
- •Preface
- •Foreword
- •Contents
- •Contributors
- •1. Medical History
- •1.1 Congestive Heart Failure
- •1.2 Angina Pectoris
- •1.3 Myocardial Infarction
- •1.4 Rheumatic Heart Disease
- •1.5 Heart Murmur
- •1.6 Congenital Heart Disease
- •1.7 Cardiac Arrhythmia
- •1.8 Prosthetic Heart Valve
- •1.9 Surgically Corrected Heart Disease
- •1.10 Heart Pacemaker
- •1.11 Hypertension
- •1.12 Orthostatic Hypotension
- •1.13 Cerebrovascular Accident
- •1.14 Anemia and Other Blood Diseases
- •1.15 Leukemia
- •1.16 Hemorrhagic Diatheses
- •1.17 Patients Receiving Anticoagulants
- •1.18 Hyperthyroidism
- •1.19 Diabetes Mellitus
- •1.20 Renal Disease
- •1.21 Patients Receiving Corticosteroids
- •1.22 Cushing’s Syndrome
- •1.23 Asthma
- •1.24 Tuberculosis
- •1.25 Infectious Diseases (Hepatitis B, C, and AIDS)
- •1.26 Epilepsy
- •1.27 Diseases of the Skeletal System
- •1.28 Radiotherapy Patients
- •1.29 Allergy
- •1.30 Fainting
- •1.31 Pregnancy
- •Bibliography
- •2.1 Radiographic Assessment
- •2.2 Magnification Technique
- •2.4 Tube Shift Principle
- •2.5 Vertical Transversal Tomography of the Jaw
- •Bibliography
- •3. Principles of Surgery
- •3.1 Sterilization of Instruments
- •3.2 Preparation of Patient
- •3.3 Preparation of Surgeon
- •3.4 Surgical Incisions and Flaps
- •3.5 Types of Flaps
- •3.6 Reflection of the Mucoperiosteum
- •3.7 Suturing
- •Bibliography
- •4.1 Surgical Unit and Handpiece
- •4.2 Bone Burs
- •4.3 Scalpel (Handle and Blade)
- •4.4 Periosteal Elevator
- •4.5 Hemostats
- •4.6 Surgical – Anatomic Forceps
- •4.7 Rongeur Forceps
- •4.8 Bone File
- •4.9 Chisel and Mallet
- •4.10 Needle Holders
- •4.11 Scissors
- •4.12 Towel Clamps
- •4.13 Retractors
- •4.14 Bite Blocks and Mouth Props
- •4.15 Surgical Suction
- •4.16 Irrigation Instruments
- •4.17 Electrosurgical Unit
- •4.18 Binocular Loupes with Light Source
- •4.19 Extraction Forceps
- •4.20 Elevators
- •4.21 Other Types of Elevators
- •4.22 Special Instrument for Removal of Roots
- •4.23 Periapical Curettes
- •4.24 Desmotomes
- •4.25 Sets of Necessary Instruments
- •4.26 Sutures
- •4.27 Needles
- •4.28 Local Hemostatic Drugs
- •4.30 Materials for Tissue Regeneration
- •Bibliography
- •5. Simple Tooth Extraction
- •5.1 Patient Position
- •5.2 Separation of Tooth from Soft Tissues
- •5.3 Extraction Technique Using Tooth Forceps
- •5.4 Extraction Technique Using Root Tip Forceps
- •5.5 Extraction Technique Using Elevator
- •5.6 Postextraction Care of Tooth Socket
- •5.7 Postoperative Instructions
- •Bibliography
- •6. Surgical Tooth Extraction
- •6.1 Indications
- •6.2 Contraindications
- •6.3 Steps of Surgical Extraction
- •6.4 Surgical Extraction of Teeth with Intact Crown
- •6.5 Surgical Extraction of Roots
- •6.6 Surgical Extraction of Root Tips
- •Bibliography
- •7.1 Medical History
- •7.2 Clinical Examination
- •7.3 Radiographic Examination
- •7.4 Indications for Extraction
- •7.5 Appropriate Timing for Removal of Impacted Teeth
- •7.6 Steps of Surgical Procedure
- •7.7 Extraction of Impacted Mandibular Teeth
- •7.8 Extraction of Impacted Maxillary Teeth
- •7.9 Exposure of Impacted Teeth for Orthodontic Treatment
- •Bibliography
- •8.1 Perioperative Complications
- •8.2 Postoperative Complications
- •Bibliography
- •9. Odontogenic Infections
