
- •ICU Protocols
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1: Airway Management
- •Suggested Reading
- •2: Acute Respiratory Failure
- •Suggested Reading
- •Suggested Reading
- •Website
- •4: Basic Mechanical Ventilation
- •Suggested Reading
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Websites
- •7: Weaning
- •Suggested Reading
- •8: Massive Hemoptysis
- •Suggested Reading
- •9: Pulmonary Thromboembolism
- •Suggested Reading
- •Suggested Reading
- •Websites
- •11: Ventilator-Associated Pneumonia
- •Suggested Readings
- •12: Pleural Diseases
- •Suggested Reading
- •Websites
- •13: Sleep-Disordered Breathing
- •Suggested Reading
- •Websites
- •14: Oxygen Therapy
- •Suggested Reading
- •15: Pulse Oximetry and Capnography
- •Conclusion
- •Suggested Reading
- •Websites
- •16: Hemodynamic Monitoring
- •Suggested Reading
- •Websites
- •17: Echocardiography
- •Suggested Readings
- •Websites
- •Suggested Reading
- •Websites
- •19: Cardiorespiratory Arrest
- •Suggested Reading
- •Websites
- •20: Cardiogenic Shock
- •Suggested Reading
- •21: Acute Heart Failure
- •Suggested Reading
- •22: Cardiac Arrhythmias
- •Suggested Reading
- •Website
- •23: Acute Coronary Syndromes
- •Suggested Reading
- •Website
- •Suggested Reading
- •25: Aortic Dissection
- •Suggested Reading
- •26: Cerebrovascular Accident
- •Suggested Reading
- •Websites
- •27: Subarachnoid Hemorrhage
- •Suggested Reading
- •Websites
- •28: Status Epilepticus
- •Suggested Reading
- •29: Acute Flaccid Paralysis
- •Suggested Readings
- •30: Coma
- •Suggested Reading
- •Suggested Reading
- •Websites
- •32: Acute Febrile Encephalopathy
- •Suggested Reading
- •33: Sedation and Analgesia
- •Suggested Reading
- •Websites
- •34: Brain Death
- •Suggested Reading
- •Websites
- •35: Upper Gastrointestinal Bleeding
- •Suggested Reading
- •36: Lower Gastrointestinal Bleeding
- •Suggested Reading
- •37: Acute Diarrhea
- •Suggested Reading
- •38: Acute Abdominal Distension
- •Suggested Reading
- •39: Intra-abdominal Hypertension
- •Suggested Reading
- •Website
- •40: Acute Pancreatitis
- •Suggested Reading
- •Website
- •41: Acute Liver Failure
- •Suggested Reading
- •Suggested Reading
- •Websites
- •43: Nutrition Support
- •Suggested Reading
- •44: Acute Renal Failure
- •Suggested Reading
- •Websites
- •45: Renal Replacement Therapy
- •Suggested Reading
- •Website
- •46: Managing a Patient on Dialysis
- •Suggested Reading
- •Websites
- •47: Drug Dosing
- •Suggested Reading
- •Websites
- •48: General Measures of Infection Control
- •Suggested Reading
- •Websites
- •49: Antibiotic Stewardship
- •Suggested Reading
- •Website
- •50: Septic Shock
- •Suggested Reading
- •51: Severe Tropical Infections
- •Suggested Reading
- •Websites
- •52: New-Onset Fever
- •Suggested Reading
- •Websites
- •53: Fungal Infections
- •Suggested Reading
- •Suggested Reading
- •Website
- •55: Hyponatremia
- •Suggested Reading
- •56: Hypernatremia
- •Suggested Reading
- •57: Hypokalemia and Hyperkalemia
- •57.1 Hyperkalemia
- •Suggested Reading
- •Website
- •58: Arterial Blood Gases
- •Suggested Reading
- •Websites
- •59: Diabetic Emergencies
- •59.1 Hyperglycemic Emergencies
