
- •Preface
- •Acknowledgments
- •Basic Physics
- •Transducers and Resolution
- •Doppler Physics
- •Artifacts
- •Summary
- •Introduction
- •Patient Preparation
- •Patient Positioning
- •Transducer Selection
- •Two-Dimensional Images
- •Two-Dimensional Imaging Controls
- •Introduction
- •M-Mode Echocardiography
- •Color-Flow Doppler
- •Spectral Doppler
- •Tissue Doppler Imaging
- •Measurement and Assessment of Two-Dimensional Images
- •Measurement and Assessment of M-Mode Images
- •Measurement and Assessment of Spectral Doppler Flow
- •Measurement and Assessment of Tissue Doppler Imaging
- •Evaluation of Color-Flow Doppler
- •Evaluation of Ventricular Function
- •Mitral Regurgitation
- •Aortic Regurgitation
- •Tricuspid Regurgitation
- •Pulmonary Regurgitation
- •Endocarditis
- •Pulmonary Hypertension
- •Systemic Hypertension
- •Hypertrophic Cardiomyopathy
- •Dynamic Right Ventricular Outflow Obstruction
- •Moderator Bands
- •Dilated Cardiomyopathy
- •Right Ventricular Cardiomyopathy
- •Restrictive Cardiomyopathy
- •Endocardial Fibroelastosis
- •Arrhythmogenic Right Ventricular Cardiomyopathy
- •Myocardial Infarction
- •Myocardial Contusions
- •Pericardial Effusion
- •Neoplasia as a Cause of Pericardial Effusion
- •Pericardial Disease
- •Abscesses
- •Pericardial Cysts
- •Thrombus
- •Ventricular Septal Defect
- •Patent Ductus Arteriosus
- •Aorticopulmonary Window
- •Right to Left Shunting PDA
- •Atrial Septal Defects
- •Endocardial Cushion Defects
- •Bubble Studies
- •Atrioventricular Valve Dysplasia
- •Outflow Obstructions
- •Inflow Obstructions
- •Tetralogy of Fallot
- •APPENDIX ONE Bovine
- •APPENDIX TWO Canine
- •APPENDIX THREE Equine
- •APPENDIX FOUR Feline
- •APPENDIX FIVE Miscellaneous Species
- •Index
Parameters Very Specific for Assessment of AR
Jet height to LVOT width ratio
Vena contracta
Diastolic flow reversal in descending aorta
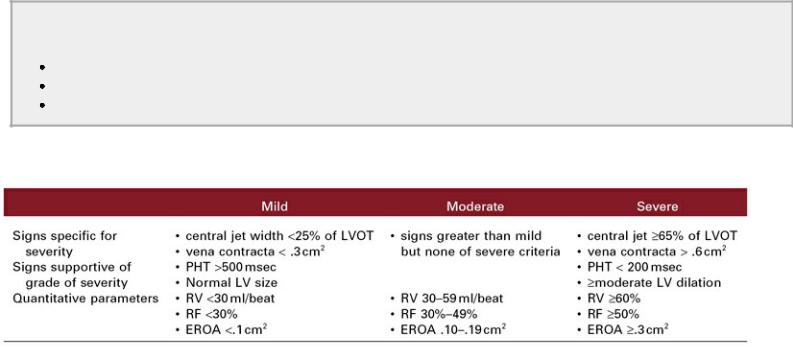
Table 5.5
Aortic Regurgitation: Parameters for the Assessment of Severity in Man
Adapted from: Zoghbi W, Enriquez-Sarano M, Foster E, et al. American Society of Echocardiography. Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography. J Am Soc Echocardiogr 2003;16:777–802.
Tricuspid Regurgitation
Degenerative valvular disease involving the tricuspid valve occurs less commonly than myxomatous degeneration of the mitral valve and when it does, it is generally in addition to the left-sided valvular disease. A high percentage of normal animals have trivial to mild tricuspid insufficiency, and this should not be mistaken for tricuspid valve disease. Chapter 3 discusses the incidence of normal valvular leaks and shows some examples of normal tricuspid insufficiency in various species. Tricuspid insufficiency may be present as a consequence of chronic mitral valve insufficiency that has led to pulmonary hypertension.
Two-Dimensional and M-mode Evaluation
Assessment of the tricuspid valve is best from four-chamber parasternal or apical views. Long-axis left ventricular outflow views of the heart typically are not good enough to assess the tricuspid valve. It often looks thick when it is not. This is true in the small and large animal. The tricuspid valve may prolapse just as the mitral valve does secondary to stretch of the chordae or minor chordal rupture (Figure 5.77).
Figure 5.77 The tricuspid valve may prolapse (arrow) with tricuspid insufficiency secondary to chronic stretch or possibly ruptured minor chordae just as the mitral valve does. RV = right ventricle, LV = left ventricle, RA = right atrium, LA = left atrium, Plane = right parasternal four chamber.

The changes that tricuspid insufficiency creates in the right ventricle and atrium are of great importance when assessing the hemodynamic significance of the leaks (Figures 5.78, 5.79). The normal right ventricle is about one third the size of the left ventricular chamber on the long-axis left ventricular inflow outflow view. Once this relationship changes, tricuspid insufficiency, pulmonic insufficiency, pulmonary hypertension, or all of the above should be suspected.
Figure 5.78 This apical four-chamber view of the heart shows moderate to severe tricuspid insufficiency. The right atrium is very dilated when compared to the left atrium. RV = right ventricle, LV = left ventricle, RA = right atrium, LA = left atrium, Species = dog.
Figure 5.79 (A) Severe right atrial dilation and (B) severe tricuspid insufficiency is documented with color-flow Doppler in this horse with right ventricular cardiomyopathy. RV = right ventricle, RA = right atrium, AO = aorta, LA = left atrium.

