the pelvic cavity)
Afracture can be confirmed on x-rayand is seen as a break in continuityof the pelvic ring.
Decubitus Ulcers
Also called pressure sores
Can be a partialor full-thickness loss of skin, underlying connective tissue and can extend into muscle, bone, tendons, and joint capsules. Two thirds of pressure sores occur in patients older than 70 years
Results from prolonged pressure on an area of skin, connective tissue and muscle from a mattress, wheelchair seat, or bed rail. Commonlyoccur in those with poor mobility, bed-bound, poor nutrition, and incontinence.
Can become infected with bacteria from poor skin care, or fecal or urinaryincontinence
The hip and buttock regions account for 67% of all pressure sores, with ischial tuberosity, trochanteric, and sacral locations being most common.
In the sitting position, the ischial tuberositybears the weight of the whole bodyand thus is a prime site of ulceration
263 / 425

34 Pelvic Floor and Contents
STUDYAIMS
At the end of your study, you should be able to:
State the structures that form the pelvic floor
Describe the two main muscles that form the pelvic floor and their attachments List the functions of the pelvic floor muscles
Describe the attachments of the peritoneum within the pelvis and the location of the vesicoand recto-uterine pouches in females and rectovesical pouch in males
Understand the organization and function of the pelvic fascia
Describe the clinical problems that mayarise with weaknesses of the pelvic floor muscles
264 / 425
GUIDE
Pelvis and Perineum: Pelvic Floor and Contents
[Plate 338, Pelvic Diaphragm: Female (continued)]
265 / 425
[Plate 339, Pelvic Diaphragm: Female (Continued)]
266 / 425
[Plate 341, Pelvic Diaphragm: Male (Continued)]
267 / 425
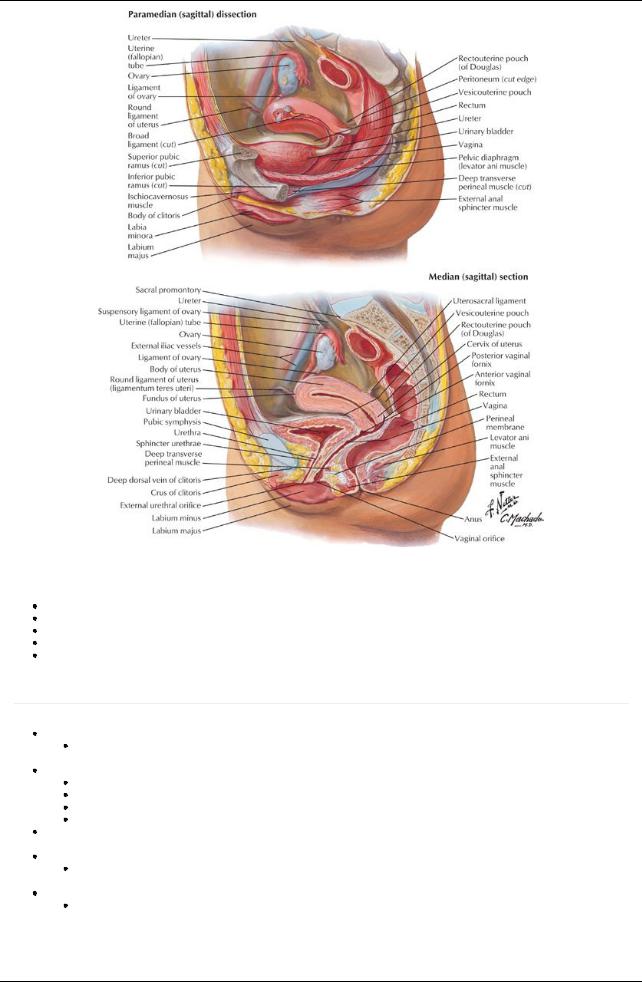
[Plate 342, Pelvic Viscera and Perineum: Female]
Pelvic Floor
Formed bythe pelvic diaphragm
Funnel-shaped
Muscular partition from the pubis to the coccyxand from lateral wall to lateral wall
Separates pelvic cavityfrom perineum inferiorly
Transmits urethra, vagina (in females) and anal canal
Muscles of Pelvic Floor
page 172 page 173
The pelvic diaphragm is composed of two paired muscles
Levator ani
 Coccygeus Levator ani muscle
Coccygeus Levator ani muscle
Paired muscle
Principal muscle of pelvic floor
Supports pelvic contents
Activelymaintains position of pelvic viscera
Arcus tendineus: a thickened line of the fascia over the obturator internus muscles running in an arching line from the pubis to the ischial spine
Central perineal tendon or perineal body
Afibromuscular bodyextending from the perineum into the urogenital hiatus
 The site of numerous muscle attachments in the perineum Components of the levator ani muscle