- •59.2 Hypoglycemia
- •Suggested Reading
- •60: Glycemic Control in the ICU
- •Suggested Reading
- •61: Transfusion Practices and Complications
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Website
- •63: Onco-emergencies
- •63.1 Hypercalcemia
- •63.2 ECG Changes in Hypercalcemia
- •63.3 Superior Vena Cava Syndrome
- •63.4 Malignant Spinal Cord Compression
- •Suggested Reading
- •64: General Management of Trauma
- •Suggested Reading
- •65: Severe Head and Spinal Cord Injury
- •Suggested Reading
- •Websites
- •66: Torso Trauma
- •Suggested Reading
- •Websites
- •67: Burn Management
- •Suggested Reading
- •68: General Poisoning Management
- •Suggested Reading
- •69: Syndromic Approach to Poisoning
- •Suggested Reading
- •Websites
- •70: Drug Abuse
- •Suggested Reading
- •71: Snakebite
- •Suggested Reading
- •72: Heat Stroke and Hypothermia
- •72.1 Heat Stroke
- •72.2 Hypothermia
- •Suggested Reading
- •73: Jaundice in Pregnancy
- •Suggested Reading
- •Suggested Reading
- •75: Severe Preeclampsia
- •Suggested Reading
- •76: General Issues in Perioperative Care
- •Suggested Reading
- •Web Site
- •77.1 Cardiac Surgery
- •77.2 Thoracic Surgery
- •77.3 Neurosurgery
- •Suggested Reading
- •78: Initial Assessment and Resuscitation
- •Suggested Reading
- •79: Comprehensive ICU Care
- •Suggested Reading
- •Website
- •80: Quality Control
- •Suggested Reading
- •Websites
- •81: Ethical Principles in End-of-Life Care
- •Suggested Reading
- •82: ICU Organization and Training
- •Suggested Reading
- •Website
- •83: Transportation of Critically Ill Patients
- •83.1 Intrahospital Transport
- •83.2 Interhospital Transport
- •Suggested Reading
- •84: Scoring Systems
- •Suggested Reading
- •Websites
- •85: Mechanical Ventilation
- •Suggested Reading
- •86: Acute Severe Asthma
- •Suggested Reading
- •87: Status Epilepticus
- •Suggested Reading
- •88: Severe Sepsis and Septic Shock
- •Suggested Reading
- •89: Acute Intracranial Hypertension
- •Suggested Reading
- •90: Multiorgan Failure
- •90.1 Concurrent Management of Hepatic Dysfunction
- •Suggested Readings
- •91: Central Line Placement
- •Suggested Reading
- •92: Arterial Catheterization
- •Suggested Reading
- •93: Pulmonary Artery Catheterization
- •Suggested Reading
- •Website
- •Suggested Reading
- •95: Temporary Pacemaker Insertion
- •Suggested Reading
- •96: Percutaneous Tracheostomy
- •Suggested Reading
- •97: Thoracentesis
- •Suggested Reading
- •98: Chest Tube Placement
- •Suggested Reading
- •99: Pericardiocentesis
- •Suggested Reading
- •100: Lumbar Puncture
- •Suggested Reading
- •Website
- •101: Intra-aortic Balloon Pump
- •Suggested Reading
- •Appendices
- •Appendix A
- •Appendix B
- •Common ICU Formulae
- •Appendix C
- •Appendix D: Syllabus for ICU Training
- •Index
New-Onset Fever |
52 |
|
|
Subhash Todi and Rajesh Chawla |
|
A 70-year-old male patient was admitted to the ICU with hemorrhagic stroke. On the fifth day of admission, he spiked a fever of 100°F orally. He was not intubated and had an indwelling urinary catheter, peripheral intravenous cannula, and a nasogastric tube. His sensorium remained unchanged, and he was hemodynamically stable.
