
- •ICU Protocols
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1: Airway Management
- •Suggested Reading
- •2: Acute Respiratory Failure
- •Suggested Reading
- •Suggested Reading
- •Website
- •4: Basic Mechanical Ventilation
- •Suggested Reading
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Websites
- •7: Weaning
- •Suggested Reading
- •8: Massive Hemoptysis
- •Suggested Reading
- •9: Pulmonary Thromboembolism
- •Suggested Reading
- •Suggested Reading
- •Websites
- •11: Ventilator-Associated Pneumonia
- •Suggested Readings
- •12: Pleural Diseases
- •Suggested Reading
- •Websites
- •13: Sleep-Disordered Breathing
- •Suggested Reading
- •Websites
- •14: Oxygen Therapy
- •Suggested Reading
- •15: Pulse Oximetry and Capnography
- •Conclusion
- •Suggested Reading
- •Websites
- •16: Hemodynamic Monitoring
- •Suggested Reading
- •Websites
- •17: Echocardiography
- •Suggested Readings
- •Websites
- •Suggested Reading
- •Websites
- •19: Cardiorespiratory Arrest
- •Suggested Reading
- •Websites
- •20: Cardiogenic Shock
- •Suggested Reading
- •21: Acute Heart Failure
- •Suggested Reading
- •22: Cardiac Arrhythmias
- •Suggested Reading
- •Website
- •23: Acute Coronary Syndromes
- •Suggested Reading
- •Website
- •Suggested Reading
- •25: Aortic Dissection
- •Suggested Reading
- •26: Cerebrovascular Accident
- •Suggested Reading
- •Websites
- •27: Subarachnoid Hemorrhage
- •Suggested Reading
- •Websites
- •28: Status Epilepticus
- •Suggested Reading
- •29: Acute Flaccid Paralysis
- •Suggested Readings
- •30: Coma
- •Suggested Reading
- •Suggested Reading
- •Websites
- •32: Acute Febrile Encephalopathy
- •Suggested Reading
- •33: Sedation and Analgesia
- •Suggested Reading
- •Websites
- •34: Brain Death
- •Suggested Reading
- •Websites
- •35: Upper Gastrointestinal Bleeding
- •Suggested Reading
- •36: Lower Gastrointestinal Bleeding
- •Suggested Reading
- •37: Acute Diarrhea
- •Suggested Reading
- •38: Acute Abdominal Distension
- •Suggested Reading
- •39: Intra-abdominal Hypertension
- •Suggested Reading
- •Website
- •40: Acute Pancreatitis
- •Suggested Reading
- •Website
- •41: Acute Liver Failure
- •Suggested Reading
- •Suggested Reading
- •Websites
- •43: Nutrition Support
- •Suggested Reading
- •44: Acute Renal Failure
- •Suggested Reading
- •Websites
- •45: Renal Replacement Therapy
- •Suggested Reading
- •Website
- •46: Managing a Patient on Dialysis
- •Suggested Reading
- •Websites
- •47: Drug Dosing
- •Suggested Reading
- •Websites
- •48: General Measures of Infection Control
- •Suggested Reading
- •Websites
- •49: Antibiotic Stewardship
- •Suggested Reading
- •Website
- •50: Septic Shock
- •Suggested Reading
- •51: Severe Tropical Infections
- •Suggested Reading
- •Websites
- •52: New-Onset Fever
- •Suggested Reading
- •Websites
- •53: Fungal Infections
- •Suggested Reading
- •Suggested Reading
- •Website
- •55: Hyponatremia
- •Suggested Reading
- •56: Hypernatremia
- •Suggested Reading
- •57: Hypokalemia and Hyperkalemia
- •57.1 Hyperkalemia
- •Suggested Reading
- •Website
- •58: Arterial Blood Gases
- •Suggested Reading
- •Websites
- •59: Diabetic Emergencies
- •59.1 Hyperglycemic Emergencies
- •59.2 Hypoglycemia
- •Suggested Reading
- •60: Glycemic Control in the ICU
- •Suggested Reading
- •61: Transfusion Practices and Complications
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Website
- •63: Onco-emergencies
- •63.1 Hypercalcemia
- •63.2 ECG Changes in Hypercalcemia
- •63.3 Superior Vena Cava Syndrome
- •63.4 Malignant Spinal Cord Compression
- •Suggested Reading
- •64: General Management of Trauma
- •Suggested Reading
- •65: Severe Head and Spinal Cord Injury
- •Suggested Reading
- •Websites
- •66: Torso Trauma
- •Suggested Reading
- •Websites
- •67: Burn Management
- •Suggested Reading
- •68: General Poisoning Management
- •Suggested Reading
