
- •ICU Protocols
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1: Airway Management
- •Suggested Reading
- •2: Acute Respiratory Failure
- •Suggested Reading
- •Suggested Reading
- •Website
- •4: Basic Mechanical Ventilation
- •Suggested Reading
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Websites
- •7: Weaning
- •Suggested Reading
- •8: Massive Hemoptysis
- •Suggested Reading
- •9: Pulmonary Thromboembolism
- •Suggested Reading
- •Suggested Reading
- •Websites
- •11: Ventilator-Associated Pneumonia
- •Suggested Readings
- •12: Pleural Diseases
- •Suggested Reading
- •Websites
- •13: Sleep-Disordered Breathing
- •Suggested Reading
- •Websites
- •14: Oxygen Therapy
- •Suggested Reading
- •15: Pulse Oximetry and Capnography
- •Conclusion
- •Suggested Reading
- •Websites
- •16: Hemodynamic Monitoring
- •Suggested Reading
- •Websites
- •17: Echocardiography
- •Suggested Readings
- •Websites
- •Suggested Reading
- •Websites
- •19: Cardiorespiratory Arrest
- •Suggested Reading
- •Websites
- •20: Cardiogenic Shock
- •Suggested Reading
- •21: Acute Heart Failure
- •Suggested Reading
- •22: Cardiac Arrhythmias
- •Suggested Reading
- •Website
- •23: Acute Coronary Syndromes
- •Suggested Reading
- •Website
- •Suggested Reading
- •25: Aortic Dissection
- •Suggested Reading
- •26: Cerebrovascular Accident
- •Suggested Reading
- •Websites
- •27: Subarachnoid Hemorrhage
- •Suggested Reading
- •Websites
- •28: Status Epilepticus
- •Suggested Reading
- •29: Acute Flaccid Paralysis
- •Suggested Readings
- •30: Coma
- •Suggested Reading
- •Suggested Reading
- •Websites
- •32: Acute Febrile Encephalopathy
- •Suggested Reading
- •33: Sedation and Analgesia
- •Suggested Reading
- •Websites
- •34: Brain Death
- •Suggested Reading
- •Websites
- •35: Upper Gastrointestinal Bleeding
- •Suggested Reading
- •36: Lower Gastrointestinal Bleeding
- •Suggested Reading
- •37: Acute Diarrhea
- •Suggested Reading
- •38: Acute Abdominal Distension
- •Suggested Reading
- •39: Intra-abdominal Hypertension
- •Suggested Reading
- •Website
- •40: Acute Pancreatitis
- •Suggested Reading
- •Website
- •41: Acute Liver Failure
- •Suggested Reading
- •Suggested Reading
- •Websites
- •43: Nutrition Support
- •Suggested Reading
- •44: Acute Renal Failure
- •Suggested Reading
- •Websites
- •45: Renal Replacement Therapy
- •Suggested Reading
- •Website
- •46: Managing a Patient on Dialysis
- •Suggested Reading
- •Websites
- •47: Drug Dosing
- •Suggested Reading
- •Websites
- •48: General Measures of Infection Control
- •Suggested Reading
- •Websites
- •49: Antibiotic Stewardship
- •Suggested Reading
- •Website
- •50: Septic Shock
- •Suggested Reading
- •51: Severe Tropical Infections
- •Suggested Reading
- •Websites
- •52: New-Onset Fever
- •Suggested Reading
- •Websites
- •53: Fungal Infections
- •Suggested Reading
- •Suggested Reading
- •Website
- •55: Hyponatremia
- •Suggested Reading
- •56: Hypernatremia
- •Suggested Reading
- •57: Hypokalemia and Hyperkalemia
- •57.1 Hyperkalemia
- •Suggested Reading
- •Website
- •58: Arterial Blood Gases
- •Suggested Reading
- •Websites
- •59: Diabetic Emergencies
- •59.1 Hyperglycemic Emergencies
- •59.2 Hypoglycemia
- •Suggested Reading
- •60: Glycemic Control in the ICU
- •Suggested Reading
- •61: Transfusion Practices and Complications
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Website
- •63: Onco-emergencies
- •63.1 Hypercalcemia
- •63.2 ECG Changes in Hypercalcemia
- •63.3 Superior Vena Cava Syndrome
- •63.4 Malignant Spinal Cord Compression
- •Suggested Reading
- •64: General Management of Trauma
- •Suggested Reading