New onset of fever is an everyday problem encountered in the ICU. The reason could be manifold such as noninfectious cause, mild infection, or an initial presentation of severe infection. This should trigger a careful clinical assessment and a systematic approach to differentiate these possibilities.
Step 1: Record temperature
•All patients in the ICU should have, as a minimum, hourly temperature recorded and charted in the nursing record as per the ICU protocol.
•The site of recorded temperature should be marked in the nursing chart (O = oral, R = rectal, A = axillary, T = tympanic).
•All ICUs should have access to a core temperature measurement device (tympanic, rectal), properly calibrated and sterilized.
•Temperature may be recorded as centigrade or Fahrenheit.
•Uniformity of the scale should be maintained.
S. Todi, M.D., M.R.C.P. (*)
Critical Care & Emergency, A.M.R.I. Hospital, Kolkata, India e-mail: drsubhashtodi@gmail.com
R. Chawla, M.D., F.C.C.M.
Department of Respiratory, Critical Care & Sleep Medicine, Indraprastha Apollo Hospitals, New Delhi, India
e-mail: drchawla@hotmail.com
R. Chawla and S. Todi (eds.), ICU Protocols: A stepwise approach, |
411 |
DOI 10.1007/978-81-322-0535-7_52, © Springer India 2012 |
|

412 |
S. Todi and R. Chawla |
|
|
•In immunocompetent patients who are stable, temperature below 101°F in which clinical examination does not reveal any definite source of fever may be observed for a few hours before initiating investigation.
•As a general rule, temperature of more than 38.3°C (101°F) warrants special attention in all patients.
•In immunocompromised patients, temperature of any degree should be investigated.
Step 2: Take a detailed history
•Take proper history from the bedside nurse and do a thorough chart review.
•Inquire about medications, blood transfusion, diarrhea, rash, new procedure, dressing changes, and line manipulation.
•Duration of indwelling urinary catheter and central line placement.
Step 3: Perform focused clinical examination
•Examine for any source of infection or noninfectious causes of fever (Tables 52.1 and 52.2).
•Perform systematic head-to-toe examination:
–Purulent nasal discharge, sinus tenderness
–Parotid swelling, oral hygiene
–Chest auscultation (including bases)
–New murmur
–Abdominal examination, suprapubic tenderness
–Vascular device sites for purulence and erythema, note insertion date
–Urinary catheter site
Table 52.1 Noninfectious causes of fever in the ICU
Drug fever
b-Lactam, antiepileptics, sulfonamides
Antipsychotics (neuroleptic malignant syndrome, serotonin syndrome)
Blood products, IV contrast, immunoglobulins, albumin
CNS causes: blood in cerebrospinal fluid, pontine bleed
Pulmonary/cardiac causes: acute respiratory distress syndrome, pulmonary emboli, fat emboli, pericarditis
Abdominal causes: ischemic gut, pancreatitis, acalculous cholecystitis
Metabolic: adrenal insufficiency, thyroid storm, gout
Postoperative fever (48 h), postprocedure (bronchoscopy)
Thrombophlebitis, decubitus ulcer, hematoma, deep venous thrombosis (DVT)
Table 52.2 Infectious causes of new-onset fever in the ICU
Ventilator-associated pneumonia
Sinusitis
Catheter-related sepsis
Urinary tract infection
Clostridium difficile diarrhea
Complicated wound infections
52 New-Onset Fever |
413 |
|
|
–Surgical wounds, drain sites (take off dressings)
–Skin rash
–Gynecological examination
–Painful leg swelling
–Decubitus ulcer
Step 4: Send investigations
•If clinical examination does not strongly suggest a noninfectious source, a pair of blood cultures should be sent in the following:
–In patients with temperature above 101°F
–In patients who are hemodynamically unstable or develop new organ dysfunction or immunosuppressed, with new onset of fever of any degree
•All ICUs should have a blood culture drawing protocol in consultation with microbiology department:
–Skin disinfection: 2% chlorhexidine or 2% iodine, give 30 s for drying.
