
- •ICU Protocols
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1: Airway Management
- •Suggested Reading
- •2: Acute Respiratory Failure
- •Suggested Reading
- •Suggested Reading
- •Website
- •4: Basic Mechanical Ventilation
- •Suggested Reading
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Websites
- •7: Weaning
- •Suggested Reading
- •8: Massive Hemoptysis
- •Suggested Reading
- •9: Pulmonary Thromboembolism
- •Suggested Reading
- •Suggested Reading
- •Websites
- •11: Ventilator-Associated Pneumonia
- •Suggested Readings
- •12: Pleural Diseases
- •Suggested Reading
- •Websites
- •13: Sleep-Disordered Breathing
- •Suggested Reading
- •Websites
- •14: Oxygen Therapy
- •Suggested Reading
- •15: Pulse Oximetry and Capnography
- •Conclusion
- •Suggested Reading
- •Websites
- •16: Hemodynamic Monitoring
- •Suggested Reading
- •Websites
- •17: Echocardiography
- •Suggested Readings
- •Websites
- •Suggested Reading
- •Websites
- •19: Cardiorespiratory Arrest
- •Suggested Reading
- •Websites
- •20: Cardiogenic Shock
- •Suggested Reading
- •21: Acute Heart Failure
- •Suggested Reading
- •22: Cardiac Arrhythmias
- •Suggested Reading
- •Website
- •23: Acute Coronary Syndromes
- •Suggested Reading
- •Website
- •Suggested Reading
- •25: Aortic Dissection
- •Suggested Reading
- •26: Cerebrovascular Accident
- •Suggested Reading
- •Websites
- •27: Subarachnoid Hemorrhage
- •Suggested Reading
- •Websites
- •28: Status Epilepticus
- •Suggested Reading
- •29: Acute Flaccid Paralysis
- •Suggested Readings
- •30: Coma
- •Suggested Reading
- •Suggested Reading
- •Websites
- •32: Acute Febrile Encephalopathy
- •Suggested Reading
- •33: Sedation and Analgesia
- •Suggested Reading
- •Websites
- •34: Brain Death
- •Suggested Reading
- •Websites
- •35: Upper Gastrointestinal Bleeding
- •Suggested Reading
- •36: Lower Gastrointestinal Bleeding
- •Suggested Reading
- •37: Acute Diarrhea
- •Suggested Reading
- •38: Acute Abdominal Distension
- •Suggested Reading
- •39: Intra-abdominal Hypertension
- •Suggested Reading
- •Website
- •40: Acute Pancreatitis
- •Suggested Reading
- •Website
- •41: Acute Liver Failure
- •Suggested Reading
- •Suggested Reading
- •Websites
- •43: Nutrition Support
- •Suggested Reading
- •44: Acute Renal Failure
- •Suggested Reading
- •Websites
- •45: Renal Replacement Therapy
- •Suggested Reading
- •Website
- •46: Managing a Patient on Dialysis
- •Suggested Reading
- •Websites
- •47: Drug Dosing
- •Suggested Reading
- •Websites
- •48: General Measures of Infection Control
- •Suggested Reading
- •Websites
- •49: Antibiotic Stewardship
- •Suggested Reading
- •Website
- •50: Septic Shock
- •Suggested Reading
- •51: Severe Tropical Infections
- •Suggested Reading
- •Websites
- •52: New-Onset Fever
- •Suggested Reading
- •Websites
- •53: Fungal Infections
- •Suggested Reading
- •Suggested Reading
- •Website
- •55: Hyponatremia
- •Suggested Reading
- •56: Hypernatremia
- •Suggested Reading
- •57: Hypokalemia and Hyperkalemia
- •57.1 Hyperkalemia
- •Suggested Reading
- •Website
- •58: Arterial Blood Gases
- •Suggested Reading
- •Websites
- •59: Diabetic Emergencies
- •59.1 Hyperglycemic Emergencies
- •59.2 Hypoglycemia
- •Suggested Reading
- •60: Glycemic Control in the ICU
- •Suggested Reading
- •61: Transfusion Practices and Complications
