
- •ICU Protocols
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1: Airway Management
- •Suggested Reading
- •2: Acute Respiratory Failure
- •Suggested Reading
- •Suggested Reading
- •Website
- •4: Basic Mechanical Ventilation
- •Suggested Reading
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Websites
- •7: Weaning
- •Suggested Reading
- •8: Massive Hemoptysis
- •Suggested Reading
- •9: Pulmonary Thromboembolism
- •Suggested Reading
- •Suggested Reading
- •Websites
- •11: Ventilator-Associated Pneumonia
- •Suggested Readings
- •12: Pleural Diseases
- •Suggested Reading
- •Websites
- •13: Sleep-Disordered Breathing
- •Suggested Reading
- •Websites
- •14: Oxygen Therapy
- •Suggested Reading
- •15: Pulse Oximetry and Capnography
- •Conclusion
- •Suggested Reading
- •Websites
- •16: Hemodynamic Monitoring
- •Suggested Reading
- •Websites
- •17: Echocardiography
- •Suggested Readings
- •Websites
- •Suggested Reading
- •Websites
- •19: Cardiorespiratory Arrest
- •Suggested Reading
- •Websites
- •20: Cardiogenic Shock
- •Suggested Reading
- •21: Acute Heart Failure
- •Suggested Reading
- •22: Cardiac Arrhythmias
- •Suggested Reading
- •Website
- •23: Acute Coronary Syndromes
- •Suggested Reading
- •Website
- •Suggested Reading
- •25: Aortic Dissection
- •Suggested Reading
- •26: Cerebrovascular Accident
- •Suggested Reading
- •Websites
- •27: Subarachnoid Hemorrhage
- •Suggested Reading
- •Websites
- •28: Status Epilepticus
- •Suggested Reading
- •29: Acute Flaccid Paralysis
- •Suggested Readings
- •30: Coma
- •Suggested Reading
- •Suggested Reading
- •Websites
- •32: Acute Febrile Encephalopathy
- •Suggested Reading
- •33: Sedation and Analgesia
- •Suggested Reading
- •Websites
- •34: Brain Death
- •Suggested Reading
- •Websites
- •35: Upper Gastrointestinal Bleeding
- •Suggested Reading
- •36: Lower Gastrointestinal Bleeding
- •Suggested Reading
- •37: Acute Diarrhea
- •Suggested Reading
- •38: Acute Abdominal Distension
- •Suggested Reading
- •39: Intra-abdominal Hypertension
- •Suggested Reading
- •Website
- •40: Acute Pancreatitis
- •Suggested Reading
- •Website
- •41: Acute Liver Failure
- •Suggested Reading
- •Suggested Reading
- •Websites
- •43: Nutrition Support
- •Suggested Reading
- •44: Acute Renal Failure
- •Suggested Reading
- •Websites
- •45: Renal Replacement Therapy
- •Suggested Reading
- •Website
- •46: Managing a Patient on Dialysis
- •Suggested Reading
- •Websites
- •47: Drug Dosing
- •Suggested Reading
- •Websites
- •48: General Measures of Infection Control
- •Suggested Reading
- •Websites
- •49: Antibiotic Stewardship
- •Suggested Reading
- •Website
- •50: Septic Shock
- •Suggested Reading
- •51: Severe Tropical Infections
- •Suggested Reading
- •Websites
- •52: New-Onset Fever
- •Suggested Reading
- •Websites
- •53: Fungal Infections
- •Suggested Reading
- •Suggested Reading
- •Website
- •55: Hyponatremia
- •Suggested Reading
- •56: Hypernatremia
- •Suggested Reading
- •57: Hypokalemia and Hyperkalemia
- •57.1 Hyperkalemia
- •Suggested Reading
- •Website
- •58: Arterial Blood Gases
- •Suggested Reading
- •Websites
- •59: Diabetic Emergencies
- •59.1 Hyperglycemic Emergencies
- •59.2 Hypoglycemia
- •Suggested Reading
- •60: Glycemic Control in the ICU
- •Suggested Reading
- •61: Transfusion Practices and Complications
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Website
- •63: Onco-emergencies
- •63.1 Hypercalcemia
- •63.2 ECG Changes in Hypercalcemia
- •63.3 Superior Vena Cava Syndrome