- •9.1 Infections of the Orofacial Region
- •Bibliography
- •10. Preprosthetic Surgery
- •10.1 Hard Tissue Lesions or Abnormalities
- •10.2 Soft Tissue Lesions or Abnormalities
- •Bibliography
- •11.1 Principles for Successful Outcome of Biopsy
- •11.2 Instruments and Materials
- •11.3 Excisional Biopsy
- •11.4 Incisional Biopsy
- •11.5 Aspiration Biopsy
- •11.6 Specimen Care
- •11.7 Exfoliative Cytology
- •11.8 Tolouidine Blue Staining
- •Bibliography
- •12.1 Clinical Presentation
- •12.2 Radiographic Examination
- •12.3 Aspiration of Contents of Cystic Sac
- •12.4 Surgical Technique
- •Bibliography
- •13. Apicoectomy
- •13.1 Indications
- •13.2 Contraindications
- •13.3 Armamentarium
- •13.4 Surgical Technique
- •13.5 Complications
- •Bibliography
- •14.1 Removal of Sialolith from Duct of Submandibular Gland
- •14.2 Removal of Mucus Cysts
- •Bibliography
- •15. Osseointegrated Implants
- •15.1 Indications
- •15.2 Contraindications
- •15.3 Instruments
- •15.4 Surgical Procedure
- •15.5 Complications
- •15.6 Bone Augmentation Procedures
- •Bibliography
- •16.1 Treatment of Odontogenic Infections
- •16.2 Prophylactic Use of Antibiotics
- •16.3 Osteomyelitis
- •16.4 Actinomycosis
- •Bibliography
- •Subject Index

70 |
F. D. Fragiskos |
Fig. 4.72. Clinical photograph showing closure of the operative field with surgical dressing
4.30
Materials for Tissue Regeneration
Sometimes during surgical procedures (removal of cysts, extraction of impacted teeth, etc.) large bony defects are created, which cause problems associated with esthetics, function, and the healing process, or they may even affect the stability of the jaw bone. Recently, application of a variety of materials in oral surgery to the area around these bony defects aids bone regeneration and eliminates the defect or limits its size. These materials may also prove useful in the regeneration of periodontal tissues, for the filling of bone defects around an implant, or for augmentation of a deficient alveolar ridge, etc. The most commonly used such materials are membranes and bone grafts.
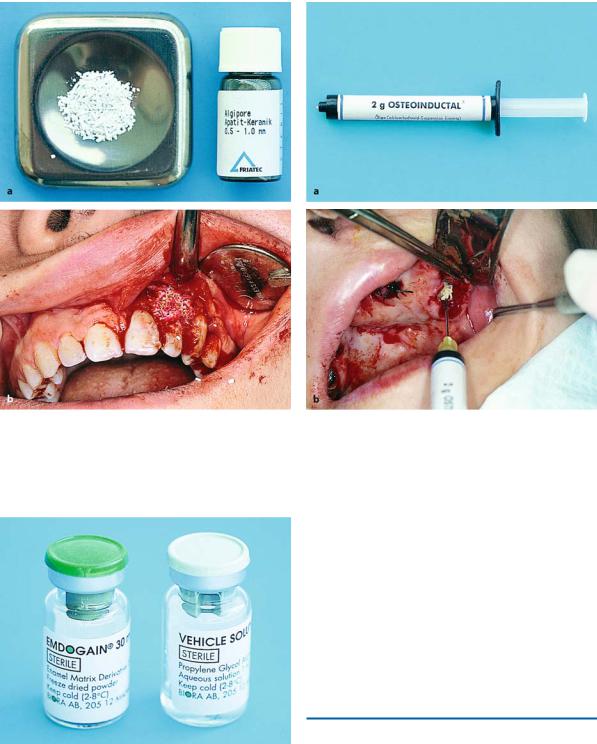
Membranes. These may be absorbable or nonabsorbable. Synthetic polymer and collagen membranes are absorbable (Fig. 4.73a). Nonabsorbable membranes include those reinforced with titanium, as well as metallic titanium network membranes. The main disadvantage of nonabsorbable membranes is the need to perform a second surgical procedure for their removal.
Bone Grafts. These belong to four categories:
Fig. 4.73 a, b. a Absorbable collagen membrane used for guided bone regeneration. b Clinical photograph showing stabilization of the membrane in an area of bone deficit after surgical extraction
Fig. 4.74 a, b. Heterografts of bovine bone (Bio-Oss) for the regeneration of large osseous defects; a in compact form, and b in granules
1.Autografts, which are composed of tissues from the actual patient.
2.Allografts, which are composed of tissues from an- 4. Alloplastic grafts, which are composed of synthetic
other individual.
3.Heterografts, which are composed of tissues from various animals (Fig. 4.74).
bone substitutes, e.g., hydroxylapatite (Fig. 4.75), phosphoric calcium ceramics, and oily calcium hydroxide in cream form (Fig. 4.76).