- •65: Severe Head and Spinal Cord Injury
- •Suggested Reading
- •Websites
- •66: Torso Trauma
- •Suggested Reading
- •Websites
- •67: Burn Management
- •Suggested Reading
- •68: General Poisoning Management
- •Suggested Reading
- •69: Syndromic Approach to Poisoning
- •Suggested Reading
- •Websites
- •70: Drug Abuse
- •Suggested Reading
- •71: Snakebite
- •Suggested Reading
- •72: Heat Stroke and Hypothermia
- •72.1 Heat Stroke
- •72.2 Hypothermia
- •Suggested Reading
- •73: Jaundice in Pregnancy
- •Suggested Reading
- •Suggested Reading
- •75: Severe Preeclampsia
- •Suggested Reading
- •76: General Issues in Perioperative Care
- •Suggested Reading
- •Web Site
- •77.1 Cardiac Surgery
- •77.2 Thoracic Surgery
- •77.3 Neurosurgery
- •Suggested Reading
- •78: Initial Assessment and Resuscitation
- •Suggested Reading
- •79: Comprehensive ICU Care
- •Suggested Reading
- •Website
- •80: Quality Control
- •Suggested Reading
- •Websites
- •81: Ethical Principles in End-of-Life Care
- •Suggested Reading
- •82: ICU Organization and Training
- •Suggested Reading
- •Website
- •83: Transportation of Critically Ill Patients
- •83.1 Intrahospital Transport
- •83.2 Interhospital Transport
- •Suggested Reading
- •84: Scoring Systems
- •Suggested Reading
- •Websites
- •85: Mechanical Ventilation
- •Suggested Reading
- •86: Acute Severe Asthma
- •Suggested Reading
- •87: Status Epilepticus
- •Suggested Reading
- •88: Severe Sepsis and Septic Shock
- •Suggested Reading
- •89: Acute Intracranial Hypertension
- •Suggested Reading
- •90: Multiorgan Failure
- •90.1 Concurrent Management of Hepatic Dysfunction
- •Suggested Readings
- •91: Central Line Placement
- •Suggested Reading
- •92: Arterial Catheterization
- •Suggested Reading
- •93: Pulmonary Artery Catheterization
- •Suggested Reading
- •Website
- •Suggested Reading
- •95: Temporary Pacemaker Insertion
- •Suggested Reading
- •96: Percutaneous Tracheostomy
- •Suggested Reading
- •97: Thoracentesis
- •Suggested Reading
- •98: Chest Tube Placement
- •Suggested Reading
- •99: Pericardiocentesis
- •Suggested Reading
- •100: Lumbar Puncture
- •Suggested Reading
- •Website
- •101: Intra-aortic Balloon Pump
- •Suggested Reading
- •Appendices
- •Appendix A
- •Appendix B
- •Common ICU Formulae
- •Appendix C
- •Appendix D: Syllabus for ICU Training
- •Index
General Management of Trauma |
64 |
|
|
Vinay Gulati, Sanjeev Bhoi, and Rajesh Chawla |
|
A 50-year-old male patient hit by a bus about 6 h ago presented to the emergency department. He had a labored breathing; his respiratory rate was 35/min with O2 saturation of 94%. His heart rate was 130/min, blood pressure was 100/80 mmHg, and Glasgow coma score (GCS) was 9/15. After initial stabilization, the secondary survey revealed multiple rib fractures on the right side of the chest and fracture of the right femur.
Trauma is a major cause of death and disability in the first four decades of life. Improvement and organization of trauma care services are a cost-effective way of improving patient outcome. Proper organization of these systems reduces the time between injury and the definitive care, thereby reducing the morbidity and mortality.
Step 1: Preparation
•Alert the trauma team about the arrival of the injured patient.
•Trauma team includes the general/trauma surgeon, the emergency physician, the orthopedic surgeon and/or the ICU/anesthesia specialist on call, and at least two trained nurses and two paramedics.
•Besides the general surgeon, the team leader of the trauma team can be an emergency medicine or ICU/anesthesia specialist who is skilled in airway management.