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Website
- •63: Onco-emergencies
- •63.1 Hypercalcemia
- •63.2 ECG Changes in Hypercalcemia
- •63.3 Superior Vena Cava Syndrome
- •63.4 Malignant Spinal Cord Compression
- •Suggested Reading
- •64: General Management of Trauma
- •Suggested Reading
- •65: Severe Head and Spinal Cord Injury
- •Suggested Reading
- •Websites
- •66: Torso Trauma
- •Suggested Reading
- •Websites
- •67: Burn Management
- •Suggested Reading
- •68: General Poisoning Management
- •Suggested Reading
- •69: Syndromic Approach to Poisoning
- •Suggested Reading
- •Websites
- •70: Drug Abuse
- •Suggested Reading
- •71: Snakebite
- •Suggested Reading
- •72: Heat Stroke and Hypothermia
- •72.1 Heat Stroke
- •72.2 Hypothermia
- •Suggested Reading
- •73: Jaundice in Pregnancy
- •Suggested Reading
- •Suggested Reading
- •75: Severe Preeclampsia
- •Suggested Reading
- •76: General Issues in Perioperative Care
- •Suggested Reading
- •Web Site
- •77.1 Cardiac Surgery
- •77.2 Thoracic Surgery
- •77.3 Neurosurgery
- •Suggested Reading
- •78: Initial Assessment and Resuscitation
- •Suggested Reading
- •79: Comprehensive ICU Care
- •Suggested Reading
- •Website
- •80: Quality Control
- •Suggested Reading
- •Websites
- •81: Ethical Principles in End-of-Life Care
- •Suggested Reading
- •82: ICU Organization and Training
- •Suggested Reading
- •Website
- •83: Transportation of Critically Ill Patients
- •83.1 Intrahospital Transport
- •83.2 Interhospital Transport
- •Suggested Reading
- •84: Scoring Systems
- •Suggested Reading
- •Websites
- •85: Mechanical Ventilation
- •Suggested Reading
- •86: Acute Severe Asthma
- •Suggested Reading
- •87: Status Epilepticus
- •Suggested Reading
- •88: Severe Sepsis and Septic Shock
- •Suggested Reading
- •89: Acute Intracranial Hypertension
- •Suggested Reading
- •90: Multiorgan Failure
- •90.1 Concurrent Management of Hepatic Dysfunction
- •Suggested Readings
- •91: Central Line Placement
- •Suggested Reading
- •92: Arterial Catheterization
- •Suggested Reading
- •93: Pulmonary Artery Catheterization
- •Suggested Reading
- •Website
- •Suggested Reading
- •95: Temporary Pacemaker Insertion
- •Suggested Reading
- •96: Percutaneous Tracheostomy
- •Suggested Reading
- •97: Thoracentesis
- •Suggested Reading
- •98: Chest Tube Placement
- •Suggested Reading
- •99: Pericardiocentesis
- •Suggested Reading
- •100: Lumbar Puncture
- •Suggested Reading
- •Website
- •101: Intra-aortic Balloon Pump
- •Suggested Reading
- •Appendices
- •Appendix A
- •Appendix B
- •Common ICU Formulae
- •Appendix C
- •Appendix D: Syllabus for ICU Training
- •Index
Percutaneous Tracheostomy |
96 |
|
|
Rajesh Chawla and Munish Chauhan |
|
A 50-year-old male patient, a known case of chronic obstructive pulmonary disease with ischemic cardiomyopathy and renal failure, was admitted to hospital with acute breathlessness. He was drowsy and unable to maintain oxygenation on noninvasive ventilation. He was put on invasive ventilation and he got better. Spontaneous breathing trial was tried a number of times, but he could not be weaned off the ventilator for 10 days. Percutaneous tracheostomy (PCT) was planned.
PCT is a bedside procedure performed usually in an ICU setting. This uses Seldinger technique and is associated with lesser postoperative complications.