- •63.4 Malignant Spinal Cord Compression
- •Suggested Reading
- •64: General Management of Trauma
- •Suggested Reading
- •65: Severe Head and Spinal Cord Injury
- •Suggested Reading
- •Websites
- •66: Torso Trauma
- •Suggested Reading
- •Websites
- •67: Burn Management
- •Suggested Reading
- •68: General Poisoning Management
- •Suggested Reading
- •69: Syndromic Approach to Poisoning
- •Suggested Reading
- •Websites
- •70: Drug Abuse
- •Suggested Reading
- •71: Snakebite
- •Suggested Reading
- •72: Heat Stroke and Hypothermia
- •72.1 Heat Stroke
- •72.2 Hypothermia
- •Suggested Reading
- •73: Jaundice in Pregnancy
- •Suggested Reading
- •Suggested Reading
- •75: Severe Preeclampsia
- •Suggested Reading
- •76: General Issues in Perioperative Care
- •Suggested Reading
- •Web Site
- •77.1 Cardiac Surgery
- •77.2 Thoracic Surgery
- •77.3 Neurosurgery
- •Suggested Reading
- •78: Initial Assessment and Resuscitation
- •Suggested Reading
- •79: Comprehensive ICU Care
- •Suggested Reading
- •Website
- •80: Quality Control
- •Suggested Reading
- •Websites
- •81: Ethical Principles in End-of-Life Care
- •Suggested Reading
- •82: ICU Organization and Training
- •Suggested Reading
- •Website
- •83: Transportation of Critically Ill Patients
- •83.1 Intrahospital Transport
- •83.2 Interhospital Transport
- •Suggested Reading
- •84: Scoring Systems
- •Suggested Reading
- •Websites
- •85: Mechanical Ventilation
- •Suggested Reading
- •86: Acute Severe Asthma
- •Suggested Reading
- •87: Status Epilepticus
- •Suggested Reading
- •88: Severe Sepsis and Septic Shock
- •Suggested Reading
- •89: Acute Intracranial Hypertension
- •Suggested Reading
- •90: Multiorgan Failure
- •90.1 Concurrent Management of Hepatic Dysfunction
- •Suggested Readings
- •91: Central Line Placement
- •Suggested Reading
- •92: Arterial Catheterization
- •Suggested Reading
- •93: Pulmonary Artery Catheterization
- •Suggested Reading
- •Website
- •Suggested Reading
- •95: Temporary Pacemaker Insertion
- •Suggested Reading
- •96: Percutaneous Tracheostomy
- •Suggested Reading
- •97: Thoracentesis
- •Suggested Reading
- •98: Chest Tube Placement
- •Suggested Reading
- •99: Pericardiocentesis
- •Suggested Reading
- •100: Lumbar Puncture
- •Suggested Reading
- •Website
- •101: Intra-aortic Balloon Pump
- •Suggested Reading
- •Appendices
- •Appendix A
- •Appendix B
- •Common ICU Formulae
- •Appendix C
- •Appendix D: Syllabus for ICU Training
- •Index
Hyponatremia |
55 |
|
Rajesh Chawla, Subhash Todi,
and Devendra Kumar Agarwal
A 67-year-old chronic male smoker, a known case of small cell carcinoma, was admitted to hospital with altered sensorium, nausea, and dizziness. His vital signs were stable. Liver function tests, urea, and creatinine were normal. Serum sodium was 118 mEq/L and serum potassium was 3.0 mEq/L.
Hyponatremia is a very common condition encountered in the ICU in isolation or as a complication of underlying medical illness. Hyponatremia is deÞned as serum sodium less than 135 mEq/L. It is considered severe if serum sodium is less than 125 mEq/L. Too rapid correction can result in neurological complications.
Step 1: Initiate resuscitation (refer to Chap. 78)
¥Assess and secure the airway in a patient with severe hyponatremia who cannot maintain airway.
¥The patient may require assisted ventilatory support.
¥Put a peripheral line and resuscitate with suitable ßuids as deemed necessary.
¥In the hyponatremia patient, initial ßuid resuscitation should be done cautiously.
