
- •Preface
- •Acknowledgments
- •Basic Physics
- •Transducers and Resolution
- •Doppler Physics
- •Artifacts
- •Summary
- •Introduction
- •Patient Preparation
- •Patient Positioning
- •Transducer Selection
- •Two-Dimensional Images
- •Two-Dimensional Imaging Controls
- •Introduction
- •M-Mode Echocardiography
- •Color-Flow Doppler
- •Spectral Doppler
- •Tissue Doppler Imaging
- •Measurement and Assessment of Two-Dimensional Images
- •Measurement and Assessment of M-Mode Images
- •Measurement and Assessment of Spectral Doppler Flow
- •Measurement and Assessment of Tissue Doppler Imaging
- •Evaluation of Color-Flow Doppler
- •Evaluation of Ventricular Function
- •Mitral Regurgitation
- •Aortic Regurgitation
- •Tricuspid Regurgitation
- •Pulmonary Regurgitation
- •Endocarditis
- •Pulmonary Hypertension
- •Systemic Hypertension
- •Hypertrophic Cardiomyopathy
- •Dynamic Right Ventricular Outflow Obstruction
- •Moderator Bands
- •Dilated Cardiomyopathy
- •Right Ventricular Cardiomyopathy
- •Restrictive Cardiomyopathy
- •Endocardial Fibroelastosis
- •Arrhythmogenic Right Ventricular Cardiomyopathy
- •Myocardial Infarction
- •Myocardial Contusions
- •Pericardial Effusion
- •Neoplasia as a Cause of Pericardial Effusion
- •Pericardial Disease
- •Abscesses
- •Pericardial Cysts
- •Thrombus
- •Ventricular Septal Defect
- •Patent Ductus Arteriosus
- •Aorticopulmonary Window
- •Right to Left Shunting PDA
- •Atrial Septal Defects
- •Endocardial Cushion Defects
- •Bubble Studies
- •Atrioventricular Valve Dysplasia
- •Outflow Obstructions
- •Inflow Obstructions
- •Tetralogy of Fallot
- •APPENDIX ONE Bovine
- •APPENDIX TWO Canine
- •APPENDIX THREE Equine
- •APPENDIX FOUR Feline
- •APPENDIX FIVE Miscellaneous Species
- •Index

Table 5.3
Mitral Regurgitation: Parameters for the Assessment of Severity in Man
Adapted from: Zoghbi W, Enriquez-Sarano M, Foster E, et al. American Society of Echocardiography. Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography. J Am Soc Echocardiogr 2003;16:777–802.
Aortic Regurgitation
Aortic insufficiency may result from degeneration, vegetative lesions, torn or flail cusps, or congenital malformation of the leaflets (112). Echocardiographically it may not be possible to differentiate between these causes of insufficiency. Aortic insufficiency shows the following on an echocardiogram: left ventricular volume overload, valvular lesions, diastolic flutter of the mitral and aortic valves, and an increased E point to septal separation (EPSS). Large increases in ventricular dimension may also result in dilation of the aortic root (113–115).
Two-Dimensional and M-Mode Evaluation
Valve Appearance and Motion
Valvular lesions are not always visible on the echocardiogram, and the absence of lesions does not mean the absence of disease (116,177). The resolving capabilities of low frequency transducers is often not sensitive enough to show nodules and irregularities smaller than 2 mm on aortic valves (118,119). Even in small animals with high resolution transducers, resolving small lesions is sometimes difficult.
Degenerative lesions of the aortic valve are typically smooth, small, and rounded (Figures 5.53, 5.54). Large irregular hyperechoic masses associated with the leaflets are more suggestive of vegetative endocarditis (Figures 5.55, 5.56) (116,120,121). Large vegetations are often floppy and prolapse into the outflow tract (122,123). Prolapsed aortic valve cusps with or without lesions bow into the outflow tract and are easily visible on real-time images (Figure 5.57). This is seen more frequently in horses as a cause of aortic insufficiency (Figure 5.58). M-mode images sometimes show multiple linear echoes representing the lesions during diastole or systole on aortic root images instead of the normal fine single line associated with the closed and open aortic valve (Figure 5.59) (114,122–

125).
2D and M-Mode Features of AR
Valvular lesions
LV volume overload if insufficiency significant
Diastolic MV flutter
Increased EPSS
AR secondary to rapid vegetative growth will not show LV volume overload.
Figure 5.53 This dog has both mitral valve and aortic valve lesions (arrows). Whether these are degenerative or vegetative cannot be determined echocardiographically. RV = right ventricle, LV = left ventricle, LA = left atrium, AO = aorta, View = right parasternal left ventricular outflow view.
Figure 5.54 (A) Small nodules are seen on the aortic valve of this horse. View = right parasternal long axis inflow outflow. (B) At least two aortic valve cusps are thickened in this horse (arrow). RV = right ventricle, AO = aorta, LA = left atrium, LV = left ventricle. View = right parasternal transverse heart base.