Step 1: Assess the need for tracheostomy and advantage of PCT
A.Indications
•Securing the airway
–Temporary—to aid weaning after long-term mechanical ventilation
–Permanent—airway protection in neurological patients
•Tracheal toileting and airway protection
–In the patient with excess or thick secretions who is not able to expectorate
–Generalized weakness—neuromuscular disease or central cause
–Altered mentation—unable to maintain airways
R. Chawla, M.D., F.C.C.M. (*)
Department of Respiratory, Critical Care & Sleep Medicine, Indraprastha Apollo Hospitals, New Delhi, India
e-mail: drchawla@hotmail.com
M. Chauhan, M.D.
Department of Respiratory & Critical Care Medicine, Indraprastha Apollo Hospitals, New Delhi, India
R. Chawla and S. Todi (eds.), ICU Protocols: A stepwise approach, |
767 |
DOI 10.1007/978-81-322-0535-7_96, © Springer India 2012 |
|
768 |
R. Chawla and M. Chauhan |
|
|
•Relief of nonemergent upper airway obstruction
–Once initial airway stabilization has been done via translaryngeal intubation/emergency cricothyroidotomy
B.Advantages of PCT over surgical tracheostomy
•Blunt dilatation causes less tissue trauma and devitalization than sharp dissection.
•It may lead to lower rates of hemorrhage, stomatitis, and cosmetic deformity.
•The tracheostomy tube is fitted tightly against the stoma.
•Interval between decision and actual procedure is shorter.
•It can be done at the bedside in the ICU, avoiding a potentially hazardous transfer of critically ill patients to the operating room.
•Savings in cost of operating room personnel and equipment can be achieved.
Step 2: Select patient for PCT
•The patient should be hemodynamically stable as much as possible.
•FiO2 should be below 0.6
•Positive end-expiratory pressure should be less than 10 cm H2O.
•History of uncomplicated translaryngeal intubation is obtained.
•Cricoid cartilage is palpable at least 3 cm above the sternal angle during appropriate neck extension.
Step 3: Check for the contraindications
There are no absolute contraindications. Suggested contraindications are not supported by adequate data but are decided on merit depending on the operator experience and protocols of the center involved (Table 96.1).
Table 96.1 Contraindications to PCT
Inability to identify anatomical landmarks |
Surgical skin site infection |
Previous major neck surgery completely obscuring |
Midline neck mass |
the anatomy |
|
Emergency airway control |
High positive end-expiratory pressure |
|
(>10–20 cm H2O) |
Repeat tracheostomy |
Severe coagulopathy |
Age less than 15 years |
Tracheomalacia |
Cervical fixation/injury/fracture |
Obese/thick neck |
Step 4: Decide timing
•The decision about tracheostomy requires anticipation of the duration of expected mechanical ventilation and the expected benefits and risks of the procedure.
•Time of PCT could be 7–14 days of intubation or less than 7 days for anticipated prolonged ventilation.
96 Percutaneous Tracheostomy |
769 |
|
|
Step 5: Obtain informed consent
•Discuss the prognosis of the patient and the need for the procedure.
•Explain the advantages and disadvantages of the procedure and the available options in detail. Communicate with the patients or their surrogates.
•Explain the detailed procedure, the benefits, the risks, and the alternatives in the language they understand.
•Document the consent and get it signed.
•In case of emergency, when the patient is unconscious and the surrogates are not available, document the situation clearly and perform the procedure.
Step 6: Form your team
•The operating physician.
•One physician, managing the upper airway and bronchoscope, manipulates the tube to allow PCT.
•The paramedical staff/technician who assists with the bronchoscope and handling of the endotracheal tube.
•Another paramedical staff monitoring the vitals and administering medication.
Step 7: Prepare for the procedure
•A PCT set as per the type decided by the physician
•A bronchoscope and its attachments
•Continuous monitoring of ECG, blood pressure, and oximetry
•Functioning intravenous access
•A sterile setup with enough sterile linen and instruments
•A crash cart with a laryngoscope and endotracheal tubes and emergency drugs
•Suction equipment
•Medications
–1% Xylocaine with epinephrine
–Sedating and paralyzing agents
Step 8: Identify anatomy (Fig. 96.1)
•Tracheostomy is carried out at least one to two rings beyond the cricoid.
•The tracheostomy tube is entered between the second and third cartilage rings or between the third and fourth cartilage rings.
•In a too high tracheostomy (close to cricoid), there is a risk of a subglottic stenosis.
•In a too low tracheotomy, there is a risk of bleeding from the brachiocephalic trunk.