Once diastolic pressures within the right ventricle increase and exceed left ventricular diastolic pressures, paradoxical septal motion will be seen. The motion may be subtle when pressures are fairly equal or it may be dramatic when right ventricular pressure elevation is severe (Figures 4.103, 5.80, 5.81). If there is concurrent left-sided disease that would elevate left ventricular diastolic pressure as in mitral or aortic insufficiencies then paradoxical motion will not be seen until right-sided pressure exceeds left despite a very large right ventricle (160–162).
Paradoxical Septal Motion
Seen with elevated RV diastolic pressure
Figure 5.80 Mild paradoxical septal motion (arrow) is seen on this M-mode secondary to mildly elevated right ventricular diastolic pressures. RV = right ventricle, LV = left ventricle.

Figure 5.81 Significant tricuspid insufficiency results in paradoxical septal motion due to elevated right ventricular diastolic pressures. The septum is flattened as a result of this motion (arrow). This horse also has pericardial effusion. RV = right ventricle, LV = left ventricle, PE = pericardial effusion.
Right heart dilation because of tricuspid insufficiency should be differentiated from right ventricular enlargement secondary to pulmonary hypertension. Tricuspid insufficiency will create volume overload of the right atrium and ventricle but will not enlarge the pulmonary artery (Figure 5.82). Pulmonary hypertension causes the pulmonary artery and right ventricle to dilate and eventual hypertrophy. Right atrial dilation is seen with pulmonary hypertension when the tricuspid valve becomes incompetent or filling pressure in the right ventricle is high. Paradoxical septal motion may be seen with either problem since diastolic pressure elevates with both pulmonary hypertension and tricuspid regurgitation.

RV Dilation because of TR
Little observable RVH
Normal or small PA size
RV Dilation because of Chronic Pulmonary Hypertension
Observable RVH if chronic
Dilated PA
Figure 5.82 Tricuspid insufficiency will create volume overload of the right atrium and ventricle but will not enlarge the pulmonary artery. RV = right ventricle, TV = tricuspid valve, RA = right atrium, AO = aorta, PV = pulmonary valve. PA = pulmonary artery.
Evaluating the vena cava as it crosses the diaphragm is a way to subjectively assess right atrial pressure. Atrial pressure is estimated to be 5 mm Hg or less when there is no evidence of right atrial dilation and the vena cava collapses completely with respiration (Figure 5.52). The right atrium has an estimated pressure of approximately 10 mm Hg if there is right atrial dilation, no evidence of rightsided congestive heart failure and the vena cava collapses approximately 50% with respiration. When the vena cava does not collapse with respiration and there is evidence of right-sided congestive heart failure, right atrial pressure is estimated at ≥15 mm Hg (13,80,106,107).
Color-Flow Doppler Imaging
Color-flow Doppler assessment using tricuspid regurgitation jet area is less reliable than for mitral regurgitation. However, jets that extend deep into the right atrial chamber are associated with significant regurgitation (Figure 5.83) (1). Eccentric jets are common and multiple imaging planes should be used, including left apical and cranial views of the tricuspid valve.
Figure 5.83 (A) Mild tricuspid regurgitation (arrow) is present in this cat. (B) A moderate amount of tricuspid regurgitation is seen in this heart. (C) Severe tricuspid regurgitation is seen on this apical four-chamber view of the heart in a dog. RV = right ventricle, RA = right atrium, AO = aorta, LA = left atrium, LV = left ventricle.

PISA is challenging at the tricuspid annulus, but the vena contracta has a high correlation with severity in man. A vena contracta width of >7 mm in man has a 93% specificity for severe tricuspid

regurgitation and is 89% sensitive (163,164).
Color-Flow Assessment
PISA difficult and inaccurate Vena contracta
>7 mm = severe TR
Spectral Doppler Imaging
Spectral Doppler can be used to determine the velocity of the regurgitant jet and estimate pressure of the right ventricle and pulmonary vascular system (165,166). Apical four-chamber views, modified apical four-chamber views, and left cranial transverse views are imaging planes that usually optimize the alignment of the tricuspid regurgitant jet and the Doppler cursor (Figure 5.84). Remember that the velocity of regurgitant flow is not representative of severity for this or any valvular insufficiency (Figure 5.84) (1). A huge regurgitant volume may often have very low velocity (<2 m/sec) when right ventricular and atrial pressures equilibrate rapidly. See Chapter 6 for further discussion of pulmonary hypertension. An early peaking velocity with a v wave may be seen in these situations (1). Additionally density of the spectral signal will be equal in the forward and the regurgitant directions when tricuspid regurgitation is severe (167).
Figure 5.84 Image several views in order to find the one that aligns a tricuspid regurgitant jet best with the Doppler cursor. Here a mild to moderate amount of tricuspid regurgitation aligns well on an apical view. This mild to moderate amount of tricuspid regurgitation has a high pressure gradient (93 mm Hg). TR Vmax = maximum velocity of tricuspid regurgitation, TR max PG = maximum pressure gradient of the tricuspid regurgitation.
The use of spectral Doppler to evaluate regurgitant fraction and volume is difficult because of significant error in measuring the tricuspid annulus. Both the inability to align trans tricuspid flow with the Doppler cursor and the asymmetric shape of the tricuspid annulus are sources of this error. Spectral Doppler is used in the hepatic vessels however and are a reflection of right atrial pressure just as pulmonary venous flow is analyzed on the left side of the heart. Systolic reversal of flow in the hepatic veins is 80% sensitive for severe regurgitation. Respiratory variation, preload, and impaired