V. Gulati, M.D. (*) • S. Bhoi, M.D.
Department of Emergency Medicine, J.P.N. Apex Trauma Centre, AIIMS, New Delhi, India e-mail: drvinaygulati@gmail.com
R. Chawla, M.D., F.C.C.M.
Department of Respiratory, Critical Care & Sleep Medicine, Indraprastha Apollo Hospitals, New Delhi, India
e-mail: drchawla@hotmail.com
R. Chawla and S. Todi (eds.), ICU Protocols: A stepwise approach, |
511 |
DOI 10.1007/978-81-322-0535-7_64, © Springer India 2012 |
|
512 |
V. Gulati et al. |
|
|
•Airway cart, crash cart, suction, monitors and IV cannula, warm IV fluids, and other equipment should be rechecked.
•The trauma team members should be ready with universal precautions by putting on mask, splash-resistant and lead gowns, eye protection, and gloves.
•The operating theater personnel should be informed.
Step 2: Triage
•Triage is a process of determining the priority of treatment based on the patient’s airway (A), breathing (B), and circulation (C) as well as availability of resources.
•Triage separates the injured patients into five categories:
1.The injured patient with compromised ABC who needs immediate treatment (red)
2.The injured patient with stable ABC whose treatment can wait (yellow)
3.Those with minor injuries (walking wounded), who need help less urgently (green)
4.The unsalvageable patients who are beyond help (blue or gray)
5.The injured patients who are already dead (black)
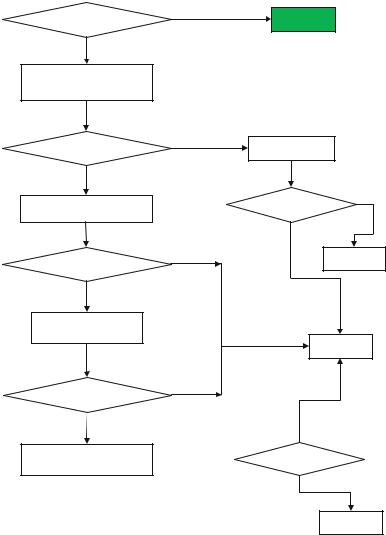
•A simple tool, which can be used for triage, is START (simple triage and rapid treatment) (Figure 1).
Emergency Department Management Protocol
Triage Protocol
Step 3: Primary survey and resuscitation
•The “ABCDE” of primary survey is, in essence, to identify the life-threatening conditions and institution of life-preserving therapies by priority based on their injuries, vital signs, and injury mechanisms.
•Take history from the accompanying person about the following:
–Mechanism of injury
–Injuries suspected
–Vital signs
–Treatment en route to hospital
•The management is concurrent with the assessment, resuscitation, and stabilization.
ABCDE
Airway maintenance with cervical spine control
Breathing and ventilation
Circulation/hemorrhage control
Disability/neurological status
Exposure/environmental control
64 General Management of Trauma |
513 |
|
|
Yes
Victim can walk?
No
Assess breathing without opening the airway
No
Breathing?
Yes
Assess respiratory rate
Yes
> 30 / min?
No
Take pulse at wrist
No
Present?
Yes
Assess level consciousness 
Green
Open airway
No
Breathing?
Yes
Black
Red
No
Responsive
Yes
Yellow
Fig. 64.1 START (simple triage and rapid treatment) algorithm
A-Airway with cervical spine control
•Airway is assessed immediately for patency, protective reflexes, foreign body, secretions, and injury.
•The patency of the airway should be assessed with special attention to foreign body or maxillofacial fractures that may result in airway obstruction.
•Absence of response, stridor, confusion, or a hoarse reply may indicate airway compromise.
514 |
V. Gulati et al. |
|
|
•Chin-lift or jaw-thrust maneuver may be used to achieve airway patency, simultaneously protecting the cervical spine by inline cervical stabilization.
•Head tilt maneuver is avoided in an injured patient while managing airway.
•A definitive airway is required in the following conditions:
–Inadequate ventilation and oxygenation
–Impending or actual airway obstruction secondary to injury
–Brain injury with a GCS of less than 8
–Inability to adequately protect the airway from aspiration
–Severe multisystem injury or hemodynamic instability
–Facial burns or inhalation injury
–Inability to closely monitor during ongoing resuscitation and investigation (e.g., angiography and CT scanning)
–Uncooperative or combative behavior
–An infant or a child unable to cooperate with investigations
•Cervical spine protection (by application of cervical collar) during airway maneuvers should be done in all trauma patients unless specifically cleared.