- •69: Syndromic Approach to Poisoning
- •Suggested Reading
- •Websites
- •70: Drug Abuse
- •Suggested Reading
- •71: Snakebite
- •Suggested Reading
- •72: Heat Stroke and Hypothermia
- •72.1 Heat Stroke
- •72.2 Hypothermia
- •Suggested Reading
- •73: Jaundice in Pregnancy
- •Suggested Reading
- •Suggested Reading
- •75: Severe Preeclampsia
- •Suggested Reading
- •76: General Issues in Perioperative Care
- •Suggested Reading
- •Web Site
- •77.1 Cardiac Surgery
- •77.2 Thoracic Surgery
- •77.3 Neurosurgery
- •Suggested Reading
- •78: Initial Assessment and Resuscitation
- •Suggested Reading
- •79: Comprehensive ICU Care
- •Suggested Reading
- •Website
- •80: Quality Control
- •Suggested Reading
- •Websites
- •81: Ethical Principles in End-of-Life Care
- •Suggested Reading
- •82: ICU Organization and Training
- •Suggested Reading
- •Website
- •83: Transportation of Critically Ill Patients
- •83.1 Intrahospital Transport
- •83.2 Interhospital Transport
- •Suggested Reading
- •84: Scoring Systems
- •Suggested Reading
- •Websites
- •85: Mechanical Ventilation
- •Suggested Reading
- •86: Acute Severe Asthma
- •Suggested Reading
- •87: Status Epilepticus
- •Suggested Reading
- •88: Severe Sepsis and Septic Shock
- •Suggested Reading
- •89: Acute Intracranial Hypertension
- •Suggested Reading
- •90: Multiorgan Failure
- •90.1 Concurrent Management of Hepatic Dysfunction
- •Suggested Readings
- •91: Central Line Placement
- •Suggested Reading
- •92: Arterial Catheterization
- •Suggested Reading
- •93: Pulmonary Artery Catheterization
- •Suggested Reading
- •Website
- •Suggested Reading
- •95: Temporary Pacemaker Insertion
- •Suggested Reading
- •96: Percutaneous Tracheostomy
- •Suggested Reading
- •97: Thoracentesis
- •Suggested Reading
- •98: Chest Tube Placement
- •Suggested Reading
- •99: Pericardiocentesis
- •Suggested Reading
- •100: Lumbar Puncture
- •Suggested Reading
- •Website
- •101: Intra-aortic Balloon Pump
- •Suggested Reading
- •Appendices
- •Appendix A
- •Appendix B
- •Common ICU Formulae
- •Appendix C
- •Appendix D: Syllabus for ICU Training
- •Index

Heat Stroke and Hypothermia |
72 |
|
|
Jagdish Dureja and Harpreet Singh |
|
72.1Heat Stroke
It was the month of July; a 55-year-old male laborer became unconscious at work. On examination, he was found to be obtunded with minimal response to painful stimulus. His skin was hot and flushed. He was tachypneic, tachycardiac, hypotensive, and hyperthermic (core temperature 107°F).
Normal temperature is a balance between heat production and dissipation. High fever can have serious consequences such as renal failure, disseminated intravascular coagulation, and death. Prompt and appropriate management can improve the outcome in these patients.
Step 1: Initiate resuscitation
•These patients should be resuscitated as mentioned in Chap. 78.
•Administer IV fluids promptly as these patients are dehydrated. The type and amount of fluid should be guided by volume status, electrolytes, and cardiac functions.
Step 2: Assess the type of hyperthermia by history and examination
•Hyperthermia is a core temperature greater than 104°F. The most common causes are heat stroke and adverse reactions to drugs.
J. Dureja, M.D., F.N.B. (*)
Department of Anaesthesia, BPS Mahilla Medical College, Khanpur, Sonipat, India e-mail: drdureja@gmail.com
H. Singh, M.D.
Department of Medicine, Pt. B.D. Sharma Post Graduate Institute of Medical Sciences, Rohtak, India
R. Chawla and S. Todi (eds.), ICU Protocols: A stepwise approach, |
573 |
DOI 10.1007/978-81-322-0535-7_72, © Springer India 2012 |
|
574 |
J. Dureja and H. Singh |
|
|
Heat stroke is caused commonly by prolonged exposure to excessive heat:
•Exertional heat stroke occurs in young, healthy individuals engaged in heavy exercise during periods of high ambient temperature and humidity.