R. Chawla, M.D., F.C.C.M., F.C.C.P. (*)
Department of Respiratory, Critical Care & Sleep Medicine, Indraprastha Apollo Hospitals, New Delhi, India
e-mail: drchawla@hotmail.com
S. Todi, M.D., M.R.C.P.
Critical Care & Emergency, A.M.R.I. Hospital, Kolkata, India e-mail: drsubhashtodi@gmail.com
D.K. Agarwal, M.D., D.M.
Department of Nephrology, Indraprastha Apollo Hospitals, New Delhi, India
R. Chawla and S. Todi (eds.), ICU Protocols: A stepwise approach, |
433 |
DOI 10.1007/978-81-322-0535-7_55, © Springer India 2012 |
|
434 |
|
|
|
|
|
|
|
|
|
|
|
R. Chawla et al. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Hyponatremia |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
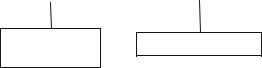
Normal/high plasma osmolality |
|
|
|
|
Low plasma osmolality |
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Translocational |
|
Peudohyponatremia |
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Glucose, mannitol, glycine, maltose
Protein, lipids
Fig. 55.1 Diagnostic approach to hyponatremia
Step 2: Take focused history and perform physical examination
¥This should be done to assess severity of hyponatremia and urgency of correction.
¥Pay immediate attention to neurological symptoms such as disorientation, drowsiness, impaired consciousness, or seizures irrespective of duration of hyponatremia.
¥Other symptoms of hyponatremia are anorexia, nausea, dizziness, and lack of balance.
¥Examine previous records of serum sodium to assess chronicity.
¥Take drug history, especially for thiazide diuretics.
¥Ask for history suggestive of ßuid loss such as vomiting, diarrhea, or excessive water intake.
¥Look for features of ßuid overload such as pedal edema, ascites, and pleural effusion.
Step 3: Identify etiology
¥Assess volume status, measure serum and urine osmolality, and measure spot urine sodium (see Table 55.1 and Fig. 55.2).
¥Calculate serum osmolality:
Ð 2 × [Na] + [glucose mg/dL]/18 + [BUN mg/dL]/2.8.
¥Normal: 275Ð290 mOsm/kg.
¥Serum osmolarity should always be measured rather than calculated to differentiate hypo-, hyper-, and iso-osmolar types of hyponatremia (Fig. 55.1).
¥A patient with true hyponatremia will have low serum osmolality.
¥Urine osmolality of less than 100 mOsm/kg: with low serum osmolarity: suggests excess water intake.
¥Urine osmolality of more than 100 mOsm/kg: impaired renal excretion of water (eg. CCF, cirrhosis of liver, prerenal renal failure) or salt (eg. salt loosing nephropathy).
¥Urine osmolality may be calculated by the last two digits of urine speciÞc gravity × 30.

55 Hyponatremia |
|
|
|
|
|
|
|
|
|
435 |
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
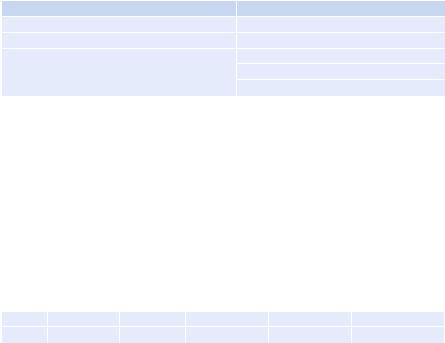
Patient of hyponatremia |
|
|
|||
|
|
|
|
|
|
|
Measure spot urinary Na+ |
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
Urinary Na+< 20 |
|
|
|
|
Urinary Na > 20 |
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Assess volume status |
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Hypovolemia |
|
|
|
Hypervolemia |
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Extrarenal cause |
|
|
|
|
|
|
|
|
|
|
|
|
• Vomiting |
|
|
|
- Cirrhosis |
|
|
|||||
|
• Diarrhea |
|
|
|
- Nephrotic syndrome |
|
|
|||||
|
• Burns |
|
|
|
- Cardiac failure |
|
|
|||||
•Pancreatitis
•Trauma
•Third spacing of
fluids
|
|
|
|
|
Assess volume status |
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
Hypovolemia |
|
|
|
|
Euvolemia |
|
|
Hyperovolemia |
|
||
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Renal losses |
|
|
• Syndrome of |
|
|
Hypervolemia |
||||||
• Diuretic excess |
|
|
inappropriate |
|
|
|||||||
|
|
|
|
- Acute or chronic |
||||||||
• Mineralocorticoid deficiency |
|
|
antidiuretic hormone |
|
|
|||||||
|
|
|
|
renal failure |
||||||||
• Salt-losing states |
|
|
(SIADH) secretion |
|
|
|||||||
|
|
|
|
|
|
|||||||
Bicarbonaturia with renal tubal |
|
|
• Reset osmostat |
|
|
|
|
|||||
acidosis (RTA)and metabolic |
|
|
• Psychogenic polydipsia |
|
|
|
|
|||||
alkalosis |
|
|
• Hypothyroidism, adrenal |
|
|
|
|
|||||
• Ketonuria |
|
|
insufficiency |
|
|
|
|
|||||
• Osmotic diuresis |
|
|
• Glucocorticoid |
|
|
|
|
|||||
• Cerebral salt wasting |
|
|
deficiency |
|
|
|
|
|||||
Fig. 55.2 Diagnostic approach to hyponatremiaÑmeasure urinary sodium and assess volume status
¥Measure spot urine sodium: less than 20 mEq/L or more than 20 mEq/L.