•Rapid-sequence intubation protocol should be followed for securing airway.
Unstable adult patient
1–2 mg/kg ketamine with 1–2 mg/kg IV succinylcholine
Adult head injury with normal pulse/BP
GCS of 3—intubate without drugs
GCS more than 4—0.3 mg/kg—etomidate with 1–2 mg/kg IV succinylcholine
Pediatric rapid-sequence intubation
With hypovolemia—0.1 mg/kg IV midazolam
With normovolemia—0.3 mg/kg IV midazolam
•Difficult or failed intubations
–Call anesthesiologist or a more experienced person.
–Anticipate airway problems with the following:
•The decreased level of consciousness
•Head trauma
•Facial trauma
•Neck trauma
•Upper thorax trauma
•Severe burns to any of these areas
Airway – management options with cervical spine control treatment include:
O2 administration
Basic airway maneuvers: chin lift and jaw thrust
Oropharyngeal or nasopharyngeal airway, but caution in bleeding patient
Endotracheal intubation
Surgical airway, that is, cricothyroidotomy/tracheostomy
64 General Management of Trauma |
515 |
|
|
B-Breathing and ventilation
•Chest wall mechanics are altered due to rib fracture and pulmonary contusions.
•Breathing is assessed by determining the patient’s respiratory rate and by subjectively quantifying the depth and effort of inspiration.
•The patient’s chest should be exposed to adequately assess chest wall excursion.
•Visual inspection and palpation to detect chest wall injuries, percussion for hyperresonance or dullness to exclude air or blood respectively in the chest, and auscultation to detect adequate air entry in lungs should be carried out.
•Rapid respiratory effort, use of accessory muscles of respiration, hypoxia, hypercapnia, asymmetric chest wall excursions, and diminished or absent breath sounds will require treatment before proceeding further.
•Specific life-threatening problems that should be identified immediately and addressed during the primary survey are the following:
–Tension pneumothorax
–Open pneumothorax
–Massive hemothorax
–Flail chest
–Cardiac tamponade
Breathing – treatment options include:
Endotracheal intubation and ventilation
Needle decompression
Intercostal tube drain
Pericardial drainage
Thoracotomy
Adequate analgesia
C-Circulation with hemorrhage control
•Hypotension in a trauma patient is always assumed to result from significant hemorrhage (>30% blood loss) unless proved otherwise.
•Hemorrhage is the primary cause of shock in trauma patients.
•Rapid and accurate assessment of the patient’s hemodynamic status and identification of the site of hemorrhage is therefore essential.
•It is critical to establish two large-bore short-length intravenous cannulas (16G or bigger) in a trauma patient, preferably in the upper extremities, and resuscitation should be started with warm crystalloids (Ringer’s lactate). The blood transfusion should be done in patients with ongoing hemodynamic instability after initial fluid boluses. The three body regions, which hide significant amounts of blood in cases of blunt injury, include the chest, abdomen, and pelvis.
•Chest and pelvic radiographs and a focused assessment by sonography in trauma (FAST) or a diagnostic peritoneal lavage (DPL) are mandatory screening studies for patients in shock.

516 |
V. Gulati et al. |
|
|
•Hemorrhage control by direct application of external pressure and/or careful application of tourniquet may be done in all patients.
•Pelvic ring should be closed using pelvic binders if the bleeding is suspected from an unstable pelvis.
•Fractured long bones are reduced, and traction splint is applied if they are possible source of bleeding to decrease ongoing blood loss and pain as well as to prevent further local injury.
Circulation and hemorrhage control – treatment options include:
Warm fluids (crystalloid—Ringer’s lactate)
Warm blood and blood products (e.g., fresh frozen plasma)
Arrest bleeding by direct local pressure
Arrest bleeding by splinting pelvis
Central line if inotropes/vasopressors are needed
Urinary catheter
Surgery—laparotomy, thoracotomy, and/or pelvic fracture fixation (damage control or definitive) may be undertaken to control bleeding
D-Disability/neurological status
•A rapid neurological evaluation is carried out at the end of primary survey only after the resuscitation and stabilization have been achieved as mentioned above.
•This assesses the patient’s level of consciousness, pupillary size and reaction, and focal neurological deficit.
•The level of consciousness may be described in terms of the GCS.