Figure 5.55 There is a large vegetative lesion on the aortic valve of this dog (arrow). RV = right ventricle, LA = left atrium, AO = aorta, LAU = left auricle, View = right parasternal transverse heart base.

Figure 5.56 A large growth is seen on this dog’s aortic valve. Lesions of this size have a greater chance of embolization and may create both insufficiency and obstruction. LV = left ventricle, AO = aorta, LA = left atrium, View = right parasternal long axis left ventricular outflow view.
Figure 5.57 A zoomed image of the aortic valve growth in this dog shows the lesion prolapsing into the outflow tract (arrow). LV = left ventricle, AO = aorta, LA = left atrium, MV = mitral valve, View = right parasternal left ventricular outflow.

Figure 5.58 The aortic valve in this horse has no obvious lesions but does prolapse into the outflow tract and is the cause of aortic insufficiency in this animal (arrow). RV = right ventricle, LV = left ventricle, AO = aorta, View = right parasternal left ventricular outflow view.
Figure 5.59 M-mode images of aortic valve lesions typically show multiple lines representing the thickened cusps during (A) diastole (arrow) and (B) systole (arrow). RV = right ventricle, AO = aorta, LA = left atrium.

Diastolic fluttering of the mitral valve is probably the most common M-mode finding in man and animals with aortic insufficiency. This is seen even if the volume of regurgitation is not severe. The diastolic fluttering occurs secondary to turbulence associated with the regurgitant jet as it flows into the outflow tract. M-mode images may show dramatic mitral valve fluttering, a sawtooth appearance, during diastole when the mitral leaflet is wide open, and this is especially easy to appreciate with slow heart rates (Figures 4.100, 5.60, 5.61) (114,115,120,122,126–129). This fine vibration may encompass the entire diastolic time period or any portion of it. The regurgitant jet does not have to directly strike the leaflet to create this fluttering; jets that are directed away from the mitral valve create the vibration simply because of turbulence within the left ventricular outflow tract. Regurgitant jets directed toward the ventricular septum may cause early diastolic vibration of the septum (114,115,119,122, 126–128,130).
Diastolic MV flutter may be seen even with mild AR.

Figure 5.60 Fine vibrations on the mitral valve during diastole are a sign of aortic insufficiency (arrow) in this horse. RV = right ventricle, LV = left ventricle.
Figure 5.61 Diastolic flutter of the mitral valve (arrows) is a sign of aortic insufficiency in this dog with bacterial endocarditis. This is a zoomed-in image.
The mitral valve may also show reverse doming of the septal leaflet back toward the left atrial chamber during diastole as the force of the aortic regurgitant jet flows into the left ventricular outflow tract. On transverse views this appears as indentation of the septal leaflet toward the free wall of the left ventricular chamber (128,131–133).
The mitral valve E point to septal separation (EPSS) in animals with significant aortic insufficiency is increased as the regurgitant jet restricts motion of the mitral valve (Figure 4.99). A large EPSS in this case does not correlate with decreased ejection fraction but neither does it necessarily correlate with severity of the valvular insufficiency (134). Mitral valve motion may be dramatically altered and