¥Measurement of spot urinary sodium and assessment of the volume status can help to know the etiology (Fig. 55.2).
Step 4: Assess severity of hyponatremia
¥Mild hyponatremiaÑ130Ð135 mmol/L
¥Moderate hyponatremiaÑ125Ð130 mmol/L
¥Severe hyponatremiaÑless than 125 mmol/L
Step 5: Send further investigations
In addition to serum osmolality, urine osmolality, and urinary sodium, send further investigations to ascertain the cause and severity of hyponatremia.
436 |
R. Chawla et al. |
|
|
¥Serum K, Cl, bicarbonate
¥Serum glucose, urea, creatinine, total proteins, triglycerides, uric acid
¥Arterial blood gases
¥Serum TSH, cortisol
¥UrineÑcreatinine, uric acid
¥Fractionated excretion of sodium (FE Na) = (U Na × P Cr)/(P Na × U Cr) × 100
Step 6: Correct serum sodium
¥Treatment of hyponatremia must be individualized.
¥Factors to be considered are as follows:
ÐSeverity
ÐDuration
ÐSymptoms
¥Risks of treatment (osmotic demyelination) should be balanced against beneÞt (see Table 55.1). Too rapid correction of sodium is the most important risk factor for the development of osmotic demyelination syndrome.
Table 55.1 Risk factors of neurological complications in hyponatremia
Acute cerebral edema |
Osmotic demyelination syndrome |
Postoperative patients and young females |
Too rapid correction of sodium |
Children |
Malnourished patients |
Psychiatric polydipsic patients |
Alcoholics |
|
Burn patients |
|
Elderly women taking thiazides |
Step 7: Determine the rate of correction of sodium
¥In asymptomatic patients, the rate of correction should not be more than 0.5Ð 1.00 meq/L/h and less than 12 meq over the Þrst 24 h.
¥Avoid overcorrection of serum sodium concentration.
¥In symptomatic patients, sodium may be corrected at the rate of 1Ð2 mEq/L for an initial few hours or till seizure subsides.
Step 8: Calculate sodium deficit and rate of rise of sodium
¥Sodium deÞcit = total body water (TBW) × (desired serum Na − measured serum Na)
¥TBW = body weight (kg) × Y.
Y = |
Children |
Adult men |
Adult women |
Elderly men |
Elderly women |
|
0.6 |
0.6 |
0.5 |
0.5 |
0.45 |
¥The main use of this formula is in the volume depletion state and in SIADH to estimate initial rate of ßuid administration.
For example, in a 60-kg woman with a serum sodium of 115 mEq/L with a goal
of increasing sodium by 8 mEq/L in Þrst 24 h,
55 Hyponatremia |
437 |
|
|
Sodium deÞcit = (60 × 0.5) × (123−115) = 240 mEq.
¥Three percent hypertonic saline contains approximately 500 mEq of sodium per liter or 1 mEq per 2 mL. So, 480 mL (240 meq of sodium) of hypertonic saline given over 24 h or 20 mL/h will raise serum sodium by 8 mEq (from 115 meq/L to 123 meq/L in 24 h or 0.25 mEq/h.