•The GCS is used as a baseline determination of neurological function, and frequent reassessment is required to detect an early or previously missed injury.
•A complete neurological examination is not appropriate at this time and should be performed during secondary survey.
Disability – treatment options include:
O2 administration
Intubation (to ensure normal PO2 and PCO2)
Avoid hypotension and hypoxia to prevent secondary brain damage
Inotropes/vasopressors (to ensure adequate cerebral perfusion)
Head up, ensure venous drainage
Emergency imaging of the brain or spine
Early neurosurgical consultation
E-Exposure/environmental control
•The patient should be completely undressed to facilitate thorough examination and assessment in front and back.
•At the same time, care should be taken to prevent hypothermia.
– Remove wet or blood-soaked clothes, and warm IV fluids (39°C).
64 General Management of Trauma |
517 |
|
|
–Use blood warmers for transfusing and external warming (warmed blankets to all patients and forced, heated air, or radiant warmers as needed) to prevent hypothermia.
Step 4: Adjuncts to primary survey and resuscitation
(a)ECG monitoring
•The appearance of dysrhythmias may indicate blunt cardiac injury.
•Pulseless electrical activity, the presence of cardiac rhythm without peripheral pulse, may indicate cardiac tamponade, tension pneumothorax, or profound hypovolemia.
(b)Urinary catheter
•Urine output is a sensitive indicator of the volume status of the patient and reflects renal perfusion.
•All trauma victims should be catheterized to enable monitoring of the urine output and to plan intravenous fluid therapy.
•Transurethral catheterization is contraindicated in patients whom urethral transaction is suspected.
(c)Gastric catheter
•A naso/orogastric (in skull base fracture) tube is indicated to reduce stomach distension and decrease the risk of aspiration.
(d)X-rays and diagnostic studies
•The chest and pelvis X-rays help in the assessment of a trauma patient.
•The blood should be sent for crossmatching and arranging for packed cells, and important diagnostic parameters such as hemoglobin, coagulation profile, renal parameters, electrolytes, random blood sugar, and arterial blood gas (ABG) should be checked.
•Pulse oximetry is a valuable adjunct for monitoring oxygenation and adequacy of peripheral circulation in injured patients.
(e)FAST(focused assessment with sonography for trauma)
The FAST is a rapid, bedside, ultrasound examination performed to identify intraperitoneal hemorrhage or pericardial tamponade. FAST examines four areas for free fluid: perihepatic and hepatorenal space, perisplenic, pelvis, and pericardium
Step 5: Consideration for interhospital transfer
•Identify the early, potential need for transfer of the polytrauma patient to an institution where definitive care can be undertaken.
•Transfer decision should be on the basis of known injuries and patterns of injury.
•An effective communication including the condition of the patient, treatment given, and anticipated requirements during transfer should be made to the receiving hospital.
•The transfer to another center should not be delayed for the want of investigations.
518 |
V. Gulati et al. |
|
|
Step 6: Admit in ICU
•Airway protection and mechanical ventilation
•Cardiovascular resuscitation
•Severe head injury
•Organ support
•Correct coagulopathy
•Invasive monitoring
•Active rewarming of hypothermic patients
Step 7: Secondary survey
•Once the primary survey is accomplished—life-threatening conditions are managed and resuscitative efforts are underway—secondary survey is carried out.
•This is a head-to-toe evaluation of the trauma patient, which includes a complete history and physical examination and reassessment of all the vital signs.
•History includes the following:
A—Allergies
M—Medications currently taken
P—Past illness/pregnancy
L—Last meal
E—Events/environment related to the injury
•Each region of the body is completely examined.
•The care should be continued with regular reevaluation of the patient for any deterioration and new findings so that appropriate measures can be taken.
Reevaluation
•After the completion of the secondary survey, the patient should be reevaluated beginning with the ABCs and thorough physical examination and examined for any missed injury (tertiary survey) such as fractures.
•Constant monitoring of the severely injured patient is required and may necessitate rapid transfer to the surgical intensive care unit, operating room, or to another center having better specialized facilities.
•Appropriate referral for specialists should be sent.
•Adequate pain relief, tetanus prophylaxis, and antibiotic should be given.
•Specific care should be taken to examine the possible missed injuries on the following:
Back of the head and the scalp
The neck, beneath semirigid collar
Back, buttocks, and flanks
Groin creases, perineum, and genitalia