Step 9: Perform percutaneous tracheostomy
•Ciaglia method (Blue Rhino PCT kit—Cook Critical Care Inc, Bloomington, IN)
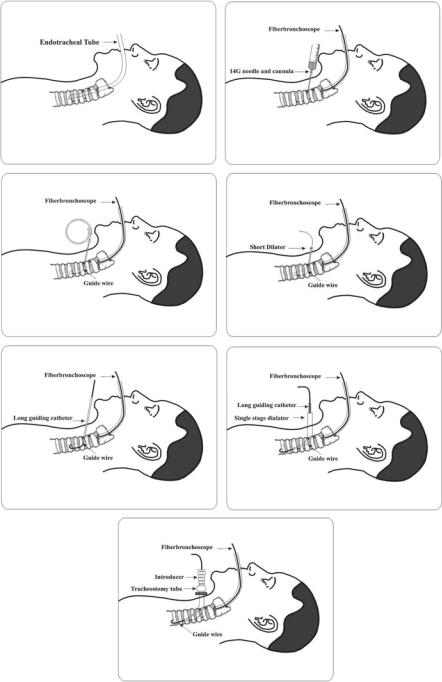
(Figs. 96.2, 96.3, 96.4, 96.5, 96.6, 96.7, and 96.8)
1. Continuously monitor vital signs, pulse oximetry, and complete ventilatory parameters.
2. Ventilate with 100% oxygen during the procedure.

770 |
R. Chawla and M. Chauhan |
|
|
Fig. 96.1 Tracheal anatomy
3. Counsel and comfort the patient if he/she is conscious. 4. Sedate and paralyze the patient before positioning.
5. Extend the neck to open the tracheal interspaces, carefully supporting the vertex using a sand bag beneath the shoulders and the head ring.
6. Prepare the surgical field with alcohol-containing solution and drape it.
7. Verify the anatomy and identify the neck structures and landmarks. A preprocedure ultrasound may be done if anatomy is not clear (e.g., morbid obesity).
8. The local anesthetic with epinephrine is infiltrated into the surgical site.
9. Check all parts of the tracheostomy set. Check the tracheostomy balloon by inflating and collapsing it.
10. Make a transverse skin incision approximately 2 cm over the first and second tracheal interspace, approximately two fingers’ breadth above the sternal notch.
11. Dissect the wound bluntly with a hemostat through the subcutaneous fascia.
12. Withdraw the endotracheal tube into a position above the first tracheal interspace under bronchoscopic guidance.
13. Insert a 14-gauge cannula over the needle through the skin incision between either the first and second or the second and third tracheal rings under bronchoscopic guidance, aspirating for air (Fig. 96.3).
14. Withdraw the needle leaving the cannula in place.
15. Advance a J-tipped guidewire through the cannula toward the carina and withdraw the cannula (Fig. 96.4).
16. Dilate the opening using a small dilator (Fig. 96.5).
17. Insert a stiffer guide cannula over the guidewire after withdrawing the cannula (Fig. 96.6).
96 Percutaneous Tracheostomy |
771 |
|
|
Figs. 96.2, 96.3, 96.4, 96.5, 96.6, 96.7, and 96.8 Ciaglia method
772 |
R. Chawla and M. Chauhan |
|
|
18. Use a single, sharply tapered dilator with a hydrophilic coating and dipped in water-based jelly, for complete dilatation in one step (Fig. 96.7).
19. Withdraw the dilator leaving the guidewire and the stiff white guide cannula assembly in place.
20. Once the tracheostoma has been dilated to the appropriate size, a tracheostomy tube is introduced into the trachea over the same guidewire using introducer dilators as an obturator (Fig. 96.8).
21. The guidewire assembly is removed leaving the tracheostomy tube in place.
22. Position is confirmed by bronchoscopic visualization.
23. The tube is sutured to the skin and also fixed with the provided thread around the neck.
•Griggs guidewire dilating forceps
–Steps 1–15 as above.
–The cannula is removed leaving the guidewire in place.
–The Griggs guidewire dilating forceps are threaded over the guidewire into the soft tissue.
–Open the forceps “dilating” the soft tissue and advance the forceps into the trachea.
–The trachea is dilated to an aperture sufficient enough to accommodate the tracheotomy tube.
–An obturator is used to insert the tube over the guidewire.