The site of numerous muscle attachments in the perineum Components of the levator ani muscle
Pubococcygeus
Is anterior part of levator ani Main contributor to the levator ani
Arises from the posterior bodyof the pubic bone and anterior part of the arcus Tendineus
Runs posteriorlyto attach to the anococcygeal ligament and the coccyx
268 / 425
Iliococcygeus
Posterior part of the levator ani Is thin and poorlydeveloped
Arises from the posterior part of the arcus tendineus and the ischial spine Attaches to the anococcygeal raphe and the coccyx
Puborectalis
Athickened band of muscle best seen inferior to the pubococcygeus
Unites with its partner to make a U-shaped sling around the rectum at its junction with the anus
Has a sphincter-like action bypulling the anorectal junction forward and contributing to anal continence Medial muscle fibers of the pubococcygeus border the urogenital hiatus
Most anterior fibers insert into the urethra
Other fibers sweep behind the vagina or prostate and insert into the central perineal tendon, and are called the levator prostatae or pubovaginalis
Coccygeus muscle
Reinforces pelvic floor posteriorly
Arises from ischial spine
Inserts on lower two sacral and upper two coccygeal segments
 Blends with sacrospinous ligament on its external surface Innervation of the levator ani and coccygeus muscles
Blends with sacrospinous ligament on its external surface Innervation of the levator ani and coccygeus muscles
Levator ani innervated bybranches from the anterior rami of S3-S4 spinal nerves
Puborectalis also innervated bybranch of pudendal nerve (S2,3,4)
 Coccygeus supplied bybranches of the anterior rami of S4-S5 spinal nerves Functions of the levator ani
Coccygeus supplied bybranches of the anterior rami of S4-S5 spinal nerves Functions of the levator ani
Acting together raise the pelvic floor to increase abdominal pressure, such as when coughing, sneezing, urinating, defecating, lifting heavyobjects.
Important in voluntarycontrol of micturition (urinating)
Supports pelvic viscera Supports head of the fetus
Muscles Lining the Lateral Walls of the Pelvis
Obturator internus muscle
Proximal attachment: pelvic surfaces of ischium and ilium and obturator membrane
Distal attachment: greater trochanter of femur
Innervated bynerve to obturator internus (L5, S1-S2)
Lateral rotator of thigh
Piriformis muscle
Proximal attachment: pelvic surfaces of S2-4 segments of sacrum, sacrotuberous ligament
Distal attachment: greater trochanter of femur
Innervated byventral rami of S1-S2 spinal nerves
Lateral rotator of this
Muscle |
Proximal Attachment (Origin) |
Distal Attachment (Insertion) |
Innervation |
Main Actions |
Obturator internus |
Pelvic aspect of obturator |