reduced with significant aortic insufficiency.
The mitral valve may also close earlier than usual, before the beginning of the QRS complex. This occurs secondary to elevated left ventricular diastolic filling pressures, and with acute severe aortic regurgitation, left ventricular diastolic pressure increases rapidly and can become higher than left atrial pressure toward the end of diastole resulting in premature mitral valve closure (132). This is usually seen in animals already in congestive heart failure (114,122,135,136).
MV closure before the start of the QRS complex = high left ventricular pressure.
Diastolic flutter of the aortic valve is also reported with aortic insufficiency. This is most commonly seen in horses with aortic valve insufficiency (113,129,137). The vibration occurs secondary to flow through the cusps when they should be closed during diastole. Aortic valve diastolic flutter has been reported with fenestration of the aortic cusps, torn cusps, and endocarditis involving the aorta in horses (122,138,139).
Left Ventricular Size and Function
Volume overload occurs with chronic moderate to severe aortic insufficiency. Aortic insufficiency (AI) often has a greater negative impact upon myocardial function than mitral regurgitation (MR). Afterload and wall stress are higher in animals with AI versus MR since there is no flow into a low pressure left atrium early during systole (112). All of the volume within the left ventricle must be must be dealt with when only the aortic valve is insufficient. Volume overload should lead to compensatory eccentric hypertrophy, and function should elevate secondary to stretch of the myocardial fibers (52,113,122,129). Failure to see an elevation in fractional shortening and a normal systolic dimension suggests the presence of myocardial failure (52,117,120,140). Acute aortic regurgitation often results in significant symptoms since there is no time for compensatory mechanisms to manifest themselves (112). Studies that create aortic regurgitation show an acute increase in volume and wall stress with a return to normal wall stress after compensatory hypertrophy has occurred. This takes approximately 1 month (141).
The severity of aortic insufficiency is best evaluated with Doppler ultrasound, but its effect on the left ventricle must be assessed as well. Hemodynamically insignificant insufficiencies will not cause the ventricle to dilate. Chronically, mild to moderate leaks cause an increase in left ventricular diastolic dimension, compensatory hypertrophy, and elevated fractional shortening. The heart affected by acute severe insufficiency will not have developed these compensatory changes.
LV Function in AR (man)
Ejection fraction <50% = poor prognosis
Assessment of left ventricular function is an important parameter in patients with aortic insufficiency. Ejection fractions calculated from apical images provide some assessment of prognosis in man. An ejection fraction of less than 50 to 55% endures a poor prognosis in people with aortic regurgitation regardless of whether they are symptomatic (112,142). This has not been evaluated in animals.

Color-Flow Doppler Evaluation
Color-flow Doppler utilizes three methods to assess the severity of aortic insufficiency. These are the proximal flow convergence in the aorta, vena contracta, and jet direction and size into the left ventricular outflow tract and chamber.
Color assessment of AR uses:
Flow convergence
Vena contracta
Jet height
Jet Size
Historically the Doppler assessment of the severity of aortic insufficiency in man is based upon the extent of the regurgitant jet into the left ventricular outflow tract and chamber. A regurgitant jet that extends just beyond the aortic valve and dissipates into a nonaliased signal quickly is considered to be mild, a jet that extends to the tips of the mitral valves is moderate in severity, and a jet that extends beyond the mitral leaflets into the left ventricular chamber is severe (Figures 5.62, 5.63, 5.64, 5.65, 5.66). The correlation here with actual severity is less than for mitral insufficiency because this flow is influenced by the volume and compliance of the left ventricular chamber, the size of the orifice, the pressure gradient, and the duration of the gradient between the aorta and left ventricle (73,74,131,143).
Figure 5.62 This small jet of aortic insufficiency represents mild insufficiency (arrow). It has a small point of origin and quickly dissipates to a nonaliased signal. RV = right ventricle, RA = right atrium, LV = left ventricle, AO = aorta, View = right parasternal left ventricular outflow image.
Figure 5.63 An aortic regurgitant jet that encompasses about half the width of the outflow tract and extends past the tips of the mitral valve leaflets is considered to be severe (arrow). RV = right ventricle, LV = left ventricle, AO = aorta, LA = left atrium, View = right parasternal left ventricular

outflow image, Species = equine.
Figure 5.64 Severe aortic regurgitation fills the outflow tract and extends to the apex of the left ventricular chamber on this apical view of the heart. LV = left ventricle, RV = right ventricle, AO = aorta, LA = left atrium.
Figure 5.65 This severe aortic regurgitant jet fills up the outflow tract and extends significantly beyond the mitral valve leaflets. RV = right ventricle, AO = aorta, LV = left ventricle.