¥This should be conÞrmed by serial measurements of serum sodium.
¥ Increase in serum sodium by any ßuid = (infusate sodium − serum sodium)/ TBW + 1.
¥In cases when potassium is added to intravenous ßuid, increase in serum sodium = [(infusate sodium + potassium) − (serum sodium)]/TBW + 1.
For example, in a 60-kg woman with a serum sodium of 110 mEq/L, if 1 L of
isotonic saline (containing 154 mEq/L of sodium) is administered, the estimated rise of serum sodium will be
(154 − 110)/(30 + 1) = 1.4 mEq/L.
That is, serum sodium will be 111.4 mEq/L after giving 1 L of normal saline.
¥Rule of thumb
ÐFor hypertonic (3%) saline
ÐInfusion rate = weight (kg) × desired rate of correction For example, to correct at 1 mEq/L/h in a 50-kg person,
ÐInfusion rate = 50 × 1 = 50 mL/h.
To correct at 0.5 mEq/L/h in a 70-kg person,
ÐInfusion rate = 70 × 0.5 = 35 mL/h.
¥For isotonic (0.9%) saline,
Ð0.9 NaCl corrects at 1Ð2 mEq/L for every 1 L of NaCl.
¥Remember that these formulas are just an approximation as they do not take into account translocation of water, correction of underlying cause, or ongoing water loss.
¥Rise of sodium should always be veriÞed by repeated sodium measurement.
Step 9: Euvolemic, hypoosmolar, hyponatremia
Consider SIADH
¥Clinical euvolumia
¥Urine osmolality more than 300 mOsm/kg H2O
¥Urinary sodium concentration more than 40 mmol/L
¥Normal renal, hepatic, adrenal, and thyroid function
¥Serum osmolality less than 275 mOsm/kg H2O
¥Serum sodium less than 134 mEq/L
¥In severely symptomatic patients:
ÐGive 3% hypertonic saline
ÐCheck serum sodium frequently
¥In asymptomatic and mildly symptomatic patients:
ÐRestrict total water intake approximately to 600Ð1,000 mL/day (intake = 50% of output).
438 |
R. Chawla et al. |
|
|
ÐAddition of salt to diet.
ÐLoop diuretics may be added if urine output very low.
ÐConsider vasopressin antagonist (vaptans), if available.
ÐDemeclocycline 600Ð1,200 mg/day.
ÐIn all cases of SIADH, correct the underlying cause and withdraw any offending drug.
¥Other causes of euvolemic, hypo-osmolar hyponatremia such as hypothyroid, adrenal insufÞciency, renal disease, and psychogenic polydipsia should be managed by water restriction, hormone replacement, and treatment of the underlying disease
Step 10: Hypervolemic, hypoosmolar, hyponatremia
¥Consider edematous states such as cirrhosis, nephrotic syndrome, cardiac failure, and renal failure.
¥These should be managed by the following:
ÐFluid restriction
ÐLoop diuretics
ÐTreating the underlying disease
ÐAvoiding extra sodium
Step 11: Hypovolemic, hypoosmolar, hyponatremia
¥Consider the volume-depleted state (renal or extrarenal).
¥These should be managed by the following:
ÐVolume replacement
ÐTreating the underlying disease
Diuretic-Induced Hyponatremia
¥This may mimic SIADH, as it may be clinically euvolemic.
¥Occurs predominantly with thiazide diuretics.
¥May occur within a few days of starting diuretics.
¥Elderly patients with low body mass are more vulnerable.
¥May be associated with increased water intake.
¥Managed by stopping diuretics, isotonic or hypertonic saline, in symptomatic patients.
¥At high risk of rapid correction after stopping diuretics.
¥Careful monitoring is required to avoid osmotic demyelination.
Cerebral Salt Wasting (CSW)
¥This may mimic SIADH as laboratory Þndings are similar.
¥Hyponatremia with a low plasma osmolality.
¥An inappropriately elevated urine osmolality (>100 mOsm/kg and usually >300 mOsm/kg).
¥A urine sodium concentration above 40 mEq/L.
¥Much less common than SIADH.
¥Occurs with acute CNS disease, mainly subarachnoid hemorrhage.
¥Clinically hypovolemic.