Greater trochanter of femur |
Nerve of |
Rotates external thigh |
|
membrane and pelvic bones |
|
obturator |
laterally; abducts flexed |
|
|
|
internus |
thigh at hip |
Piriformis |
Anterior surface of second to |
Greater trochanter of femur |
Ventral rami |
Rotates external thigh |
|
fourth sacral segments and |
|
of S1-S2 |
laterally; abducts flexed |
|
sacrotuberous ligament |
|
|
thigh; stabilizes hip joint |
Levator ani |
Bodyof pubis, tendinous arch |
Perineal body, coccyx, anococcygeal |
Ventral rami |
Supports pelvic viscera; |
|
of obturator fascia, and ischial |
raphe, walls of prostate or vagina, |
of S3-S4, |
raises pelvic floor |
|
spine |
rectum, and anal canal |
perineal |
|
|
|
|
nerve |
|
Coccygeus |
Ischial spine and |
Inferior sacrum and coccyx |
Ventral rami |
Supports pelvic viscera; |
(ischiococcygeus) |
sacrospinous ligament |
|
S4-S5 |
draws coccyxforward |
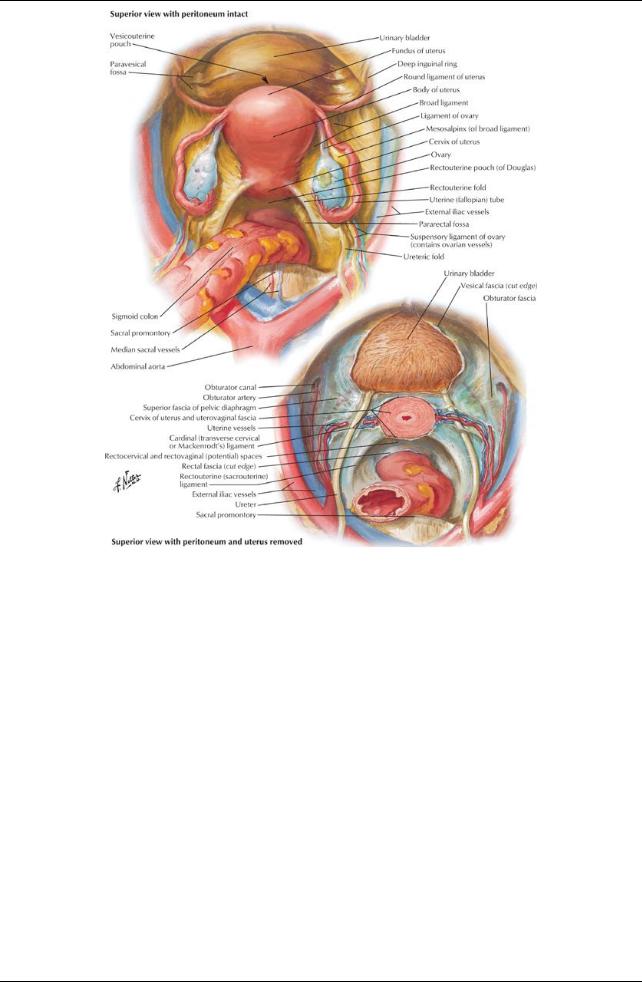
Pelvic Fascia
Occupies space between peritoneum and muscles of the pelvic floor and walls
Parietal pelvic fascia lines the internal surface (facing the pelvic cavity) of the muscles of the floor and walls Visceral pelvic fascia invests each of the pelvic organs
Visceral and parietal fascia are continuous where organs penetrate pelvic floor
Where theyare continuous, fascia thickens to form the tendineus arch of pelvic fascia (arcus tendinous fasciae pelvis)
 Arches are bilateral bands running from pubis to sacrum, adjacent to viscera Puboprostatic ligament
Arches are bilateral bands running from pubis to sacrum, adjacent to viscera Puboprostatic ligament
Pubovesical ligament Sacrogenital ligaments
Between parietal and visceral fascia is endopelvic fascia
Matrixor filler material
 In certain areas, condenses and becomes more fibrous to form fascial "ligaments" or septa Major condensation is the hypogastric sheath
In certain areas, condenses and becomes more fibrous to form fascial "ligaments" or septa Major condensation is the hypogastric sheath
Runs from lateral pelvic wall to pelvic viscera
Separates retropubic space from presacral space
Serves as a conduit for vessels and nerves
Transverse cervical (cardinal) ligaments are part of hypogastric sheath
Runs from lateral wall to the uterine cervixand vagina
Uppermost part is beneath broad ligament and transmits the uterine artery Is sufficientlyfibrous to provide passive support for the uterus
269 / 425
Uterosacral (female) or genitosacral (male) ligaments Septa separate the pelvic organs and include
Vesicovaginal septum
Rectovesical septum
Rectovaginal septum
Weakness of the pelvic floor muscles or in the pelvic fascia, which support the pelvic organs, can result in prolapse of the pelvic organs, e.g., vaginal or rectal prolapse.