Figure 5.66 Aortic regurgitation is significant when the color flow signal fills the width of the outflow tract and extends beyond the tips of the mitral leaflets. RV = right ventricle, VS = ventricular septum, LVW = left ventricular wall, LA = left atrium, AO = aorta.
Analyzing jet height is preferred over jet length when assessing the significance of aortic regurgitation with color-flow Doppler (1). This method appears to have a much better correlation with actual significance of the regurgitation than jet length (131,144). Jet height measured just proximal to the aortic valve (within 1 cm) compared to the diameter of the left ventricular outflow tract has a correlation of (r = .91) with quantitative methods of assessment. This measurement is obtained from long-axis parasternal images whenever possible to maximize axial resolution of the color jet (Figure 5.67). Jet height to outflow tract width ratio of ≥65% correlates highly with severe insufficiency, a jet height to outflow tract ratio of <24% represents mild insufficiency, moderate insufficiency has a jet height to outflow tract ratio of between 25 and 46%, and those between 47 and 64% are moderate to severe (143,144). Of all the methods for assessing aortic regurgitation severity, this method shows the best correlation with angiographically measured severity (145). When jet height is recorded from

transverse imaging planes, the radius can be used to calculate jet area. A proximal jet area to left ventricular outflow tract area ratio is obtained (Figure 5.68). A ratio of ±60% is consistent with the diagnosis of severe aortic regurgitation (144). These two methods of analysis become inaccurate when jets are eccentric. Aortic insufficiency that diffusely leaks along an entire cusp line is also difficult to assess with these methods (Figure 5.69). Jet area is usually subjectively assessed as opposed to direct measurement of jet height and area (1,144).
Regurgitant Jet Height to Outflow Tract Width
Measure just proximal to valve ( 1 cm).
Use parasternal long-axis images.
It is inaccurate if eccentric jet.
Use zoom.
Severity
Ratio >65% = severe AR
Ratio 25–46% = moderate AR
Ratio 47–64% = moderate to severe AR
Ratio <24% = mild AR
Figure 5.67 Jet height of this aortic regurgitation is between 25 and 46% of the left ventricular outflow tract diameter, making it moderate in severity. RA = right atrium, VS = ventricular septum, LV = left ventricle, LVW = left ventricular wall, LA = left atrium, Plane = right parasternal left ventricular outflow view.
Figure 5.68 Comparing aortic regurgitation jet area to left ventricular outflow tract area is used to determine severity of the leak. Here jet area is .2 cm2 and outflow area is 3.9 cm2. The ratio of 2.5 is consistent with mild regurgitation.

Figure 5.69 Jet area to outflow area ratio cannot be applied to diffuse aortic regurgitation that leaks along cusp lines. RV = right ventricle, RA = right atrium, AO = aorta, LA = left atrium.
Vena Contracta
Vena contracta is also applied to aortic regurgitant jets. The vena contracta is the smallest width of the regurgitant jet as it flows through the aortic valve. As with jet height, this measurement should be obtained from long-axis parasternal outflow views in order to maximize axial resolution, and all components of the insufficiency should be seen, proximal flow convergence, vena contracta, and jet expansion into the outflow tract (Figure 5.70) (1). This measurement will always be smaller than jet height since the regurgitant jet will expand after it enters the outflow tract. A vena contracta size of >.5 cm is highly sensitive for severe aortic regurgitation, a vena contracta width of ≥7 mm is highly specific for severe regurgitation while a vena contracta of <3 mm is highly specific for mild regurgitation in man as long as the regurgitant jet is centrally directed and not eccentric (112,146). A 6-mm size has the best combination of specificity and sensitivity for significant aortic regurgitation (1,147).

Vena Contracta
Measure smallest width through valve.
Use parasternal long-axis images.
See flow convergence, and vena contracta and jet expansion.
Use zoom.
Severity
<3 mm = mild AR >6 mm = severe AR
Figure 5.70 The vena contracta of an aortic regurgitant jet is measured at the valve from the narrowest color flow signal. RA = right atrium, LV = left ventricle, LVW = left ventricular wall, AO = aorta, LA = left atrium.
Regurgitant orifice size can be calculated. Orifice size corresponds to the area of the vena contracta. An experimental study in dogs with created aortic regurgitation found a good correlation between area of the vena contracta and EROA (r = .91) (148). An orifice size >.3 cm2 and a regurgitant volume of >60 ml/beat in man imply severe aortic regurgitation (112,146). Effective regurgitant orifice area can be calculated from vena contracta using Equation 5.16.
Equation 5.16 
Effective regurgitant orifice area is influenced by systemic pressure as well as size of the aorta. Distended ascending aortas and systemic hypertension prevent proper coaptation of the aortic valve cusps leading to insufficiency. Decreasing pressure will reduce orifice size and decrease the amount of regurgitation (149).
Vena contracta and EROA (dogs)
>.3 cm2 = severe
The vena contracta is not always symmetrical, and its width in one imaging plane may not be the same in another imaging plane. This is also a very small diameter and a miscalculation because of poor image quality, not zooming in, and so on, can compound the error and assign a severity that does