–Site: two peripheral venepunctures, or one from distal lumen of the central line and another from periphery.
–Minimum two sets—20 mL in each—to be inoculated directly into the culture bottle.
–Labeling should be done carefully for site, date, and time.
•If infection is suspected clinically and there is a focus on infection, the following investigations should be sent:
–Total and differential white blood cell count, C-reactive protein (CRP), procalcitonin when presence of infection is in doubt.
–Focused imaging such as chest X-ray, abdominal ultrasonography, CT scan of the abdomen/chest.
–If there is a history of diarrhea, send stool for occult blood, pus cells,
Clostridium difficile toxin.
–Urinalysis and culture sensitivity.
–Transthoracic/transesophageal echocardiogram—look for vegetations.
–Sputum, endotracheal suction, bronchoscopy with bronchoalveolar lavage sent for Gram stain and quantitative bacterial culture and sensitivity.
•Trend of white blood cell count or CRP is valuable to ascertain any new infection.
Step 5: Remove lines if there is a suspicion of line sepsis
•All patients with a vascular access of some duration and persistent fever without any other obvious source of infection should have the line removed at the earliest if any of the following criteria are met:
–Inflammation or purulence present at the insertion site or along the tunnel
–No other identifiable source of infection
–An abrupt onset, associated with fulminant shock
–Nonfunctioning lumen
–Fever on starting infusion/dialysis
–Persistent bacteremia or fungemia
414 |
S. Todi and R. Chawla |
|
|
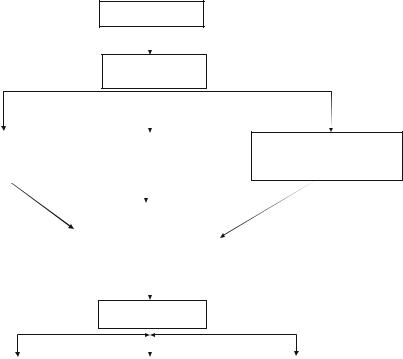
Confirm fever of >100°F
Focused clinical exam and chart review
If Source of infection |
|
If no obvious source of fever and |
|
suspected appropriate |
|
the patient has a central/arterial |
|
investigation and |
|
line placed for more than 2 days |
|
treatment (Table2) |
|
consider line sepsis |
|
|
|
|
|
|
|
|
|
|
Send blood cultures for fever>101°F |
|
|
|
or immunocompromised |
|
|
|
or hypotension |
|
|
|
or new organ dysfunction |
|
|
|
|
|
|
Look for noninfectious cause of fever (Table1)
Persistent fever on broadspectrum antibiotics
Fungemia—look for fungal |
|
Occult source of sepsis—chest |
|
Reconsider noninfectious |
colonization, send fungal |
|
CT, USG/CT abdomen, echo, |
|
source of fever (Table 1) |
culture |
|
bronchoscopy, repeat blood |
|
|
Start preemptive antifungal |
|
cultures, venous Doppler of legs |
|
|
therapy |
|
as indicated |
|
|
|
|
|
|
|
Fig. 52.1 An approach to new onset of fever in the ICU
•The intracutaneous and tip of the central line should be sent for semiquantitative culture.
•Central line infection is considered significant for the following situations:
–Culture of the same organism from both the catheter tips and at least one percutaneous blood culture
–Multiple blood cultures containing organisms that might otherwise be disregarded as contaminants such as Staphylococci (especially coagulase-negative
Staphylococci) and Candida
–Positive semiquantitative culture of the catheter tip (>15 cfu)
–Differential time to positivity—growth detected from the catheter sample at least 2 h before growth detected from the peripheral vein sample (Fig. 52.1)
Step 6: Make a diagnosis
•In patients on the ventilator, pneumonia should be considered by clinical examination, purulence of endotracheal secretions, raised white blood cell count, and new infiltrate on chest skiagram.