•Nonexertional heat stroke is precipitated by various conditions. Vasodilation, sweating, and other heat-loss mechanisms are reduced by medications, such as anticholinergic drugs, antihistaminics, and diuretics, antipsychotics (e.g., MAO inhibitors and tricyclic antidepressants), neuroleptic agents, and illicit drugs (amphetamines, cocaine, LSD, MDMA), brain hemorrhage, status epilepticus, and damage to the hypothalamus can also cause hyperthermia. Thyrotoxicosis and pheochromocytoma cause hyperthermia by increased heat production. Malignant hyperthermia is a rare complication of general anesthetics such as succinylcholine and halothane.
•A patient with heat stroke usually has a body temperature above 104°F.
•A high core temperature with appropriate history (e.g., environmental heat exposure, anticholinergics, neuroleptics, tricyclic antidepressants, succinylcholine, and halothane) is needed to diagnose heat stroke.
•Signs and symptoms include altered mentation or seizures, possible hallucinations, delirium, dry skin, rapid pulse, tachypnea, rales due to noncardiogenic pulmonary edema, pupil dilation, muscle rigidity, hypotension, arrhythmias, rhabdomyolysis, dyselectrolytemia, and coma. Disseminated intravascular coagulation and mixed acidosis can accompany the elevated temperature.
•Malignant hyperthermia: This should be suspected if there is sudden rise of EtCo2 in a patient undergoing surgery under general anesthesia.
Step 3: Send investigations
•Hemogram
•Creatine phosphokinase—elevated levels suggest hyperthermia.
•Renal functions
•Urine for myoglobin
•When indicated, coagulation studies, toxicologic screening, CT head, and lumbar puncture should be carried out.
•Diagnosis of malignant hyperthermia is confirmed by in vitro muscle contracture test.
Step 4: General management
•Ask the patient to rest, preferably in a cool place.
•If the patient is conscious, offer fluids but avoid alcohol and caffeine.
•Confirm the diagnosis with a calibrated thermometer to measure high temperature (40–47°C).
•Encourage him/her to shower and bath, or sponge off with cool water.
•There is no role of antipyretics (acetaminophen/acetylsalicylic acid).
•Monitor core temperature continuously with a rectal or esophageal probe.
•In order to avoid iatrogenic hypothermia, stop cooling at 39.5°C (103°F).
72 Heat Stroke and Hypothermia |
575 |
|
|
•Cooling measures: The biggest predictor of outcome is the degree and duration of hyperthermia.
External cooling techniques are easier to implement and are effective, welltolerated, and include the following:
–Conductive cooling—direct application of sources such as hypothermic blanket, ice bath, or ice packs to neck, axillae, and groins. Ice packs are effective but poorly tolerated by the awake patient. Avoid vasoconstriction and shivering as vasoconstriction impedes the heat loss and shivering creates heat.
–Convective techniques include removal of clothing and use of fans and air conditioners.
–Evaporative cooling can be accelerated by removing clothing and using a fan in conjunction with misting the skin with tepid water or applying a singlelayer wet sheet to bare skin. Shivering may be suppressed with IV benzodiazepines such as diazepam (5 mg) or lorazepam (1–2 mg).
•Immersing the patient in ice water is the most effective method of rapid cooling but complicates monitoring and access to the patient.
•Internal cooling techniques such as ice water gastric or rectal lavage, thoracic lavage, and extracorporeal blood cooling are effective, but they are difficult to manage and are associated with complications. Cold peritoneal lavage results in rapid cooling but is an invasive technique contraindicated in pregnant patients or those with previous abdominal surgery.
•Cold O2 and cold IV fluids are useful adjuncts.
Step 5: Specific management: Malignant hyperthermia and neuroleptic malignant syndrome
•Dantrolene, a nonspecific skeletal muscle relaxant, is the mainstay of treatment. It acts by blocking the release of calcium from the sarcoplasmic reticulum, thereby decreasing the myoplasmic concentration of free calcium, and diminishes the myocyte hypermetabolism that causes the symptoms.