not reflect an accurate assessment of regurgitation (150).
Proximal Isovelocity Surface Area
Proximal flow convergence is used to assess aortic regurgitation in man. Adjust the Nyquist limit until a hemisphere of flow convergence with an aliasing border is seen (Figures 5.71, 5.72). This should be obtained early in diastole when velocity of regurgitant flow is maximal. Calculating the flow velocity integral of the regurgitant jet allows the calculation of EROA and regurgitant volume just as it does in mitral regurgitation (Equations 5.17–5.19, 5.22).
Equation 5.17 
Equation 5.18 
Equation 5.19 
Figure 5.71 Proximal flow convergence (arrow) is used to assess aortic regurgitation. LV = left ventricle, AO = aorta, LA = left atrium, RV = right ventricle, AR Rad = radius of PISA, AR Als Vel = Nyquist limit at the aliasing velocity, AR Flow = regurgitant flow volume.
Figure 5.72 Zooming in on the flow convergence makes measurements more accurate. LV = left ventricle, AO = aorta, LA = left atrium, RV = right ventricle, AR Rad = radius of PISA, AR Als Vel = Nyquist limit at the aliasing velocity, AR Flow = regurgitant flow volume.

Calculation of EROA and RV using PISA in aortic regurgitation has the same intrinsic errors that PISA calculations have for mitral regurgitation. The lack of or a minimal flow convergence area is consistent with mild regurgitation while a large flow convergence area reflects severe aortic regurgitation (112,151). Severe aortic regurgitation is present with an EROA of ≥.3 cm2 and a regurgitant volume of ≥60 ml in man (1).
PISA and EROA
See all components of AR jet.
Flow convergence
Vena contracta
Jet expansion
Measure early in diastole when flow maximal.
This is not accurate with eccentric jets.
Use apical view.
Use zoom.
Adjust Nyquist limit for best hemisphere.
Spectral Doppler
Pressure Half-Time and Slope
Using slopes and pressure half-times, spectral Doppler provides additional hemodynamic information concerning the severity and hemodynamic significance of aortic regurgitation. The slope and halftime (see Chapter 4) of an aortic insufficiency jet is dependent upon how fast the aortic and ventricular pressures equilibrate during diastole. A large regurgitant orifice allows the pressure to equilibrate rapidly (aortic pressure drops quickly and left ventricular pressure rises rapidly during diastole as volume leaves the aorta and enters the left ventricle) resulting in a steep slope and short pressure half-time (Figures 4.91, 5.73). A small regurgitant orifice delays the equilibration, and a plateau-shaped profile is seen with a long pressure half-time (Figures 4.92, 5.74). In other words, the pressure gradient at the end of diastole is relatively unchanged from the pressure gradient at the beginning of diastole. In man, a pressure half-time of greater than 500 msec is indicative of