Chapter 4 Equipment, Instruments, and Materials |
71 |
Fig. 4.75 a, b. a Synthetic bone substitute (hydroxylapatite) in granules. b Clinical photograph of transplantation of lateral incisor of the maxilla. The area of osseous defect is filled with hydroxylapatite
Fig. 4.77. Amelogenin (base and catalyst) used for tissue regeneration
Fig. 4.76 a, b. a Oily calcium hydroxide in cream form used for bone regeneration. b Postextraction socket with buccal loss of bone. The area is filled with synthetic material
Other materials that contain amelogenin as the active ingredient, amelogenin being one of the proteins associated with tooth enamel (Fig. 4.77), may also promote tissue regeneration.
Of all the grafts, bone autografts give the best results. In spite of that, their use of limited, because a second concurrent surgical procedure is required. For this reason, the aforementioned synthetic substitute materials are used today instead, and bone regeneration in areas with large bone defects is accomplished satisfactorily.
Bibliography
Abbas F, Wennstrom J, Van der Weijen F, Schneiders T, Van der Velden U (2003) Surgical treatment of gingival recessions using emdogain gel: clinical procedure and case reports. Int J Periodontics Restorative Dent 23(6):607–613
AESCULAP Dental Catalogue (1990)
Council on Dental Materials, Instruments and Equipment (1991) Sterilization required for infection control. J Am Dent Assoc 122:80

72 F. D. Fragiskos
Dahlin C, Sennerby L, Lekholm U, Linde A, Nyman S (1989) Generation of new bone around titanium implants using a membrane technique: an experimental study in rabbits. Int J Oral Maxillofac Implants 4:19–25
Findlay IA (1960) The classification of dental elevators. Br Dent J 109:219–223
Gans BJ (1972) Atlas of oral surgery. Mosby, St. Louis, Mo. Heijl L, Heden G, Svardstrom G, Ostgren A (1997) Enamel
matrix derivative (EMDOGAIN®) in the treatment of intrabony periodontal defects. J Clin Periodont 24:705– 714
Howe GL (1997) Minor oral surgery, 3rd edn. Wright, Oxford
Kandler HJ (1982) The design and construction of dental elevators. J Dent 10:317–322
Klinge B, Alberius P, Isaksson S, Jonsson J (1992) Osseous response to implanted natural bone mineral and synthetic hydroxylapatite ceramic in the repair of experimental skull bone defects. J Oral Maxillofac Surg 50:241
Koerner KR (1994) The removal of impacted third molars. Principles and procedures. Dent Clin North Am 38:255– 278
Kruger GO (1984) Oral and maxillofacial surgery, 6th edn. Mosby, St. Louis, Mo.
Laskin DM (1980) Oral and maxillofacial surgery, vol 1. Mosby, St. Louis, Mo.
Laskin DM (1985) Oral and maxillofacial surgery, vol 2. Mosby, St. Louis, Mo.
Lilly GE, Salem JE, Armstrong JH, Cutcher JL (1969) Reaction of oral tissues to suture materials. Part III. Oral Surg Oral Med Oral Pathol 28:432–438
Macht SD, Krizek TJ (1978) Sutures and suturing – current concepts. J Oral Surg 36:710–712
Parisis N, Tsirlis A, Lavrentiadis I, Iakovidis D (1998) Surgical treatment of bone deficits with heterografts and absorbable membranes. Hell Period Stomat Gnathoprosopike Cheir 13:7–15
Pepelasi E, Vrotsos I (1992) Use of bone grafts in treatment of periodontal bone lesions. Odontostomatologike Proodos 46:285–296
Peterson LJ, Ellis E III, Hupp JR, Tucker MR (1993) Contemporary oral and maxillofacial surgery, 2nd edn. Mosby, St. Louis, Mo.
Rosenberg E, Rose LF (1998) Biologic and clinical considerations for autografts and allografts in periodontal regeneration therapy. Dent Clin North Am 42(3):467–490
Sailer HF, Pajarola GF (1999) Oral surgery for the general dentist. Thieme, Stuttgart
Schenk RK, Buser D, Hardwick WR, Dahlin C (1994) Healing pattern of bone regeneration in membrane-protected defects: a histologic study in the canine mandible. Int J Oral Maxillofac Implants 9:13–29
Tinti C, Vincenzi G, Cocchetto R (1993) Guided tissue regeneration in mucogingival surgery. J Periodontol 64:1184–1191
Waite DE (1987) Textbook of practical oral and maxillofacial surgery, 3rd edn. Lea and Febiger, Philadelphia, Pa.
Weingart D, Schilli W (1997) Surgical techniques for prevention of sinking of membrane using guided tissue regeneration. Implantology 4:307–319