–The rest of the steps of fixation of the tube are same as above (Fig. 96.3).
•PercuTwist technique. (It contains a J-tipped guidewire, a scalpel, a large-bore introducer needle, the hydrophilically coated PercuTwist dilator, a specially designed 9.0-mm internal diameter PercuTwist tracheotomy cannula, and an insertion dilator.)
–Steps 1–15 as above.
–The PercuTwist single dilator is moistened to activate the hydrophilic coating.
–Advance it over the guidewire into the soft tissue using a clockwise rotation.
–Further rotation of the device engages the anterior tracheal wall and enlarges the aperture.
–Once dilated adequately, the device is removed and replaced with the 9.0-mm tracheotomy tube fitted with the insertion dilator.
Step 10: Postoperative care of the tracheostomy tube
•Wound and dressing care
–Daily examination of the stoma is needed to identify infections or excoriations of the skin.
–Keep the wound clean and free of blood and secretions, especially in the immediate posttracheostomy period.
96 Percutaneous Tracheostomy |
773 |
|
|
–Dressing changes should be performed at least twice a day and when the dressings are soiled.
–When changing dressings and tapes, special care is needed to avoid accidental dislodgement of the tracheostomy tube.
–The inner cannula if used is changed daily or more frequently if necessary.
•Humidification
–Humidification of inspired gases prevents obstruction of the tube by inspissated secretions and maintains mucociliary clearance and cough reflex.
–Heat and moisture exchangers are preferred over heated humidifiers.
•Suctioning
–Airways should be cleared of excess secretions to decrease the risk of lung infection and airway plugging.
–Suctioning is frequently required in patients with poor or ineffective cough.
–Suctioning should remove the maximal amount of secretions and cause the least amount of airway trauma. Thus, practice slow suctioning.
1. Routine suctioning, however, is not recommended.
2. Upper airway suctioning should also be done periodically to remove oral secretions and to minimize stasis of pooled secretions above the tracheotomy cuff with subsequent potential aspiration into the lower airways.
•Change tracheostomy tube
–In case of a functional problem with the tube, such as an air leak.
–If the lumen is narrowed due to the buildup of dried secretions.
–Switching to a new type of the tube.
–May downsize the tube prior to decannulation.
–Do not change the outer cannula, unless the cuff is damaged, in the initial 5–7 days as the tract is not stable.
•Tube cuff pressure
–Tracheotomy tube cuffs require monitoring to maintain pressures in a range of 20–25 mmHg.
–Cuff pressures should be monitored with calibrated devices.
–Record at least once every nursing shift and after manipulation of the tracheotomy tubes.
–Maintain the tube in a central position, avoiding angling and contact between tracheal mucosa and the tube to avoid damage by the distal end.
–Avoid traction as well as unnecessary movement of the tube.
•Nutrition
–Feeding may become complicated because of tube interference with normal swallowing and airway control.
–It decreases laryngeal elevation during swallowing and an inflated cuff may compress the esophagus. So it may deflate a little.
–Keep the head end elevated to 45° during periods of tube feeding.
–Before attempting oral feedings, several objective criteria must be met.
•The patient must be consistently alert and able to follow complex commands.
774 |
R. Chawla and M. Chauhan |
|
|
•Adequate cough and swallowing reflexes.
•Adequate oral motor strength.
•A significant respiratory reserve.
•Assess swallowing function.
•Oral feeding is done under supervision of a caregiver and carefully assessed for aspiration or regurgitation.
Step 11: Manage complications
•Early complications (until 7 days)
1.Tube displacement
•Management—endotracheal intubation to establish airway. Replace the tracheostomy tube under less urgent conditions, always under fiber-optic guidance as there is a danger of entering a false tract. If it fails, intubate orally.
•Prevention— proper placement of the stoma, avoid excessive neck hyperextension and/or tracheal traction, apply sufficiently tight tracheostomy tube retention tapes, and suture tracheostomy tube flange to the skin.
•Displacements after 7 days are managed by simply replacing the tube as the tract is well formed.
2.Tube obstruction
•By mucus, blood clots, displacement into surrounding soft tissues, or abutment of the tube’s open tip against the tracheal wall.
•Reposition or suction thoroughly; deflate cuff as a temporizing measure.