Pelvic Contents
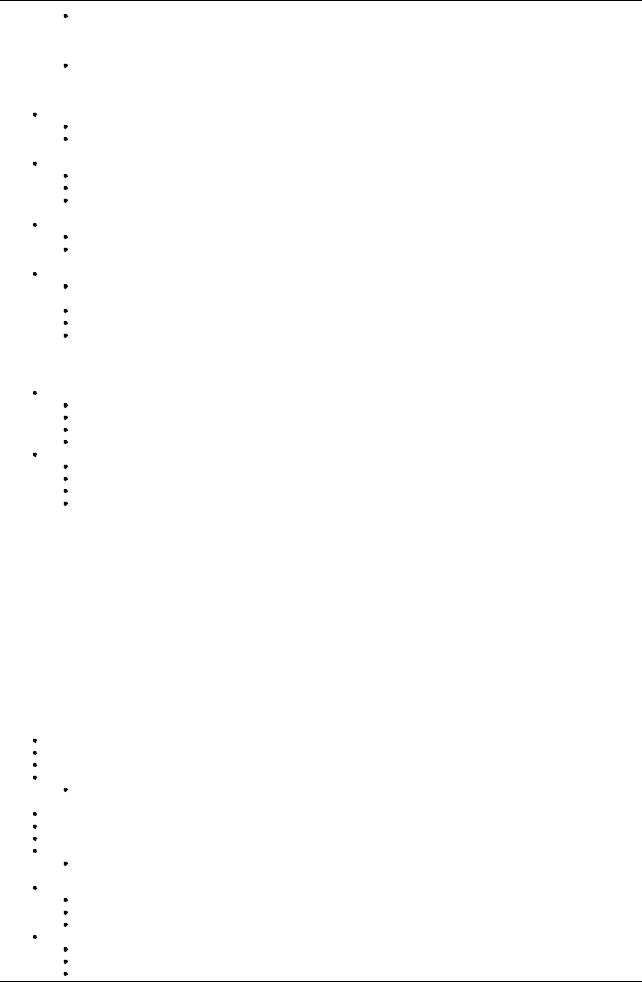
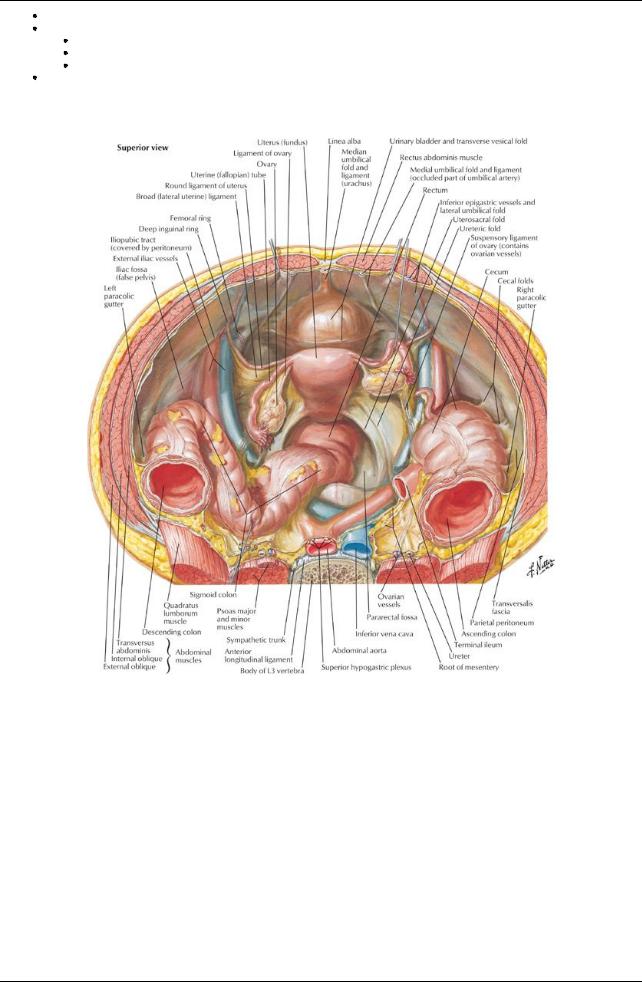
[Plate 343, Pelvic Contents: Female]
270 / 425
[Plate 344, Pelvic Viscera: Female]
271 / 425
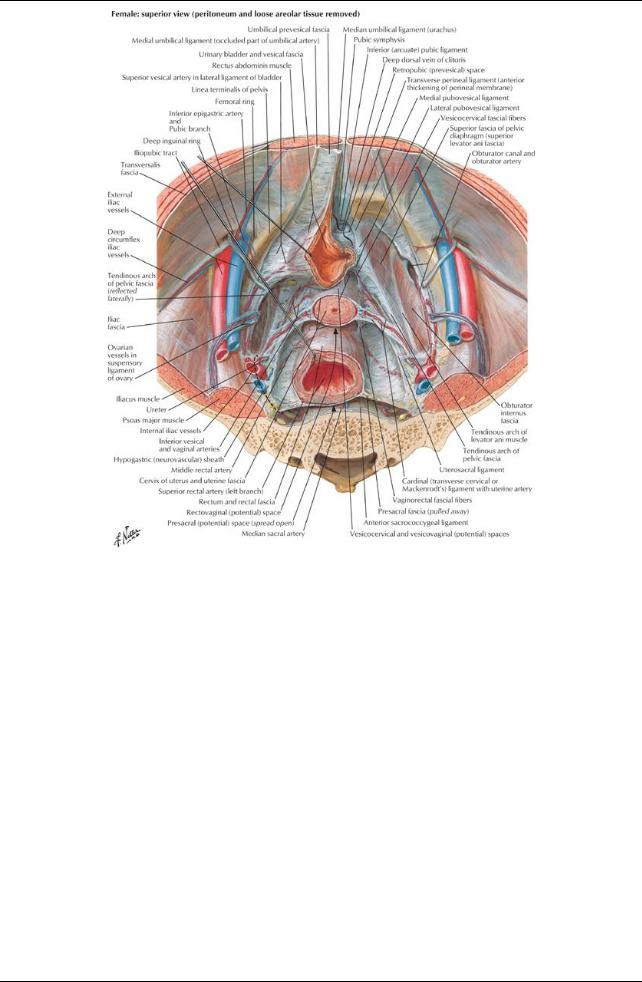
[Plate 345, Endopelvic Fascia and Potential Spaces]
272 / 425