•It is most effective if given early in the illness, when maximal calcium can be retained within the sarcoplasmic reticulum.
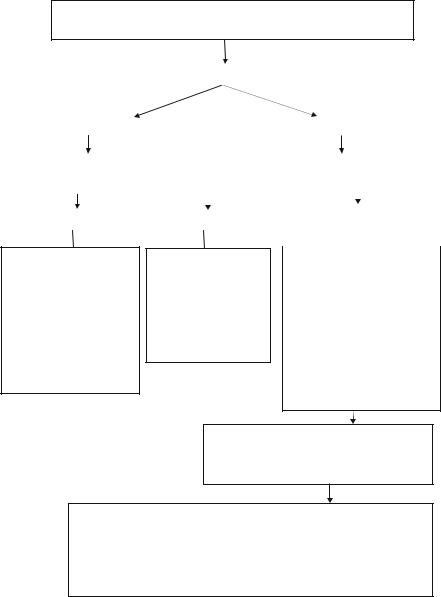
•There is associated risk of hepatotoxicity with dantrolene, so it should be avoided if liver function tests are abnormal (see Fig. 72.1 for detail).
Step 6: Manage complications
•Rhabdomyolysis
–Expand the intravascular volume with normal saline and administer mannitol and sodium bicarbonate.
–Alkalinization of urine prevents the precipitation of myoglobin in the renal tubules.
–The goal is to prevent myoglobin-induced renal injury by promoting renal blood flow, diuresis, and urinary alkalinization. Monitor serum electrolytes to prevent life-threatening arrhythmias.
576 |
J. Dureja and H. Singh |
|
|
•Get the victim out of the sun to a cool place, preferably one that is air-conditioned
•Discontinue the presumed causative agent (neuroleptics/suxamethonium/halothane)
•Give IV diazepam 5 mg IV if the patient is having seizures
|
|
|
|
|
Assess breathing and pulse |
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
Pulse and breathing present |
|
|
|
|
|
|
|
Pulse or breathing absent |
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
O2 inhalation |
|
|
|
|
|
|
|
|
ACLS CPR protocol |
|
|
|||
|
|
Cold IV fluids |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Measure core temperature |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Neuroleptic malignant syndrome |
|
|
|
Heat stroke |
|
|
|
|
Malignant hyperthermia |
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1.Discontinue the neuroleptic
2.Bromocriptine—2.5 mg PO
every 6–8 hours titrated up to a maximum dose of 40 mg/day.
To be continued for 10 days after NMS is controlled and then taper.
OR
Amantadine—100 mg/day PO and is titrated to a maximum dose of 200 mg every 12 hours OR Dantrolene 1-3 mg/kg IV initially, maximum dose is
10 mg/kg/d
1.Get the victim out of the hot area
2.Loosen the garments
3.Give cold IV saline
4.Give high flowhumidified oxygen
5.Do external cooling and avoid vasoconstriction
6.Do internal cooling
7.Treat complications
1.Remove the trigger drugs
2.Turn off the vaporisers
3.Use high fresh gas flows (O2)
4.Use new, nonrebreathing circuit
5.Hyperventilate
6.Maintain anaesthesia with IV agents
7.Dantrolene: 2 mg/kg IV initially and repeated every 5 minutes until symptoms abate up, maximum dose 10 mg/kg, followed by 4-8 mg/kg per day, P.O. in four divided doses x 3 days
8.Use active body cooling but avoid vasoconstriction. Give cold IV fluids, cold peritoneal lavage and extracorporeal heat exchanges.
ICU management
Continue monitoring and symptomatic treatment Assess for renal failure and compartment syndrome Give further dantrolene as necessary
Consider other diagnoses,e.g., sepsis, phaeochromocytoma
Treat complications
Hypoxemia and acidosis: 100% O2, hyperventilate, sodium bicarbonate Hyperkalaemia: sodium bicarbonate, glucose and insulin, calcium chloride
Myoglobinaemia: forced alkaline diuresis (keep urine output >3 mL/kg/h, urine pH >7.0) Disseminated intravascular coagulation: fresh frozen plasma, cryoprecipitate, platelets Cardiac arrhythmias: procainamide, magnesium,and amiodarone (Avoid calcium channel blockers—interaction with dantrolene)
Refer the patient and family to MH testing center for contracture or DNA testing
Fig. 72.1 Management of hyperthermia