hemodynamically insignificant aortic regurgitation whereas a pressure half-time of less than 300 msec (some use 200 msec) implies mild aortic insufficiency (1,112). This method shows much overlap between levels of severity, but it is good at differentiating between mild regurgitation and severe regurgitation by using a pressure half-time of 400 msec (specificity .92) (152).
Significant AR allows LV and AO diastolic pressures to equalize rapidly resulting in short pressure half-times.
AR Pressure Half-Time (man) <300 msec = severe AR >500 msec = mild MR Much overlap in midrange
AR Slope (man)
<2 m/sec2 = mild AR >3 m/sec2 = severe AR
Figure 5.73 A large aortic regurgitant orifice allows aortic and left ventricular pressures to equilibrate rapidly resulting in a rapid decline in velocity and a short pressure half-time (PHT = 338 msec). MVA = mitral valve area.
Figure 5.74 A small aortic regurgitant orifice prevents equilibration of pressures between the aorta and left ventricle, and the flow profile is plateau shaped with a long pressure half-time (PHT = 777 msec). MVA = mitral valve area.
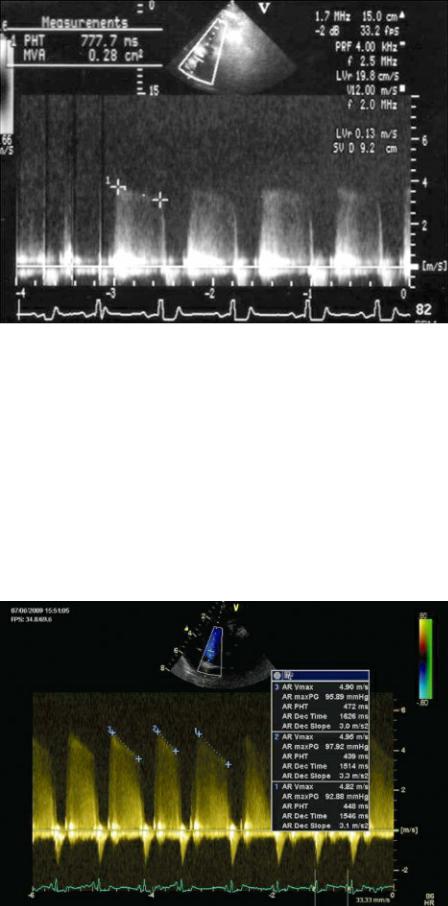
Calculating slope instead of pressure half-time of course has the same degree of ambiguity and there is considerable overlap. However, a deceleration slope of >2 m/sec2 differentiates mild regurgitation from moderate and severe regurgitation, and a slope of >3 m/sec2 differentiates between mild to moderate and severe aortic insufficiency in man (Figure 5.75) (153,154).
Figure 5.75 Slope of the aortic regurgitant spectral display differentiates between mild, moderate, and severe regurgitation. The slope here is at 3 m/sec2 consistent with severe aortic regurgitation. AR = aortic regurgitation, AR Vmax = maximum velocity of AR, AR max PG = maximum pressure gradient of AR, AR PHT = pressure half-time of AR, AR Dec Time = deceleration time of AR, AR Dec Slope = deceleration slope of AR.
These two parameters, slope and half-time, are dependent upon several different factors however, including the size of the regurgitant aperture, left ventricular compliance, and aortic diastolic pressure. Decreasing systemic vascular resistance with afterload reducing agents decreases the regurgitant fraction but also increases aortic compliance, which allows the pressures between the left

ventricle and aorta to equilibrate faster. This increases the slope (making the profile less plateau shaped) and decreases the pressure half-time of the regurgitant jet flow profile giving the false impression that the regurgitant fraction has worsened. Increased afterload generally increases the regurgitant fraction, but slope and pressure half-times are not affected to any great degree because both ventricular and aortic compliance decrease to relatively the same degree (155,156).
Comparing PHT before and after afterload reduction is not a valid comparison.
The amounts of regurgitation and regurgitant fraction are directly related to changes in the orifice size and influence ventricular size, slope, and pressure half-time. However, when there are changes in afterload secondary to drug therapy or other disease processes, slope and pressure half-time are no longer directly related to regurgitant volume. Clinical relief of symptoms is a better indicator of reduction in regurgitant volume than slopes and pressure half-times after afterload reduction has been initiated (156).
Regurgitant Volume and Fraction
Quantitative methods can determine regurgitant fractions and volumes. Regurgitant volume (RV) is calculated by subtracting pulmonary stroke volume from aortic stroke volume (Equation 5.20). Aortic stroke volume should be the same as pulmonary stroke volume in the normal heart. Areas of the pulmonary artery and aorta are calculated by Equations 5.17 and 5.18. Their diameters are measured at the level of the valves. Area is then multiplied by the flow velocity integrals of each vessel (Equations 5.19 and 5.21). Flow velocity integrals are obtained with PW Doppler at the level of the valve (1,112). Regurgitant fraction (RF) reflects the percent of volume regurgitating (Equation 5.22).
Equation 5.20 
Equation 5.21 
Equation 5.22 
Where r = radius of the artery in cm, SV = stroke volume in ml, and AR = aortic regurgitation. Refer to Chapter 4 for more information regarding the calculation of stroke volume.
Total stroke volume (aortic volume) can also be calculated from two-dimensional measurement of left ventricular volume using Simpson’s rule. Effective regurgitant orifice area (EROA) is calculated by multiplying the regurgitant volume by the CW flow velocity integral of the aortic regurgitant jet (Figure 5.76, Equation 5.23).
Equation 5.23 
Figure 5.76 Tracing the flow velocity integral of the aortic regurgitant jet allows calculation of effective regurgitant orifice area. See text for details. AR = aortic regurgitation, AR Vmax = maximum velocity of AR, AR Vmean = mean velocity of AR, AR max PG = maximum pressure gradient of AR, AR mean PG = mean pressure gradient of AR, AR VTI = velocity time integral of AR, HR = heart rate.