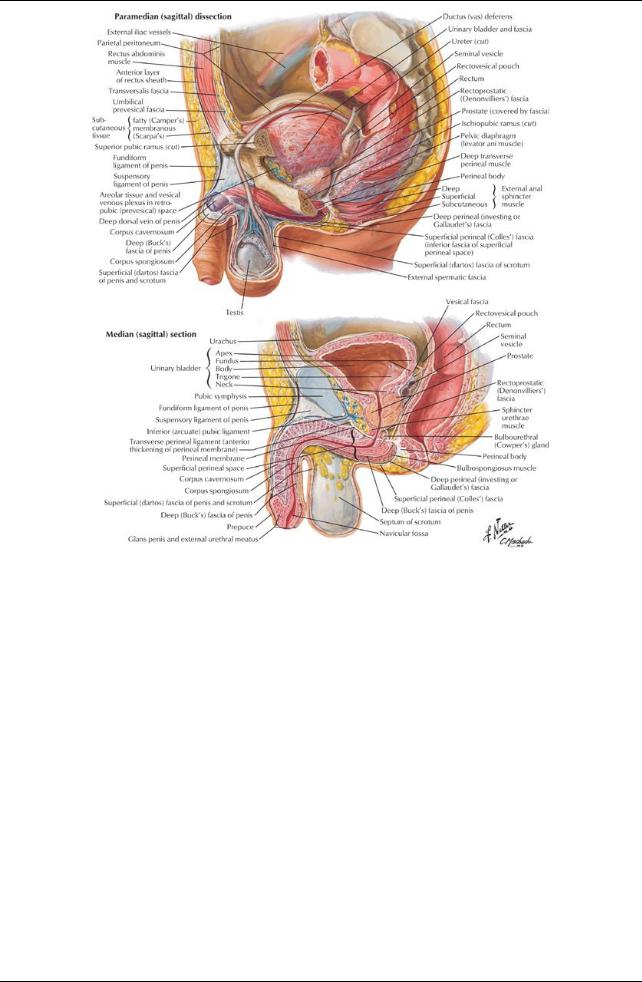
[Plate 346, Pelvic Viscera and Perineum: Male]
273 / 425
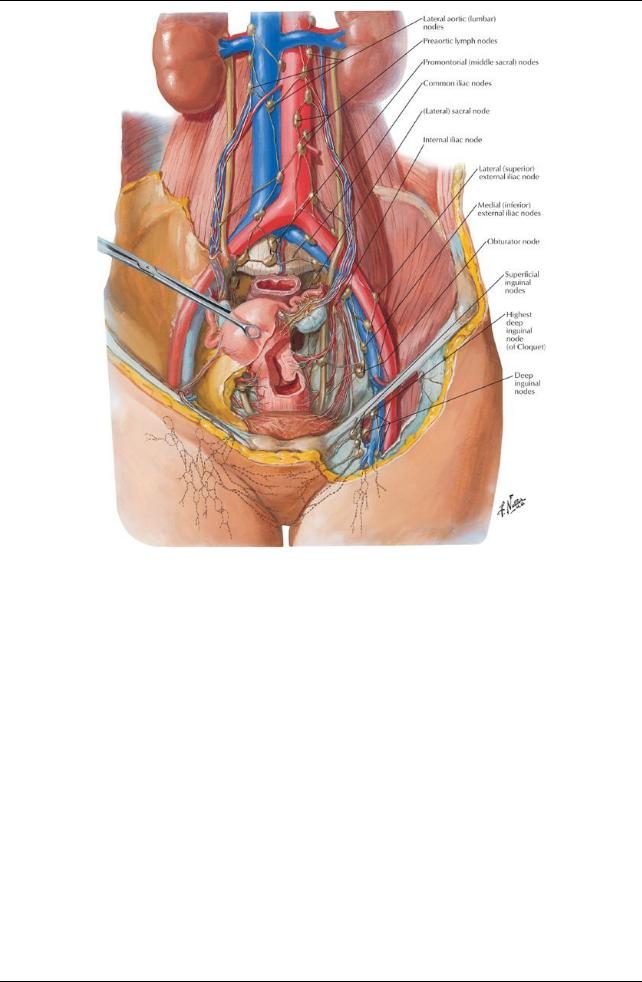
[Plate 386, Lymph Vessels and Nodes of Pelvis and Genitalia: Female]
274 / 425
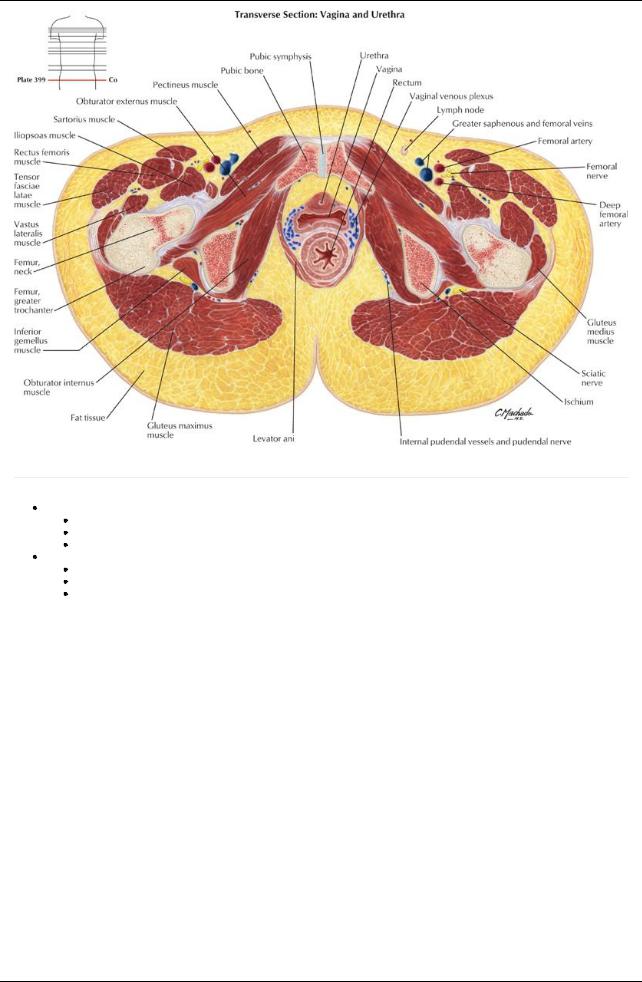
[Plate 399, Female Pelvis: Vagina-Urethra]
page 174
page 175
Female Pelvic Viscera and Perineum See:
Section 5-4: Urinary Bladder
Section 5-5: Uterus, Vagina and Supporting Structures
Section 5-9: Rectum
Male Pelvic Viscera and Perineum See:
Section 5-4: Urinary Bladder
Section 5-8: Testis, Epididymis, and Ductus Deferens
Section 5-9: Rectum
275 / 425