•If it fails, replace the tube immediately or intubate orally.
3.Pneumothorax/pneumomediastinum
•Pleura can be damaged during tracheostomy.
•The incidence of pneumothorax after tracheostomy ranges from 0% to 5%.
•Many surgeons routinely obtain a postoperative chest radiograph though optional.
•Immediate tube thoracostomy.
4.Subcutaneous emphysema
•Positive-pressure ventilation or coughing against a tightly sutured or packed wound causes this.
•It can be prevented by not suturing the wound around the tube.
•It resolves spontaneously within a few days.
•A chest radiograph should be done to rule out a pneumothorax.
5.Hemorrhage
•Usually, minor postoperative venous ooze is the most common complication.
•Elevate the head of the bed, pack the wound, and/or use homeostatic materials.
•Major bleeding can occur in up to 5% of tracheotomies.
–Hemorrhage from the isthmus of the thyroid gland
–Injury to the transverse jugular vein
–May require an exploration
96 Percutaneous Tracheostomy |
775 |
|
|
6.Stomal infections
•Good stoma care
•Early use of antibiotics but do not use prophylactic antibiotics
7.Others
•Arrhythmia
•Hypotension
•Hypoxia/hypercapnia
•Loss of airway control
•Bacteremia
•Esophageal injury
•Cardiorespiratory arrest
•Tracheolaryngeal injury
•Late complications (>7 days)
1.Tracheoinnominate artery fistula (<0.7% cases)
•Occurs due to erosion through the trachea into the artery due to excessive cuff pressure or by angulation of the tube tip against the anterior trachea
•Risk increased by the following:
–Low placement of tracheotomy
–High-pressure cuffs
–Excessive head or tracheostomy tube movement
–Malnourishment
•Management
–Evaluate even minor bleeds
–Hyperinflation of the cuff; lower neck incision with blind digital compression on the artery may be attempted in a resuscitative effort
–Operative intervention
2.Dysphagia and aspiration
•Due to causes discussed under “nutrition”
3.Tracheal stenosis
•Approximately 1–2% cases
•Caused by
–Ischemia
–Devascularization
–Chemical erosion
–Infection
•Due to high-pressure cuffs
•Forced angulation of a stiff tube
•Hyperinflation of the cuff which results in tracheal damage
•Site of stenosis may occur at the:
–Stoma
–Cuff
–Tip of the tracheotomy tube
4.Tracheoesophageal fistula
•Less than 1% of patients
•Mostly iatrogenic during procedure
776 |
R. Chawla and M. Chauhan |
|
|
•Erosion by the tracheotomy cuff
•Tube angulation with pressure against the posterior tracheal wall
•More common with a nasogastric tube in place as well
•Suspect if:
–Cuff leaks
–Abdominal distention
–Recurrent aspiration pneumonia
–Reflux of gastric fluids through the tracheostomy site
•Diagnosed by endoscopy or contrast studies
•Requires surgery or esophageal and tracheal stent
5.Granuloma formation
•A foreign body reaction to the tracheotomy tube or part.
•Treated with the YAG laser.
•Granulomas at the lower end of the tracheotomy tube require bronchoscopic removal providing temporary relief.
6.Persistent tracheocutaneous stoma
•Can occur when tube has been left in position for a prolonged period.
•Surgical closure is required.
7.Tracheomalacia
•Weakening of the tracheal wall
–Ischemic injury to the trachea
–Followed by chondritis
–Then destruction and necrosis of the tracheal cartilage
•Collapse of the affected portion of the trachea with expiration
–Airflow limitation
–Air trapping
–Retention of airway secretions
•Cause of weaning failure from mechanical ventilation.
•A short-term therapeutic approach to tracheomalacia is to place a longer tracheostomy tube to bypass the area of malacia.
•Long-term treatment options include stenting, tracheal resection, or tracheoplasty.
Step 12: Decannulation
1.Criteria
•Stable arterial blood gases
•Absence of distress
•Hemodynamic stability
•Absence of fever or active infection
•PaCO2 < 60 mmHg
•Absence of delirium or psychiatric disorder
•Normal endoscopic examination or revealing stenotic lesion occupying less than 30% of the airway
•Adequate swallowing
•Able to expectorate