An effective regurgitant orifice size of ≥.3 cm2 and a regurgitant volume of ≥60 ml are both consistent with severe regurgitation in man (1,112).
This quantitative method is not accurate when the aortic valves are stenotic. The presence of a ventricular septal defect or atrial septal defect increases volume through the pulmonary artery, and valvular regurgitation affects stroke volume through the leaky valve, all of which make these calculations inaccurate (131).
Studies in man have shown that the errors inherent in deriving regurgitant fraction by measuring cross-sectional areas may be avoided by simply using flow velocity integrals. Normal human individuals have a ratio of 0.77 of mitral valve flow integral to left ventricular outflow tract flow integral. Regurgitant fraction is estimated by applying Equation 5.24 (157). This has not been studied in animals at this time.
Equation 5.24
Flow Velocity Integral
Trans MV flow / LVOT integral ratio
= .77 normally
Becomes smaller with more significant AR
Diastolic Flow Reversal
The use of transesophageal echocardiography adds another parameter that can be used to evaluate the severity of aortic regurgitation. Spectral analysis of flow in the descending aorta determines whether there is significant reversal of flow in the aorta during diastole. There is normally a trivial amount of flow reversal during early diastole in the descending aorta (1). A holodiastolic reversal of flow is a sign of at least moderate regurgitation. When the retrograde flow velocity integral is higher than systolic forward flow velocity integral in the descending aorta, the hemodynamic significance of the regurgitation is considerable (1,158,159).

Regurgitant Jet Appearance
Difficulty obtaining a complete envelope and the presence of a light regurgitant flow profile imply a mild degree of aortic regurgitation. There is too much overlap in flow profile density when regurgitation becomes moderate and severe to use this parameter in the assessment of aortic regurgitation (1).
Aortic valve lesions may also create an obstruction to outflow. When they do so the effects on the heart will include hypertrophy of the wall and septum. A pressure gradient can be derived by applying the Bernoulli equation to the flow velocity through the stenotic area. Realize that the regurgitant volume if present affects volume and resulting pressure gradient.
Overall Assessment of Aortic Regurgitation
There is no single method of assessing the severity of aortic regurgitation that is considered to be precise. A combination of the above methods that include two-dimensional, M-mode, and color-flow and spectral Doppler should be evaluated, and an overall assessment of hemodynamic significance should be determined. An index of significance for aortic regurgitation has been proposed by Chin et al. (150). Using vena contracta, jet color jet height ratio to left ventricular outflow tract height, spectral signal strength, diastolic flow reversal in the descending aorta and pressure half-time, points are assigned to each parameter. The average of these points are used to classify the regurgitation into classes of severity. The correlation to more time-consuming quantitative methods of assessment was high. Table 5.4 lists the parameters and grading system.
Table 5.4
Aortic Regurgitation Index
Adapted from: Chin C, Chen C, Chen C, et al. Prediction of Severity of Isolated Aortic Regurgitation by Echocardiography: An Aortic Regurgitation Index Study. J Am Soc Echocardiogr 2005;18:1007–1013.
When aortic regurgitation appears to be hemodynamically significant, all of the following parameters should be evaluated and integrated into the assessment of severity: left ventricular size, left ventricular function, proximal jet width, pressure half-time, vena contracta, and aortic flow velocity (1). The Society of Echocardiography Task Force on the Assessment of Native Valvular Regurgitation in man has compiled recommendations for the assessment of aortic regurgitation, as shown in Table 5.5. Several parameters are very specific for severity (jet height to outflow tract area, vena contracta, and diastolic flow reversal in the descending aorta), while others are supportive in the assessment of severity (pressure half-time, left ventricular size). They also recommend quantitative measurement of aortic regurgitant volume and fraction if there is no consensus when using the less quantitative methods (1).
